and Augusto Ureña1
(1)
Department of Orthodontics, Maimonides University, Buenos Aires, Argentina
Lower anterior crowding is a problem that affects nearly 80 % of the adult population.
It is accepted that it is greatly due to the diminishing of the arch length as a result of aging.
It can be seen in Class I, II, or III patients no matter the facial biotype or whether they were treated orthodontically or not.
Regarding etiology, it can be classified into three groups: primary, secondary, or as a consequence of relapse.
The primary group is the result of a negative relation between the teeth width and the arch length.
If it appears later in life, it could be related to parafunctional habits, loss of vertical posterior dimension, or occlusal problems, and these patients are in the secondary group. Some studies show that there is no close relationship among the shape of the inferior incisors, the irregularity index, or the lower anterior crowding.
It is important to take into account not only the degree of the crowding but also the rate of progression during the last years. If the progression is high, it is necessary to check if posterior occlusal contacts are present.
Little et al. (1988) as well as Bishara et al. (1996) observed that there are no specific variables that could determine when and to what extent relapse could occur in patients treated with or without extractions.
When the crowding is less than 5 mm, stripping or mesiodistal enamel reduction is the best choice. Considerations should be similar to those when labial brackets are used. This procedure was described for the first time in 1944 by Ballard and then was popularized by Dr. Bjorn Zachrisson (Zachrisson 2005; Zachrisson et al. 2007).
Shillingburg and Grace, in 1973, established the amount of enamel that could be removed from each anterior tooth (mesial and distal sides), and Sheridan (Sheridan 1987; Sheridan and Hastings 1992) promoted stripping in the lateral areas.
Stripping is never performed before brackets are placed since the space gained could be easily lost. The shape of the anterior teeth is important; those with a triangular shape make it easier to perform stripping.
Bjorn Zachrisson (Zachrisson 2005; Zachrisson et al. 2007) demonstrated that it is recommendable to begin on teeth that are better positioned in order to avoid unnecessary stripping or steps that are very difficult to correct.
The authors recommend the use of diamond single-side strips because a better control is achieved. The use of burs or disks could produce more and unfavorable loss of enamel.
Before enamel reduction is performed, it is important to take intraoral radiographs to determine the thickness of the enamel and the position of the roots in relation to the inter-radicular bone.
The amount of enamel that must be removed from each side of the tooth by stripping is only 0.25–0.50 mm in total, and the dentin will not be exposed, of course. The total maximum amount of stripping recommended is 4 mm in the upper anterior teeth and 3 mm for the mandibular incisors.
After it, a careful polishing of the stripped areas is highly recommended in addition to daily fluoride rinses (Radlanski 1988).
It is important to remember that this procedure can be performed if the patients have good oral hygiene. Otherwise, interproximal cavities will be the result in a very short period of time.
At the end of the treatment, a fixed bonded retainer is advisable and should also be controlled every 6 months, for a long period of time.
Stripping is contraindicated in patients with rectangular-shaped teeth, hypoplasia, or hypersensitivity.
The following cases will demonstrate these principles.
Case Study 1
A 26-year-old female patient visited the clinic complaining about anterior lower crowding. She had had a 3-year orthodontic treatment and two first upper bicuspid extractions (Fig. 2.1a, b).
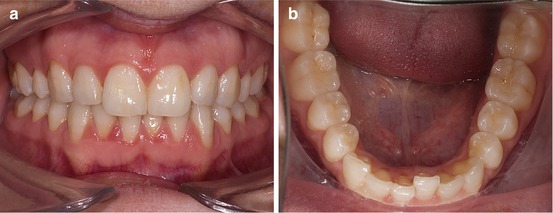
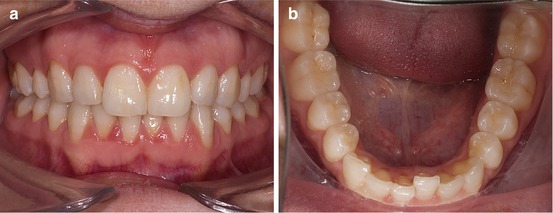
Fig. 2.1
(a, b) Pretreatment front and lower occlusal photographs
No retention appliance was indicated at that time.
Gingival margin, overjet, and overbite were pretty normal.
The molar relationship was Class I canine and molar on the right and Class II on left side. The upper incisors were slightly retroinclined.
Good oral hygiene was present (Fig. 2.2a, b).
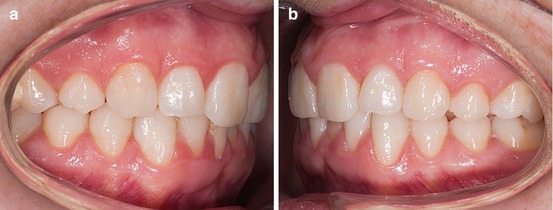
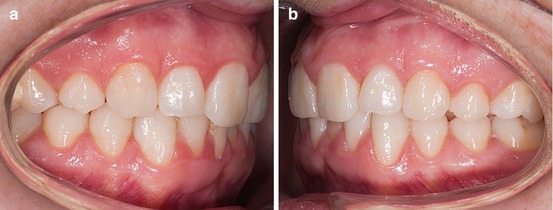
Fig. 2.2
(a, b) Lateral photographs at the beginning of the treatment
Mandibular arch discrepancy was – 3 mm.
The treatment objective was to correct the anterior crowding without extractions using interproximal enamel reduction (Fig. 2.3a, b).
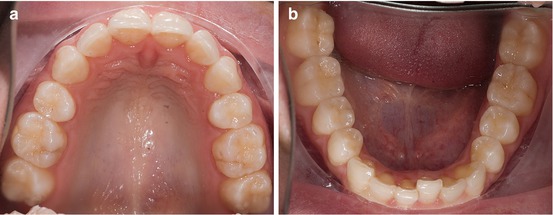
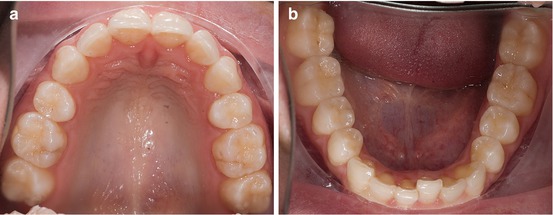
Fig. 2.3
(a, b) Upper and lower arches before treatment
No brackets were placed in the maxilla.
The goal of the treatment was to correct the lower anterior crowding without any extraction.
Lingual brackets were indirectly bonded with a setup technique.
After the initial alignment phase with a 0.0155″ coaxial arch, a Ni-Ti archwire 0.014″ was placed. Two months later, stripping between the lower incisors was progressively performed during eight visits (8 months) (Fig. 2.4a, b).
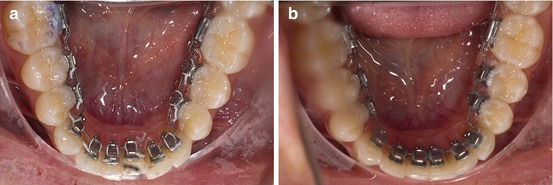
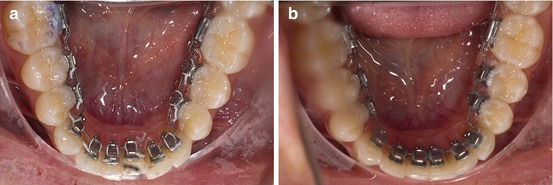
Fig. 2.4
(a, b) Before and after lower anterior stripping
These are the diamond single-side strips and the composite polishing strips that were recommended by the authors (Fig. 2.5a, b).
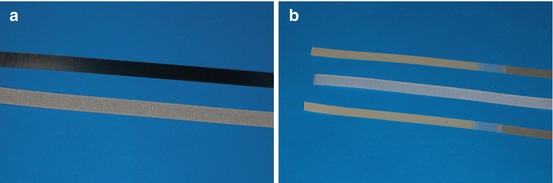
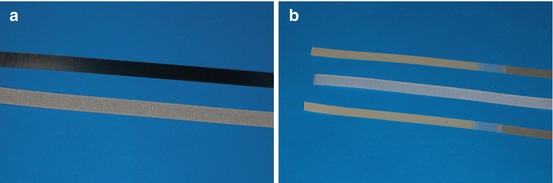
Fig. 2.5
(a, b) Different types of diamond and polishing strips
The final arch was a 0.0175″ × 0.0175″ TMA archwire for 3 months, and after that, the patient was ready for debonding.
It is important to remember that the fixed retention wire has to be placed the same day the brackets are removed (Fig. 2.6a, b).
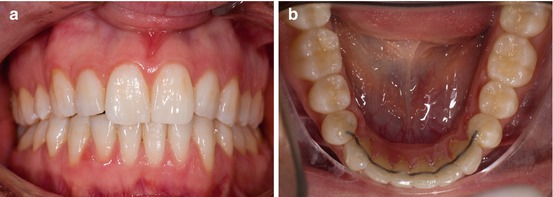
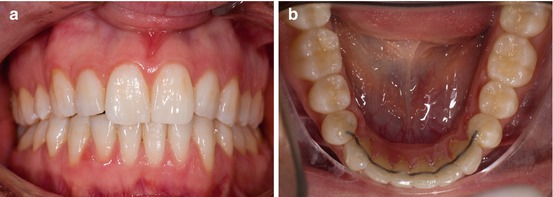
Fig. 2.6
(a, b) Final front photograph and lower fixed retention in place
The original mild crowding was corrected and the overbite was improved.
At the end of the treatment, the patient showed no signs of gingival inflammation, the midlines were coincident, and the papillae were totally recovered.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


