3
Retaining Abutment Screws
1Department of Oral and Maxillofacial Surgery, Washington Hospital Center, Washington, DC; and American Institute of Implant Dentistry, Washington, DC
2Department of Oral and Maxillofacial Surgery, Washington Hospital Center, Washington, DC
Introduction
The screw that connects the abutment to the implant body is called the prosthetic screw or retaining abutment screw (Figure 3.1). If this small, yet critical, component of the implant system is overlooked, the patient and clinician can face serious challenges. Improper use of the prosthetic screw can have deleterious effects on the implant components, surrounding bone, and final restoration. Prosthetic screws are available in different shapes, sizes, and materials depending on the manufacturer. An understanding of the materials and physical and mechanical aspects are necessary for proper implant–abutment connection, and ultimately implant success. Despite our best efforts, prosthetic failures occasionally occur, and this chapter will also discuss methods for the retrieval of fractured and stripped prosthetic screws.

Basic Terminology
Torque or Moment of Force
This is the tendency of a force to rotate an object about an axis, measured in Newton-centimeters (N-cm). In implant dentistry, this is colloquially referred to as the “tightness” at which the prosthetic screw is secured. Electronic or mechanical torque measuring devices are available to indicate magnitude of torque applied to the prosthetic screw.
Preload or Clamping
In implant dentistry, preload or clamping refers to the linear force, which a stretched prosthetic screw transmits to the abutment and implant body, holding the components together. Preload is measured in Newtons (N). As the prosthetic screw is tightened, the torque applied is transferred to the threads of the prosthetic screw and internal threads of the implant (Figure 3.2). This force clamps the abutment to the implant body. Preload is determined by three factors:
- Torque, which influences screw head friction, thread friction, and elastic (reversible) deformation of the screw.
- Screw head geometry.
- Materials of the screw and abutment, which influence the level of grip (McGlumphy et al. 1998).

Torque has a direct correlation to preload, and is the only factor directly influenced by the clinician. To date no “ideal” preload value has been determined for all prosthetic screws. Because preload is determined by so many different factors, it is recommended to follow each manufacturer’s guidelines for each specific screw.
Reverse Torque or Detorque
This is the amount of torque applied in a counterclockwise direction to a prosthetic screw to unscrew it from the implant.
Screw Loosening
This refers to the unwanted rotation of the prosthetic screw in a counterclockwise direction. Screw loosening is one of the most common complications encountered in implant dentistry (Ekfeldt et al. 1994). Loose screws are at a significantly higher risk of screw fracture. Binon and McHugh (1996) suggest multiple reasons for screw loosening:
- Poor tightening.
- An inadequate prosthesis.
- Poor component fit.
- Excessive loading.
- Settling of the screw.
- Elasticity of the bone.
Settling or Torque Loss
This is a decrease in preload as a result of burnishing of both the internal implant threads and the prosthetic screw threads. Unlike screw loosening, the prosthetic screw does not “unscrew.” The frictional forces between the components are decreased as a result of creep and stress relaxation, which eventually will cause a decrease in preload. This is a normal occurrence which should be anticipated and corrected by retorqueing the prosthetic screw to the recommended moment force after a period of time. It is recommended that the prosthetic screws be retorqued 10 minutes after initial placement and periodically thereafter (Winkler et al. 2003; Cantwell and Hobkirk 2004). Torque loss will also occur over longer periods of time. It is recommended to retorque the prosthetic screw at each recall visit. This has not been shown to have any harmful effects on the implant joint stability (Delben et al. 2011).
Abutment Screw Mechanics
Prosthetic screws are manufactured in a variety of different shapes, sizes, and materials (Figure 3.3). It is important to understand the implication of this aspect on the final prosthetic outcome. Although a seemingly small and simple piece, the mechanics of the prosthetic screw are fairly complex. Literally, this piece holds the implant system together and thus it requires sophisticated engineering to provide the best possible prosthetic results.

Shape and Size
Like any other screw, there are three basic components of the prosthetic retaining screw (Figure 3.4):
- Screw head: The head contains the driver fitting site, which is used to rotate the screw into position. Various driver fitting site types are available, including slot (flat-head), Phillips, Robertson (square), hex, and star. By far, the most common type used in implant dentistry is the hex type. It is critically important to use the appropriate corresponding driver to prevent screw head stripping.
- Shank: The shank is the unthreaded portion of the screw below the head. It is variable in length depending on the geometry of the components that are being held together.
- Thread: Without going into too much complexity, the thread can come in a myriad of different dimensions. This portion of the screw engages the internal threads of the implant and provides the surfaces onto which force is transmitted and converted to preload. The internal threads of the implant and those of the prosthetic retaining screw must be 100% compatible.

Abutment Screw Materials
Commercially Pure Titanium
This is one of the most common materials used to manufacture prosthetic screws (Figure 3.5). This material generates the least amount of preload for a given torque when compared with other materials. After applying desirable torque, commercially pure titanium prosthetic screws only undergo elastic (reversible) deformation, and can thus be used multiple times. These screws are appropriate for use with temporary restorations and laboratory procedures. They are not recommended for use with final restorations.

Coated or Treated Titanium
In an effort to decrease friction and increase preload, manufacturers began coating and treating titanium screws (Figure 3.6). Coatings and treatments can include gold, tungsten carbon carbide, and nitrides. Titanium treated in such a way to include different chemicals is called titanium alloy. These alloys are expensive to manufacture, but have very high tensile strength and toughness. In general, coated and treated prosthetic screws are able to provide higher preload than non-pure titanium prosthetic screws, and are more capable of maintaining preload after cyclical loading.

Gold
Gold prosthetic screws are available in pure gold and in gold alloys that contain other elements to strengthen the metal (Figure 3.7). Gold can act as a dry lubricant, decreasing the amount of friction between the threads as the screw is tightened. This allows increased rotation and elongation of the screw for a given torque, and thus a greater preload. These screws are least likely to loosen over time. However, gold screws, especially those of high carat, are subject to plastic (irreversible) deformation, and thus are only indicated for single use. It is recommended that before final delivery of the abutment and prosthesis, the clinician use titanium screws and to only use gold screws during final delivery.

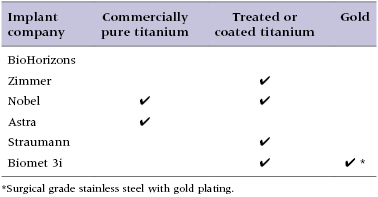
Implant manufacturers are now making implant components that are ostensibly interchangeable between systems. However, even the slightest incompatibility in physical characteristics and chemical composition of implant components affects preload and can have an effect on settling and screw loosening (Kim et al. 2012). Despite a seemingly accurate fit, slight differences in thread pitch or materials incompatibility can have significant long-term consequences and ultimately result in failure. Thus, it is always recommended using the same company for implant, abutment, screw driver, and prosthetic screw. Table 3.1 lists the screw materials that are currently available from major implant companies.
Table 3.1 Prosthetic screws available from the major implant companies
Special Considerations
Implant Connection Types
When deciding on an implant, it is also important to consider how different connection types relation to the prosthetic retaining screw. Internal connection implants have been shown to have/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


