Introduction
The objective of this study was to examine the effects of ultraviolet-mediated photofunctionalization of miniscrews and the in-vivo potential of bone-miniscrew integration.
Methods
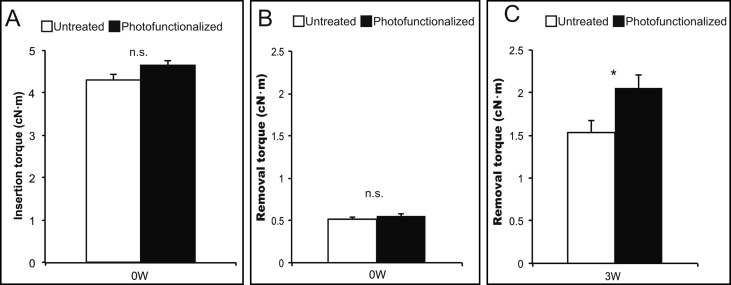
Self-drilling orthodontic miniscrews made from a titanium alloy were placed in rat femurs. Photofunctionalization was performed by treating the miniscrews with ultraviolet light for 12 minutes with a photo device immediately before implantation. Maximum insertion torque (week 0), removal torque (weeks 0 and 3), and resistance to lateral tipping force (week 3) were examined.
Results
The removal torque at 3 weeks of healing was higher for the photofunctionalized screws than for the untreated screws. The regenerated bone tissue was more intact and contiguous around the photofunctionalized miniscrews than around the untreated ones. The miniscrew-bone complex seemed to produce interface failure, not cohesive fracture, in both groups. The displacement of untreated screws under a lateral tipping force was greater than that of photofunctionalized miniscrews.
Conclusions
These results suggest that photofunctionalization increases the bioactivity of titanium-alloy miniscrews and improves the anchoring capability of orthodontic miniscrews, even without modification of the surface topography.
Highlights
- •
Miniscrews were converted from hydrophobic to hydrophilic after photofunctionalization.
- •
At week 3, the removal torque was higher for photofunctionalized screws than for untreated screws.
- •
The miniscrew-bone complex showed interface failure, not cohesive fracture, in both groups.
- •
The displacement of untreated screws was greater than that of photofunctionalized screws.
Functional appliances are a common choice for treating mandibular deficiency, and headgear is an equally obvious choice for treating maxillary excess in children. In adults, however, skeletal problems are not corrected with functional appliances or headgear. Traditionally, extraoral or intraoral appliances such as high-pull headgear and interarch elastics have been used to help maintain the anchorage of the maxillary posterior teeth. However, high-pull headgear has inherent disadvantages associated with patient noncompliance, duration of wear, unacceptability by many adults, and potential risk of injury. Therefore, since the advent of temporary anchorage devices and skeletal anchorage devices, miniplates and miniscrews have been used to obtain skeletal anchorage, with promising results. Compared with the placement of miniplates, in which the mucosa is cut to produce a flap, miniscrew insertion involves a minimal surgical invasion. Moreover, screws have many advantages, including low cost, possible immediate loading, and possible placement in most areas of the alveolar bone.
The success rate of miniscrews has been reported to be somewhat less than that of dental implants, with failure rates from 9% to 16.4%. For miniscrews to obtain clinical success, stability is an important factor. The primary stability of miniscrews has been associated with many factors, including insertion site characteristics, root proximity, geometric design of the screw, soft-tissue inflammation, operator technique, insertion torque, and magnitude and loading time of the orthodontic force. Particularly, poor quality and quantity of host bone result in the lack of primary stability.
Miniscrews are intended to be removed at the end of their clinical application, whereas conventional prosthodontic implants are intended to be in place permanently. Therefore, miniscrews are generally made of commercially pure titanium or titanium alloy (Ti-6Al-4V) and manufactured with an untreated, smooth surface. Recently, titanium surface modifications and improvements to implant surface topography have been among the important factors shown to enhance osseointegration of endosseous implants. However, these changes, caused by the increased intercuspation between the roughened screw surface and the bone, may also lead to the fracture of miniscrews because of the enhanced removal torque. Therefore, there is a need for miniscrews produced without modification of the surface topography.
Ultraviolet (UV)-mediated photofunctionalization immediately before use, by a combination of UV-A and UV-C for aging the titanium surface, is a recently reported method of surface modification for titanium to increase its biologic capacity; it is characterized by remarkable efficacy, unique mechanisms, and a simple delivery method. A 15-minute UV treatment protocol with optimized lighting conditions was established at experimental levels, followed by an even shorter protocol of a 12-minute treatment. These protocols are clinically applicable to dental implants, and the treatment is performed at chairside immediately before their use. Physicochemical changes in titanium by photofunctionalization include 3 key surface properties: the generation of superhydrophilicity; a significant reduction of surface carbon, which unavoidably and unexceptionally accumulates on titanium surfaces; and electrostatic conversion from negative to positive. These factors act synergistically to increase the recruitment, attachment, and retention of osteogenic cells. The biomechanical strength of in-vivo osseointegration for photofunctionalized dental implants was 3 times greater than that for untreated dental implants at the early healing stage in an animal model. The effectiveness of photofunctionalization has been proven for all surface topographies tested. The technology does not alter the existing topography, roughness, or other morphologic features of the implants and is categorized as neither an additive nor a subtractive method.
We tested the biologic potential of photofunctionalized miniscrews with what was assumed to be poor bony support. We hypothesized that photofunctionalization of miniscrews enhances removal torque, not insertion torque, because there has been no change in topography. The objective of this study was to examine the effects of photofunctionalization of miniscrews and the in-vivo potential of bone-miniscrew integration.
Material and methods
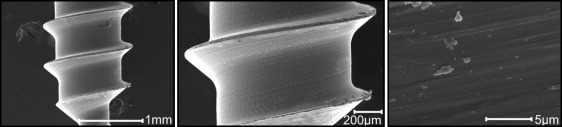
A self-drilling type of orthodontic miniscrew implant (Jeil Medical, Seoul, Korea; diameter, 1.4 mm; length, 6 mm) was used. It was made from a titanium-aluminum-vanadium alloy. The surface morphology was examined by scanning electron microscopy (SEM) (mosel XL30; Philips, Eindhoven, The Netherlands). Photofunctionalization was performed by treating samples with UV light for 12 minutes with a photo device (TheraBeam Super Osseo; Ushio, Tokyo, Japan) immediately before implantation. Hydrophilicity of the photofunctionalization and untreated miniscrew surface was assessed by 1 μL of distilled and deionized water placed on the miniscrew implant ( Figs 1 and 2 ).

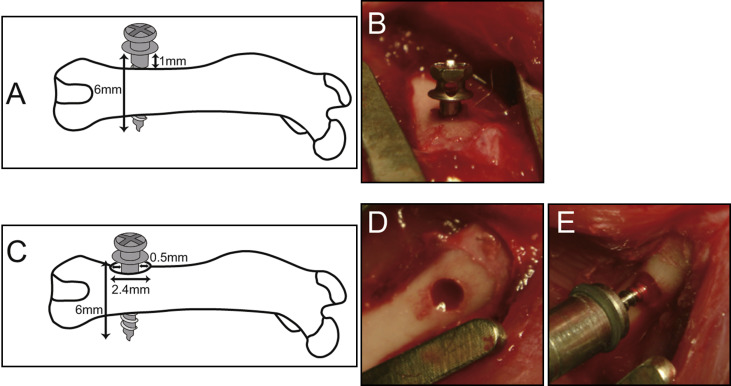
Twelve-week-old male Sprague Dawley rats were anesthetized with 1% to 2% isoflurane inhalation. After the animals’ legs were shaved and scrubbed with 10% povidone-iodine solution, the distal aspects of the femurs were carefully exposed via skin incision and muscle dissection. The flat surfaces of the distal femurs were selected for implant placement. The rats were divided into 2 research models. One had an implant site prepared 9 mm from the distal edge of the femur by drilling with a 1.0-mm round burr. Profuse irrigation with sterile isotonic saline solution was used for cooling and cleaning. One untreated orthodontic miniscrew and 1 photofunctionalized miniscrew were placed in each side of the femur alternately. The miniscrews were tightened into the hole until the screw threads were embedded below the surface of the bone. Next, they were screwed in reverse to about 1 mm from the surface of the bone (reverse model). The surgical sites were then closed in layers. Muscle and skin were sutured separately with resorbable suture thread ( Fig 3 , A and B ). The other model had an implant site prepared 9 mm from the distal edge of the femur by drilling with a 2.4-mm round burr to create a 0.5-mm gap around a miniscrew (gap model). A gap model for miniscrews was designed in the rat femur as schematically shown in Figure 3 , C-E , to simulate thin cortical bone or low bone density. Profuse irrigation with sterile isotonic saline solution was used for cooling and cleaning. One untreated orthodontic miniscrew and 1 photofunctionalized miniscrew were placed in each side of the femur alternately. The miniscrews were tightened into the hole until the screw threads were embedded below the surface of the bone. Next, they were screwed in reverse to about 0.3 mm from the surface of bone. The surgical sites were then closed in layers. Muscle and skin were sutured separately with resorbable suture thread. The University of California at Los Angeles Chancellor’s Animal Research Committee approved this protocol, and all experimentation was performed in accordance with the guidelines of the U.S. Department of Agriculture for animal research.
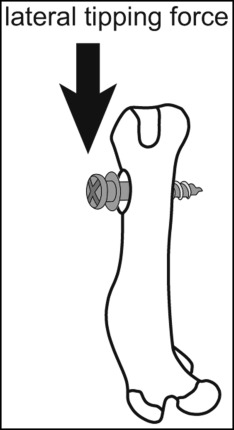
Maximum insertion torque at miniscrew insertion (week 0) and removal torque (week 0 at the time of screwing in reverse, and week 3) were assessed with a torque wrench (FTD2CN-S/FTD5CN-S; Tohnichi, Tokyo, Japan). Placement and removal torque values of all miniscrews were assessed by the same orthodontist (M.T.). To evaluate the anchoring capability of miniscrews, the resistance of miniscrews to a lateral tipping force was measured by modifying the previously established implant biomechanical test in the rat femur model. This biomechanical test was established and validated to sensitively and specifically measure the strength of bone-implant integration. After 3 weeks of healing, the femurs containing the miniscrew implants were harvested and embedded in autopolymerizing resin with the top surface of the implant level: ie, the long axis of the miniscrew was vertically aligned ( Fig 4 ). After polymerization of the resin, the resin block was positioned vertically on the stage of a mechanical testing machine (model 5544; Instron, Canton, Mass), which operated at a speed of 1 mm per minute with a pushing rod (diameter, 0.8 mm) so that the long axis of the miniscrew was aligned horizontally ( Fig 4 ). A force was applied to the head of the miniscrew. The load imposed on the testing rod and the displacement were recorded at a data sampling rate of 60 Hz.
The method we used for testing the morphology and quality of bone formed around the miniscrew has been demonstrated to be useful for the assessment of the behavior and the quality of bone around implants. At week 3 of healing, after performing the removal torque test, we harvested the bone-miniscrew complex, and the miniscrew surface was carefully exposed. The miniscrew specimen was soaked in agitated water for 1 hour and dried under heat in a vacuum. The specimens were sputter coated with carbon and then examined by SEM for surface morphology and by energy dispersive x-ray spectroscopy (model JSM-5900LV; Joel, Tokyo, Japan) for the elemental composition. SEM imaging was performed in 3 regions (upper, middle, and lower).
Statistical analysis
There were 8 samples for the torque test and the lateral tipping test, respectively. All data are presented as means and standard errors of the means, and statistical analysis was carried out by 1-way analysis of variance and the Tukey multiple comparison test. All statistical analyses were performed with Prism software (version 5; GraphPad Software, San Diego, Calif). P <0.05 was considered to be significant.
Results
We tested the surface characteristics of the titanium samples before and after photofunctionalization. The miniscrew implants made of the titanium alloy that were used in this study are shown in Figure 1 , A . Low-magnification SEM imaging showed a relatively smooth surface morphology of the miniscrews, with concentric traces characteristic of a turning lathe that are typically seen on machined titanium surfaces. High-magnification imaging shows parallel marked, scraped, and scratched surface morphology at the supramicrometer level ( Fig 2 ). The untreated miniscrew, as received, had a hydrophobicity as shown by the images of a 1-μL droplet of water, which remained spherical ( Fig 1 , B ). The miniscrew was converted to being superhydrophilic after photofunctionalization, showing an immediate spread of the water ( Fig 1 , C ). Figure 3 , E , shows the miniscrew implant surgery. The blood from the bone marrow was tracked up to the top along the photofunctionalized miniscrew immediately on contact with the drill site because of the screw’s superhydrophilicity.
On the 1-mm reverse model, with maximum insertion torque and removal torque at week 0, no differences were observed among the untreated and the photofunctionalized miniscrews. However, the removal torque at week 3 of healing on the photofunctionalized screws was higher than on the untreated ones ( Fig 5 ). Moreover, to examine the nature of biologic tissues around the miniscrew implants, miniscrew-tissue complexes were retrieved at week 3 of healing, and the morphologic characteristics of the untreated and the photofunctionalized miniscrews were compared. Representative SEM images at the upper (upper cortical), middle (bone marrow), and lower (lower cortical) regions are shown in Figure 6 . The regenerated bone tissue was intact and contiguous around the photofunctionalized miniscrews ( Fig 6 , D-F , I , and J ), with minimal remaining gaps. The untreated miniscrews had biologic tissues on their surfaces in the bone marrow zone ( Fig 6 , B ), with high-magnification imaging confirming tissue formation or remnant tissues of different morphology from the bare miniscrew surface ( Fig 6 , H ). These SEM images were taken after testing with removal torque at week 3. The miniscrew-bone complex showed interface failure, not cohesive fractures, in both groups ( Fig 6 , G and J ).