This article describes the orthodontic relapse with mandibular incisor fenestration in a 36-year-old man who had undergone orthodontic treatment 21 years previously. The patient reported that his mandibular 3 × 3 bonded retainer had been partially debonded and broken 4 years earlier. The mandibular left lateral incisor remained bonded to the retainer and received the entire load of the incisors; consequently, there was extreme labial movement of the root, resulting in dental avulsion. As part of the treatment, the root was repositioned lingually using a titanium-molybdenum segmented archwire for 8 months, followed by endodontic treatment, an apicoectomy, and 4 months of alignment and leveling of both arches. The treatment outcomes were excellent, and the tooth remained stable, with good integrity of the mesial, distal, and lingual alveolar bones and periodontal ligament. The 1-year follow-up showed good stability of the results.
Highlights
- •
A 36-year-old man experienced orthodontic relapse with incisor fenestration.
- •
A mandibular bonded retainer had partially debonded and broken 4 years earlier.
- •
The left lateral incisor received the entire load and was avulsed.
- •
Treatment included root repositioning, endodontics, apicoectomy, leveling, and aligning.
- •
Treatment outcomes were excellent, and the tooth remained stable 1 year later.
Orthodontic relapse in the anterior region of the mandibular arch is not uncommon. This is predominantly caused by constriction of the transverse distance of the canines, late growth of the mandible, and mesial direction of the occlusal forces. The best available option for avoiding mandibular arch relapse is the use of 3 × 3 bonded retainers, which can be worn for indefinite periods after orthodontic treatment. However, when the flexible wire retainers become activated, crown displacement or torque movements of the roots of the incisors or canines can make retreatment necessary.
Pazera et al reported a case in which the root of the mandibular right canine had moved buccally as a result of a broken 3 × 3 bonded retainer, and they considered it the result of wire deflection during the bonding process or even a mechanical deformation in the posttreatment period. However, since the root did not perforate the soft tissue and also retained its vitality, the authors were able to successfully reposition the root.
Here, we report on a patient who had completed orthodontic treatment 21 years previously but had been wearing a broken mandibular 3 × 3 bonded retainer for 4 years, resulting in accentuated gingival recession and tooth avulsion.
Case report
The patient was a 36-year-old man who had been diagnosed with both skeletal and dental Class II malocclusion and had been treated in our clinic in Santa Maria, RS, Brazil, with cervical headgear and standard edgewise fixed appliances. The treatment began 24 years previously and had been completed 21 years before this report. Thereafter, the patient had received a maxillary removable retainer and a mandibular 3 × 3 retainer bonded to the 6 anterior teeth. He remained under the orthodontist’s observation, with annual posttreatment follow-up examinations for up to 10 years; thereafter, he had no examinations for 11 years. At this point, he returned to the clinic with the complaint of extreme gingival recession on the labial surface of his mandibular left lateral incisor accompanied by pain in the affected tooth under certain conditions.
The clinical examination showed that the bonded retainer was broken between the mandibular right lateral incisor and the canine. Furthermore, the right lateral incisor and the right central incisor had moved lingually; consequently, the left canine had moved labially. In the initial clinical examination, we verified that the mandibular left lateral incisor received the complete load of the incisal guidance during mandibular movements. The retainer worked as a support, and the wire became debonded inside the resin of the mandibular left lateral incisor, working as a center of rotation. This system generated an extreme labial torque on the root, causing total fenestration of the root including the anterior contour of the apex ( Figs 1 and 2 ). Unfortunately, the vitality test of this tooth was negative. Likewise, in the maxillary arch, there were accentuated recessions and root abrasions on the left lateral incisor and both canines. Therefore, the chosen line of treatment for the mandibular left lateral incisor involved calcium-hydroxide therapy in the pulp cavity with concomitant tooth repositioning, followed by obturation after tooth movement and an apicoectomy with deep cleaning of the apical region. The maxillary tooth would be aligned and leveled; then the roots of the left lateral incisor and the canines would be restored with compomer.

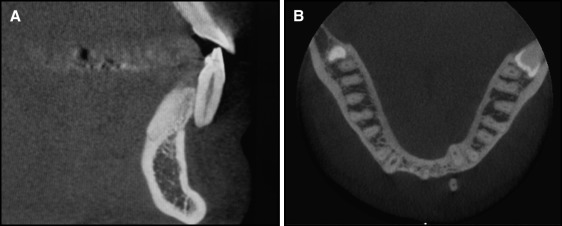
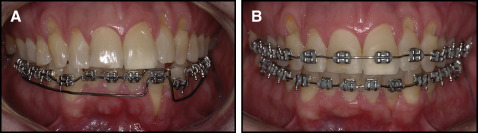
For repositioning the tooth, 0.022 × 0.028-in edgewise standard brackets were bonded only in the mandibular arch. First, a passive 0.021 × 0.025-in stainless steel archwire was inserted in all brackets except that of the mandibular left lateral incisor. Thereafter, the lingual torque of the root was corrected with a 0.019 × 0.025-in titanium-molybdenum wire connected only to the bracket of the mandibular left lateral incisor and activated in 10 g of force in the posterior region between the mandibular second premolars and the first molars on both sides ( Fig 3 ). Because there was about 30 mm of distance between the lateral incisor and the point where the force was applied, a system with a moment of about 300 g of force per millimeter acting over the root was developed. The archwire for torque movement was activated every month for 5 months. By the fifth month, the apex was totally covered with soft tissue; consequently, the apicoectomy was performed ( Fig 4 ). Thereafter, a maxillary orthodontic appliance was bonded, and alignment and leveling were performed for both arches from 0.014-in to 0.019 × 0.025-in stainless steel archwires, along with individual lingual root torque for the mandibular left lateral incisor and labial root torque for the mandibular left canine. After 13 months of treatment and after 1 month of stabilization without activation, the root was completely covered with gingival soft tissue, with only a small gingival defect visible on the labial surface of the root ( Fig 5 ). The posttreatment cone-beam computed tomography (CBCT) image showed that the root was positioned over the alveolar bone and that no regeneration of the buccal wall of the alveolar bone could be achieved. However, some integrity of the mesial and partly of the distal wall surrounding the root was present. The wide alveolar ridge at the level of the mandibular left lateral incisor ( Fig 2 , A ) was resorbed because of the lingual root movement, and only a small part of the lingual wall seemed to be present ( Fig 6 , A ). However, periodontal probing showed a sulcus depth of only 1 mm labially ( Fig 6 ). Finally, a 4 × 4 retainer of 0.016 × 0.022-in stainless steel wire was bonded to the mandibular arch, and the maxillary arch received a wraparound retainer. At the 1-year follow-up, the results obtained were totally stable in both clinical or tomographic analyses ( Figs 7 and 8 ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


