Oral and Maxillofacial Infections
Ludwig’s Angina
PMHX/PDHX/Medications/Allergies/SH/FH
This patient is otherwise healthy. (Diabetes mellitus and other immunocompromised states are risk factors for poor outcome and death [see Complications]).
Examination
Airway. The airway is stable on examination. The trachea is difficult to palpate due to edema but appears to be in the midline. Fiberoptic nasopharyngoscopy can be performed to further evaluate the patency of the upper airway and the amount of edema of the surrounding soft tissue (see Emergent Surgical Airway in Chapter 3). Alternatively, computed tomography (CT) scans of the neck can delineate neck and airway swelling.
Maxillofacial. There is obvious moderate to severe facial swelling over the lower third of the face. Brawny and painful induration of the submandibular and submental spaces is noted bilaterally (Figure 4-1). There is erythema over the anterior neck extending down to the clavicles. However, subcutaneous crepitus (indicative of subcutaneous air from gas-producing organisms) is not present. No cervical lymphadenopathy or fluctuance was palpated (lymphadenopathy would be difficult to assess in the presence of neck edema or induration).
Imaging
In the current patient, the panoramic radiograph revealed a carious right mandibular third molar with a large periapical radiolucent lesion. The CT scan of the patient’s neck revealed a rim-enhancing fluid collection involving the bilateral submandibular, submental, and right sublingual spaces (Figure 4-2). In addition, there was diffuse soft tissue edema consistent with cellulitis in the involved spaces. No subcutaneous emphysema was seen in the cervical tissues (subcutaneous gas collection is considered a hallmark of cervical necrotizing fasciitis and is seen in up to 46% to 67% of cases). The patient’s airway was patent and midline. A chest CT was ordered due to the erythema tracking down the anterior neck. No mediastinal involvement was observed.
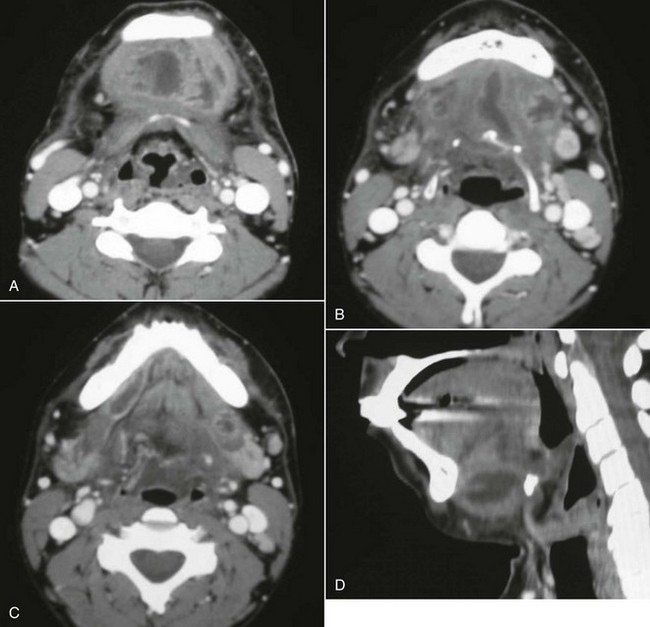
Figure 4-2 A, Axial view, soft tissue CT neck scan with contrast, showing an enhancing fluid collection in the submental space. B, Axial view, soft tissue CT neck scan with contrast, showing enhancing fluid collections in the submental and bilateral submandibular spaces. C, Axial view, soft tissue CT neck scan with contrast, showing an enhancing fluid collection in the right sublingual space. Note that Wharton’s duct, seen on this view, confirms that this abscess is above the mylohyoid muscle. D, Sagittal reconstruction, soft tissue CT neck scan with contrast, showing a large submandibular space abscess extending from the inferior border of the anterior mandible to the hyoid bone.
Treatment
Treatment begins with evaluation of the patient’s airway and appropriate management to prevent acute airway embarrassment (see Emergent Surgical Airway in Chapter 3). The airway is first evaluated by the general appearance of the patient (a distressed patient with stridorous respirations is assumed to have an airway compromise until proved otherwise). The oral cavity should be examined to evaluate the amount of tongue, floor of the mouth, soft palate, and pharyngeal wall edema (many times an oral examination is very limited due to the patient’s inability to open). A fiberoptic nasopharyngoscopy can be performed in the emergency department to further assess the airway, including the vocal cords. Intravenous dexamethasone can be given to reduce the airway edema in patients with impending upper respiratory obstruction. An emergent cricothyroidotomy should be performed if the patient loses the airway before arrival in the operating room. An awake tracheotomy or an awake fiberoptic nasal intubation can be performed in the operating room if the situation is less acute (oral intubation by direct laryngoscopy may also be possible in less severe cases). There is support in the current literature for the assumption that a tracheotomy may be indicated in patients with Ludwig’s angina (see Complications).
Empiric antimicrobial therapy should be promptly initiated to cover the mixed aerobic-anaerobic polymicrobial organisms (gram positive, gram negative, aerobic, and anaerobic) commonly involved in these infections. Penicillin G at an adult dose of 4 million to 30 million units per day, divided and given every 4 to 6 hours, in combination with metronidazole, is an appropriate regimen. Other recommendations include clindamycin 900 mg given intravenously every 8 hours; ticarcillin clavulanate 3.1 g given intravenously every 6 hours; ampicillin sulbactam 3 g given intravenously every 6 hours; and piperacillin tazobactam 3.375 g given intravenously every 6 hours. Chow in 1992 recommended high-dose intravenous penicillin G combined with clindamycin, metronidazole, or cefoxitin. When available, the antibiotic regimen should be guided by cultures and sensitivity studies. The CRP has been shown to be an excellent marker for the severity of the infection and the patient’s response to surgical and antibiotic therapy.
Complications
The most feared complication associated with Ludwig’s angina is death due to airway compromise. Loss of airway from upper airway obstruction can occur at any time during the perioperative period, before arrival at the operating room, during an attempted intubation, after an accidental or self-extubation in the intensive care unit (ICU), or after a planned extubation (see Emergent Surgical Airway in Chapter 3). Potter and colleagues in 2002 reported a 3% incidence of loss of airway for patients who received a tracheotomy versus 6% for patients maintained with endotracheal intubation. They reported two deaths (4% mortality rate) secondary to loss of airway, and both deaths occurred in the endotracheal intubation group (one occurred after a planned extubation and the other occurred after an unplanned extubation). The tracheotomy group had shorter ICU stay (1.1 versus 3.1 days) and shorter overall hospital stay (4.9 versus 5.9 days). Patients with Ludwig’s angina or a retropharyngeal space abscess have a significant need for tracheotomy. Har-El et al’s review of 110 patients showed that 4 of 8 patients meeting their criteria for severe infection who did not receive a tracheostomy developed upper airway obstruction necessitating an emergent surgical airway (50% incidence of airway loss in the endotracheal intubation group). They concluded that tracheotomy is indicated in patients with Ludwig’s angina. In 1985, Loughnan and Allen reported successful endotracheal intubation in 9 of 10 patients with Ludwig’s angina using an inhalational induction technique and direct laryngoscopy, but they did not report on the postoperative morbidity and mortality. If postoperative endotracheal intubation is planned, adequate sedation, four-point restraints, and a secured tube (taped around the head or wired to the teeth) are paramount to prevent unanticipated self or iatrogenic extubation. Upon extubation, a cuff leak test should be performed and an Eschmann tube should be left in place to facilitate reintubation if needed (postextubation laryngeal edema may cause loss of airway despite having a good cuff leak test result).
Before the advent of antibiotics, the mortality rate from Ludwig’s angina was greater than 50%. Fortunately, the prevalence and mortality rates have significantly decreased due to better access to dental care and antibiotic therapy. When the condition is complicated by descending mediastinitis and thoracic empyema, the mortality rate remains as high as 38% to 60% despite antibiotic therapy (Figure 4-3). When the condition in complicated by cervical necrotizing fasciitis, the more recent reported mortality rate is 18% to 22% (any delay in surgical treatment increases mortality). Tung-Yiu and colleagues reported that an immunocompromised state (e.g., diabetes mellitus) increases the risk of an odontogenic infection developing into cervical necrotizing fasciitis. Of their series of 11 cases, seven patients were immunocompromised (four with diabetes mellitus), which accounted for all major complications, including two deaths. Others have reported a mortality rate as high as 67% with severe odontogenic infections associated with diabetes mellitus. Currently there is no evidence to suggest that HIV/AIDS status increases the risk of developing Ludwig’s angina and its associated complications.
Discussion
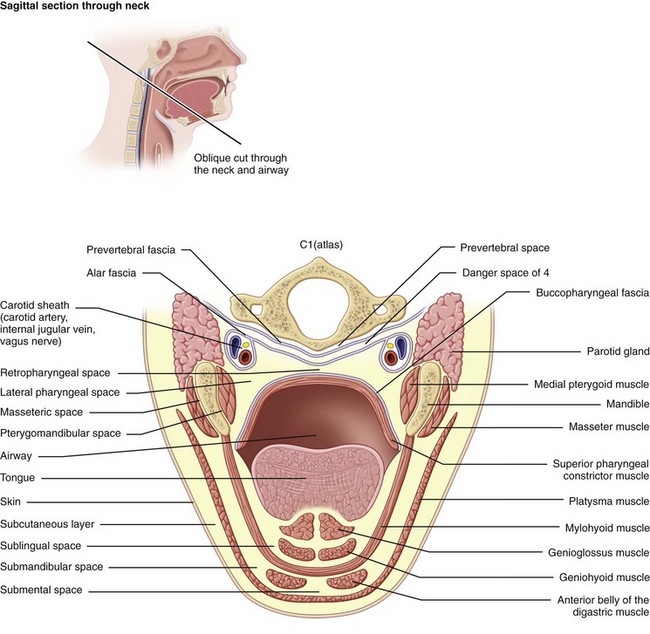
Ludwig’s angina is defined by the involvement of specific anatomic spaces (bilateral submandibular, sublingual, and submental spaces). The sublingual spaces are bounded anteriorly and laterally by the mandible, superiorly by the floor of the mouth and tongue, and inferiorly by the mylohyoid muscle. There is no anatomic barrier between the left and right sublingual spaces. The submandibular space is separated from the sublingual space by the mylohyoid muscle, thus forming the roof of the submandibular space. The hyoglossus and styloglossus muscles form the medial border, and the body of the mandible forms the lateral border. The skin, superficial fascia, platysma, and superficial layer of the deep cervical fascia form the superficial boundary. The anterior bellies of the digastric muscles form the lateral borders of the submental space. The roof is formed by the mylohyoid muscle. The symphysis of the mandible and the hyoid bone form its anterior and posterior borders, respectively. The sublingual and submandibular spaces posteriorly communicate freely with each other and with the medial masticator and lateral pharyngeal spaces, which in turn is contiguous with the retropharyngeal space. Extension of the infection along the carotid sheath (contained within the posterior compartment of the lateral pharyngeal space [LPS]) or retropharyngeal space can lead to descent into the superior mediastinum. The alar fascia separates the retropharyngeal space from the “danger space” (space 4 of Grodinksy and Holyoke), which extends to the diaphragm and the posterior mediastinum. The anterior paratracheal spaces provide anterior access to the superior mediastinum (Figure 4-4).
Allen, D, Loughnan, TE, Ord, RA. A re-evaluation of the role of tracheostomy in Ludwig’s angina. J Oral Maxillofac Surg. 1985; 43:436–439.
Barsamian, JG, Scheffer, RB. Spontaneous pneumothorax: an unusual occurrence in a patient with Ludwig’s angina. J Oral Maxillofac Surg. 1987; 45:161–168.
Bouloux, GF, Wallace, J, Xue, W. Irrigating drains for severe odontogenic infections do not improve outcome. J Oral Maxillofac Surg. 2013; 71:42–46.
Chidzonga, MM. Necrotizing fasciitis of the cervical region in an AIDS patient: report of a case. J Oral Maxillofac Surg. 2005; 63:855–859.
Chow, AW. Life-threatening infections of the head and neck. Clin Infect Dis. 1992; 14:991.
Dugan, MJ, Lazow, SK, Berger, JR. Thoracic empyema resulting from direct extension of Ludwig’s angina: a case report. J Oral Maxillofac Surg. 1998; 56:968–971.
Fischmann, GE, Graham, BS. Ludwig’s angina resulting from infection of an oral malignancy. J Oral Maxillofac Surg. 1985; 43:795–796.
Har-El, G, Aroesty, JH, Shana, A, et al. A retrospective study of 110 patients. Oral Surg Oral Med Oral Pathol. 1994; 77(5):446–450.
Loughnan, TE, Allen, DE. Ludwig’s angina: the anaesthetic management of nine cases. Anaesthesia. 1985; 40:295–297.
Mihos, P, Potaris, K, Gakidis, I, et al. Management of descending necrotizing mediastinitis. J Oral Maxillofac Surg. 2004; 62:966–972.
Potter, JK, Herford, AS, Ellis, E. Tracheotomy versus endotracheal intubation for airway management in deep neck space infections. J Oral Maxillofac Surg. 2002; 60:349–354.
Steiner, M, Gau, MJ, Wilson, DL, et al. Odontogenic infection leading to cervical emphysema and fatal mediastinitis. J Oral Maxillofac Surg. 1982; 40:600–604.
Sugata, T, Fujita, Y, Myoken, Y, et al. Cervical cellulitis with mediastinitis from an odontogenic infection complicated by diabetes mellitus: report of a case. J Oral Maxillofac Surg. 1997; 55:864–869.
Tsuji, T, Shimono, M, Yamane, G, et al. Ludwig’s angina as a complication of ameloblastoma of the mandible. J Oral Maxillofac Surg. 1984; 42:815–819.
Tsunoda, R, Suda, S, Fukaya, T, et al. Descending necrotizing mediastinitis caused by an odontogenic infection: a case report. J Oral Maxillofac Surg. 2000; 58:240–242.
Tung-Yiu, W, Jehn-Shyun, H, Ching-Hung, C, et al. Cervical necrotizing fasciitis of odontogenic origin: a report of 11 cases. J Oral Maxillofac Surg. 2000; 58:1347–1352.
Ylijoki, S, Suuronen, R, Jousimies-Somer, H, et al. Differences between patients with or without the need for intensive care due to severe odontogenic infections. J Oral Maxillofac Surg. 2001; 59:867–872.
Zachariades, N, Mezitis, M, Stavrinidis, P, et al. Mediastinitis, thoracic empyema, and pericarditis as complications of a dental abscess: report of a case. J Oral Maxillofac Surg. 1988; 46:493–495.
Buccal and Vestibular Space Abscess
Examination
Maxillofacial. Significant right-side facial edema extending from the inferior border of the mandible superiorly to the level of the zygoma (Figure 4-5). The swelling is soft and fluctuant and with no apparent intraoral or extraoral drainage (untreated buccal space infections may spontaneously drain, providing some relief or spread into other fascial spaces). There is tender right submandibular lymphadenopathy (due to active infection).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses