B
Backscattered electron (BSE) imaging High-resolution imaging of a surface using electronics, similar to how a light microscope uses visible light. The advantages of BSE over light microscopy include greater magnification and much greater depth of field. This method is most commonly performed via application of accelerating voltages of 10 kV or more to the specimen while detecting high-energy electrons that backscatter quasi-elastically off the sample. For imaging of surface detail, the application of a lower-accelerating voltage results in less beam penetration, spread, and overall specimen damage.
Bacterial collagenase Any of various collagenases purified from a variety of microbes; they preferentially cleave collagen on the N-terminal side of glycine residues and occur in several classes of differing specificity. Bacterial collagenases are used in tissue disruption for cell harvesting.
Bacterial leakage Colonization and release of bacteria at the interface of an oral implant abutment and implant.1
Bacterium (pl: bacteria) Member of a group of ubiquitous, single-celled microorganisms that have a prokaryotic (primitive) cell type. Many of these are etiologic in diseases that affect all life forms, including humans and other animals. See also: Actinobacillus actino-mycetemcomitans; Fusobacterium nucleatum.
BAHA Abbreviation for Bone-anchored hearing aid.
Balanced occlusion Existing or developed simultaneous harmonious occlusal contact of the teeth throughout the dental arch during mandibular centric and eccentric movements; especially important for removable complete dentures to achieve stability during function.2,3 See also: Articulation.
Ball attachment system Specific design of a mechanical attachment in which the patrix fits into the matrix in a ball-and-socket type of relation. Each element is incorporated into either the natural tooth as part of a restoration or as an abutment on the implant with the reciprocal element incorporated into the prosthesis. The patrix, or ball, can be made of plastic or metal alloy of various diameters and with varied amounts of resistance.4
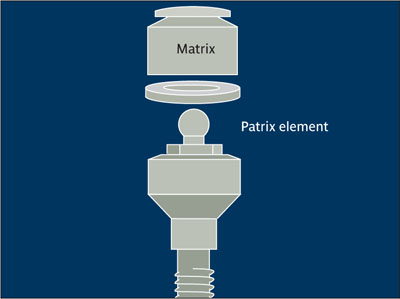
Ball attachment system.
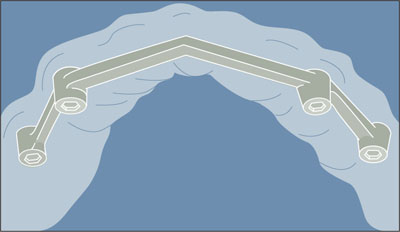
Bar Round, half-round, or elliptically shaped metallic segment with greater length than width. A bar is commonly used to connect components of a prosthesis such as abutments, crowns, or parts of a removable partial denture. It also can be used to provide support, stability, and/or retention for a prosthesis.23 See also: Dolder bar; Hader bar.
Bar attachment system Specific design of an attachment in which the patrix spans a specified width that the matrix matches. Each element is part of a prosthetic structure that spans two or more natural teeth and/or implants and is fixed intraorally with the matrix, which is incorporated within the prosthesis. Once the components are engaged by riders, clips, or microplungers, there is resistance to displacement through either a mechanical mechanism or frictional fit.5
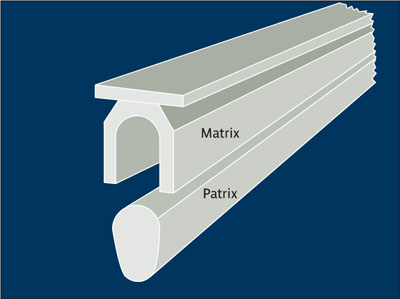
Bar attachment system (in cross section).
Four implants with b. a. s. Mechanical attachment incorporated into and fabricated as part of a prosthesis mesostructure supported by four implants.
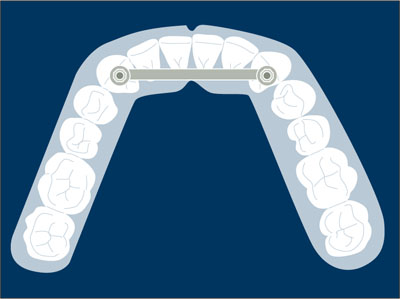
Four implants with bar attachment system.
Two-implant overdenture with b. a. s. Mechanical attachment incorporated into and fabricated as part of a prosthesis mesostructure supported by two implants.
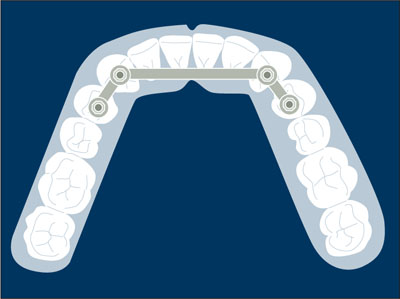
Two-implant overdenture with bar attachment system.
Bar clip retention See: Clip bar overdenture; Retainer; Retention.
Bar overdenture (implant) See: Clip bar overdenture.
Bar splint Connecting bar for adding rigidity and/or stability between teeth or implants. It is also used to fixate displaced or movable body parts as a result of trauma or surgery.2 See also: Splinting.
Bar splint.
Barium sulfate Alkaline earth metal (BaSO4). Barium is derived from the Greek word barys, meaning heavy and is generally a toxic substance in water-soluble compounds. Barium sulfate, however, is insoluble in water, and because it is even insoluble in hydrochloric acid, it can be used as a medical contrast medium to examine the gastrointestinal tract.
Barrier membrane Used in guided bone regeneration (GBR) to locally augment deficient sites in implant patients. By creating a secluded space, the barrier prevents epithelial cells and fibroblasts from proliferating into the augmentation site, whereas the slower-growing angiogenic and osteogenic cells have exclusive access to the membrane-protected space. The first membranes were made of bio-inert expanded polytetrafluoroethylene (e-PTFE), which is nonresorbable and therefore required removal with a second surgical procedure. Bioresorbable membranes, either of synthetic polymers or of animal-derived collagen, are often preferred in daily practice. Although their barrier function is limited in time, they do not require a second surgical procedure for membrane removal. Barrier membranes exclude undesirable cell types from entering the secluded area of the bony or periodontal defect during healing. Membrane configurations are designed for specific applications; vary in shape, size, and thickness. See also: Guided bone regeneration (GBR); Guided tissue regeneration (GTR); Collagen membrane; Expanded polytetrafluoroethylene (e-PTFE) membrane.

Barrier membranes specially designed for treatment of recession defects. (left Nonresorbable titanium-reinforced expanded polytetrafluorethylene (e-PTFE) membrane; right Bioresorbable polylactic acid and citric acid ester-based membrane.)
(Reprinted from Lindhe et al6 with permission.)
Basal bone Supporting bone in the mandible that underlies and is continuous with the alveolar process and houses the major nerves and vessels. It also functions as a site of muscle attachment and is resistant to resorption.7
Basic fibroblast growth factor (bFGF) See: Fibroblast growth factor (FGF).
Basic multicellular unit (BMU) Fully developed cortical bone remodeling unit comprising an elongated cylindrical structure about 2 mm long and 0.2 mm wide, which travels through bone in a controlled direction. The BMU preserves its size, shape, and internal organization for many months. Maintenance of this unique entity requires continued recruitment of new osteoclasts and osteoblasts in appropriate numbers and the growth of new blood vessels, nerves, and connective tissue.The end result of each new BMU is one new Haversian system or osteon.
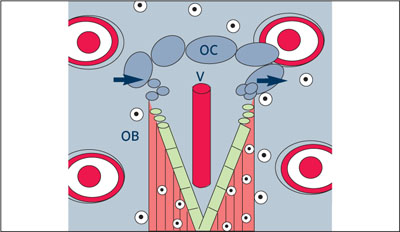
Basic multicellular unit (BMU).
A BMU contains osteoclasts OC, as well as vascular structures V and osteoblasts OB.
(Redrawn from Lang et al8 with permission.)
B cell White blood cell derived from bone marrow. As part of the immune system, B cells (or bursa-equivalent cells) may differentiate and become antibody-producing plasma cells. Called also B lymphocyte.
Bending moment Rotary effect of a force potentially causing deformation through torque.
Bennett movement Translatory or bodily side shift of the mandible that occurs with lateral mandibular movement. During lateral mandibular movement, as the advancing condyle path intersects with the sagittal plane, an angle known as the Bennett angle is formed.3 (See figure next page)
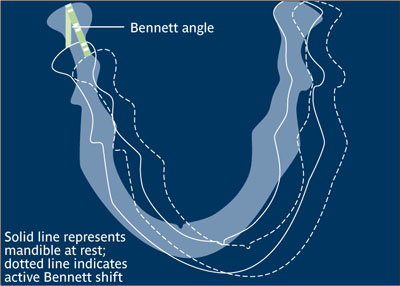
Bennett movement.
(Redrawn from Sharry9 with permission.)
Beveled incision Technique by which incisions are made at an acute angle (less than 90 degrees) to the gingival or mucosal surface, rather than perpendicularly.
bFGF Abbreviation for Basic fibroblast growth factor. See: Fibroblast growth factor (FGF).
BIC Abbreviation for Bone-implant contact.
Bicortical implant anchorage See: Bicortical stabilization.
Bicortical stabilization Practice of engaging both the superior and inferior cortices of bone at the time of implant placement. For an edentulous anterior mandible, the tip of the implant engages the inferior cortex while the neck of the implant engages the superior cortex to maximize initial stability of the implant.
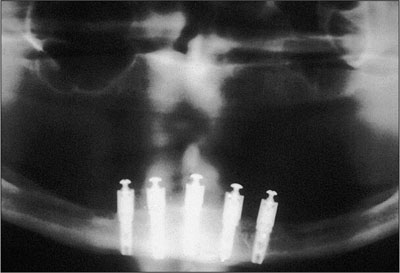
Bicortical stabilization. (Courtesy of T. D. Taylor.)
Bidirectional crest distraction Distraction approach designed to overcome the inherent difficulty in controlling the distraction vector in conventional, unidirectional devices. An additional inclination rod allows for buccaloral (lingual) distraction in addition to vertical distraction.10
Bilateral stabilization See: Cross-arch stabilization.
Bioabsorbable material Solid polymeric material that can dissolve in body fluids without any change of the polymer or decrease in molecular mass.
Bioactive glass Ceramic material that stimulates or otherwise promotes biologic activity. It consists of silicophosphate chains that bond ionically to compounds such as CaO, CaF2, Na2O, ZnO, TiO2 and NiO, among others. It may undergo ionic translocations in vivo, or exchange ions or molecular groups in an osseous recipient site, and thereby osseointegrate. Bioactive glass may be resorbable and is useful as a delivery system in bone engineering. See also: Ceramic.
Bioactivity Effect of implant material that allows interaction and bond formation with living tissues. Implant bioactivity may depend upon material composition, topography, and chemical or physical surface variations.
Bioadhesion Result of a process whereby a chemical attachment between biologic and other materials is obtained.
Bio-Col technique Technique developed to preserve the ridge in the esthetic zone. A tooth is extracted via a low-trauma technique to maintain intact bony walls and surrounding gingival anatomy without flap reflection. The extraction socket is grafted up to the alveolar crest with an anorganic bovine bone substitute, covered with a collagen plug, and sutured in place with a horizontal mattress suture. A removable or fixed provisional restoration with an ovate pontic extending 3 to 4 mm subgingivally is placed, compressing the collagen plug and supporting the surrounding soft tissue. This technique has also been described in combination with immediate implant placement and with a buccal defect, whereby the defect is first lined with a collagen membrane.11
Biocompatibility Condition whereby the body does not respond to a foreign substance (eg, metal) but recognizes it immunologically as self. Biocompatible materials do not lead to acute or chronic inflammatory responses nor do they prevent proper differentiation of implant-surrounding tissues.
Biocompatible Capable of existing together; acceptable to the body. This term is used to describe blood, organs, or tissue that can be transplanted or transfused into a patient’s body without being rejected. It describes a bio-dynamic process in which a material neither elicits an immune response nor is rejected by the host.12,13
Biodegradable material Solid polymeric material that breaks down because of macro-molecular degradation with dispersion in vivo; no proof for elimination from the body.
Bioengineering Use of engineering in biomedical technology such as the movement analysis of body parts or prostheses. See also: Tissue engineering.
Bioerodible material Solid polymeric material that shows surface degradation and resorbs in vivo; reflects total elimination of the foreign material.
Biofilm
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


