A unilateral posterior crossbite with facial asymmetry is difficult to correct with orthodontic treatment alone. This case report describes the orthodontic treatment and additional plasty without orthognathic surgery for a 19-year-old woman with a transverse discrepancy. The posterior crossbite was resolved by expansion of the narrow maxillary arch and space closure in the mandibular arch. This accelerated the correction of the functional shift of the mandible. After resolution of the unilateral posterior crossbite, the problems of the anteroposterior molar relationship were treated using orthodontic mini-implants. Mandibular angle reduction plasty was performed for the asymmetric mandibular border to improve the facial appearance. After treatment, the patient had a more symmetrical facial appearance, normal overjet and overbite, and midline coincidence. The treatment results remained stable 1 year after treatment. This case report demonstrates that a minimally invasive treatment can successfully correct a unilateral posterior crossbite with a transverse discrepancy.
Highlights
- •
Consideration of hidden functional shift by compensated dentition is important.
- •
Orthognathic surgery may not be necessary to correct Class I facial asymmetry.
- •
Arch relationship can be normalized by decompensation of a compensated dentition.
- •
Minimally invasive treatment can correct a unilateral posterior crossbite with a transverse discrepancy.
Generally, when we establish the treatment plan for patients with facial asymmetry, surgery is included because facial asymmetry is usually caused by skeletal problems. Orthodontic treatment alone is a difficult choice in this situation. Patients with facial asymmetry and a skeletal Class III malocclusion must be treated by orthognathic surgery even if there is no facial asymmetry. However, more consideration is needed to treat patients with facial asymmetry and a skeletal Class I relationship. Because correction of the asymmetry is the only goal of the orthognathic surgery in this case, satisfaction with the treatment may be low after surgery. Moreover, patients with facial asymmetry and a transverse discrepancy can be treated with orthodontics alone. This case report describes the treatment of a woman with a unilateral posterior crossbite and facial asymmetry. She had a skeletal Class I relationship. Her chin and mandibular midline were deviated to the left side with a left posterior crossbite. Because there was a transverse discrepancy, a nonsurgical approach for the correction of the occlusion could be planned. Mandibular angle reduction plasty was planned for the asymmetrical mandibular inferior border. By avoiding orthognathic surgery, it was possible to minimize the patient’s discomfort.
Diagnosis and etiology
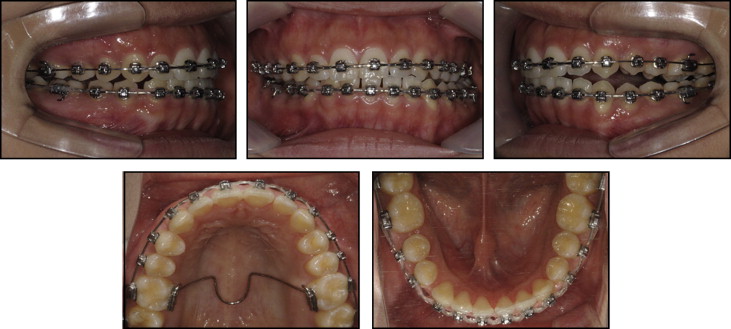
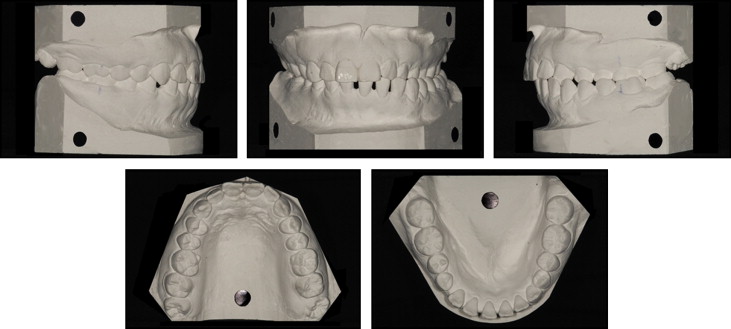
The patient was a 19-year-old woman who visited Seoul National University Dental Hospital in South Korea for an orthodontic consultation. No specific medical problems or temporomandibular joint symptoms were observed. She had a skeletal Class I relationship and facial asymmetry, with the chin deviated 4.5 mm to the left. A slight maxillary deficiency and a normal vertical growth pattern were seen. A Class I molar relationship on the right and a Class II molar relationship on the left were observed, and a posterior crossbite from the left lateral incisor to the left second molar was observed ( Fig 1 ). The mandibular dental midline was deviated 6.5 mm to the left. There was space between the mandibular anterior teeth ( Fig 2 ). The cant of the occlusal plane was minor. In the lateral cephalometric analysis, no mouth protrusion or problems of anterior tooth inclination were found ( Table I ). The major problems were summarized as frontal asymmetry, deviation of the chin, left posterior crossbite, and mandibular dental midline deviation. Furthermore, the patient had a slight transverse centric occlusion–centric relation discrepancy. This functional shift of the mandible caused mandibular asymmetry, which could be observed in the panoramic and posteroanterior radiographs ( Fig 3 ). In particular, the mandibular left inferior border was much bulkier than right inferior border. This difference in mass was the cause of the facial asymmetry.

| Pretreatment | Posttreatment | |
|---|---|---|
| ANB angle (°) | 2.4 | 2.4 |
| A to N perpendicular (mm) | −1.2 | −1.2 |
| Pog to N perpendicular (mm) | −5.9 | −5.5 |
| Björk sum (°) | 393.0 | 401.4 |
| FMA (°) | 22.3 | 30.7 |
| U1 to FH (°) | 108.7 | 108.4 |
| U1 to SN (°) | 98.0 | 97.7 |
| IMPA (°) | 104.2 | 88.3 |
| Interincisal angle (°) | 124.8 | 132.6 |
| Upper lip to E-line (mm) | −2.3 | −4.9 |
| Lower lip to E-line (mm) | −0.1 | −1.8 |
| Nasolabial angle (°) | 96.6 | 93.4 |

Treatment objectives
The treatment objectives for the dentition were correction of the left posterior crossbite, making the maxillary and mandibular midlines coincident, and closing the mandibular arch space. The treatment objectives for the skeleton were improving the facial asymmetry, including the deviation of the chin, and improving the transverse discrepancy. Thus, facial symmetry, normal overjet and overbite, and Class I canine-to-molar relationships could be obtained.
Treatment objectives
The treatment objectives for the dentition were correction of the left posterior crossbite, making the maxillary and mandibular midlines coincident, and closing the mandibular arch space. The treatment objectives for the skeleton were improving the facial asymmetry, including the deviation of the chin, and improving the transverse discrepancy. Thus, facial symmetry, normal overjet and overbite, and Class I canine-to-molar relationships could be obtained.
Treatment alternatives
Facial asymmetry and unilateral posterior crossbite are difficult to treat with orthodontics alone. Therefore, the first plan was orthodontic treatment accompanied by orthognathic surgery. Extraction of the 2 maxillary third molars was planned. Leveling of maxillary and mandibular arches and space closure of the mandibular arch were planned as the presurgical orthodontic treatment. After that, the asymmetries of the chin and mandible could be corrected with orthognathic surgery. Postsurgical orthodontic treatment would finish correction of the malocclusion. This plan has the advantage of eliminating the patient’s skeletal asymmetry, but at the cost of surgical risk and financial burden.
The second plan was orthodontic treatment and additional plasty without orthognathic surgery. Expansion of a narrow maxillary arch can help to correct the transverse discrepancy by releasing the locking in the left posterior teeth. After that, maxillary left molar distalization and mandibular left molar mesialization were planned to correct the left molar relationship and the dental midline. Mandibular angle reduction plasty and genioplasty were planned for the bulky left inferior border of the mandible. This plan would minimize the burden of surgery while maximizing the reduction of asymmetry. The downside is that it is difficult to eliminate the asymmetry completely.
The patient selected the second option because she did not want orthognathic surgery.
Treatment progress
Metal self-ligating brackets (0.022-in slot, Damon Q; Ormco, Glendora, Calif) were used for this treatment. Initial leveling progressed with a 0.014-in nickel-titanium archwire. A lingual sheath was attached to the palatal side of the maxillary first molar, and an expansion transpalatal arch was inserted into the lingual sheath ( Fig 4 ). Buccal root torque was given to the expansion transpalatal arch to decompensate the inclination of the maxillary left first molar ( Fig 5 ). The relationship of the left posterior teeth was improved to an edge bite after 4 months of leveling and expansion of the maxillary arch. To resolve the minor cant of the maxillary left anterior teeth, a titanium orthodontic mini-implant (OMI; diameter, 1.6 mm; length, 6.0 mm; Jeil Medical, Seoul, South Korea) was inserted between the mandibular left premolars. Intermaxillary elastics were applied from the OMI to the maxillary left canine and premolars. After leveling of the mandibular arch, elastomeric modules were used to close the remaining space. After 7 months of treatment, the unilateral posterior crossbite was corrected ( Fig 6 ). Expansion of the maxillary arch relieved the functional shift of the mandible ( Fig 5 , B ). In addition, the reduced mandibular intermolar width helped reduce the functional shift ( Table II ). After resolution of the unilateral posterior crossbite, mandibular angle reduction plasty and genioplasty were done to improve the bulky left inferior border of the mandible. Despite the improvement of the left posterior crossbite, a Class II molar relationship remained. Distalization of the maxillary left molars and mesialization of the mandibular left molars were planned to improve the molar relationships and the mandibular dental midline. At first, a titanium OMI was inserted between the maxillary second premolar and the first molar. After ligation between the OMI and the second premolar, the molars were distalized during 3 months using open-coil springs between the second premolar and the first molar ( Fig 7 ). After that, the OMI was moved between the maxillary first and second molars, and distalization of the remaining anterior teeth was performed. At the same time, an OMI was inserted between the mandibular left lateral incisor and the canine. The mandibular left molars were mesialized using elastomeric modules from the OMI. After 13 months, active treatment was finished, and all fixed orthodontic appliances were removed. Fixed lingual retainers were attached to both arches, and circumferential retainers were placed additionally. The instructions to the patient included full-time retainer use for 3 months and then nighttime use for 2 years at least.