Inheritance
Magnitude
Definition
Syndromic
Hypodontia
Less than six teeth absent
Nonsyndromic
Oligodontia
Six or more teeth absent
Anodontia
All permanent (and/or deciduous) teeth absent
When considering the nonsyndromic forms of selective tooth agenesis, agenesis is reported to affect any of the permanent teeth with varying prevalence that is variable among different populations and races [16]. The most commonly missing teeth include third molars (excluded from definitions of oligodontia and hypodontia), mandibular second premolars, and lateral incisors. Current estimations suggest that hypodontias affect approximately 7–8 % of the population and oligodontias are displayed by less than 0.5 % of the population [15]. Reports of anodontia are extremely rare.
Nonsyndromic selective tooth agenesis represents the most common form of congenital tooth agenesis. It has been classified as either sporadic or familial and is inherited in autosomal dominant, autosomal recessive, or X-linked modes [5]. The observed clinical diversity underscores the considerable variation in both penetrance and expression. Nonsyndromic selective tooth agenesis commonly affects the secondary dentition; rarely is it observed in the primary dentition (Fig. 4.1). This finding has many implications for clinical management. Principally, the management begins with evaluation and treatment of the primary or mixed dentition while considering the needs of the adolescent and young adult patient. When managing patients with developmentally missing teeth, it is critical to have in mind both the short-term and long-term goals as you set forth on a treatment trajectory. The clinician should always have a vision for what future treatment may be necessary to achieve those goals.
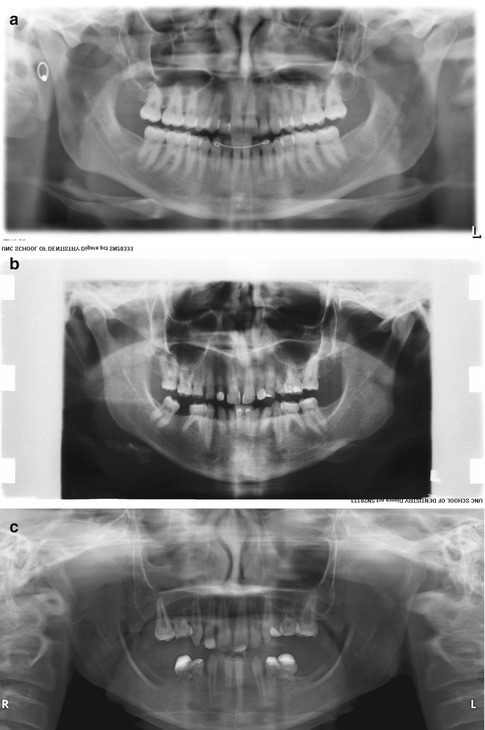
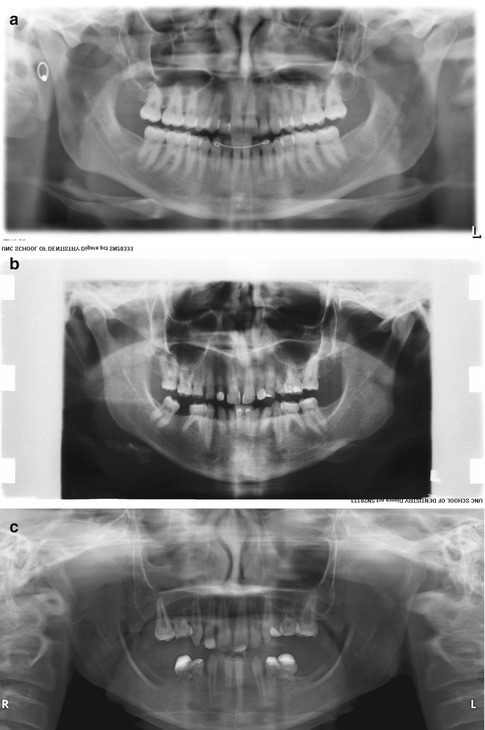
Fig. 4.1
Diversity of nonsyndromic tooth agenesis represented in young adults. (a) Panoramic radiograph reveals absence of the right maxillary lateral incisor tooth and a peg malformation of the maxillary left lateral incisor. (b) More extensive agenesis with only 14 permanent teeth present. Note that the management has involved the retention of mandibular lateral incisors and canine teeth as well as molars. (c) Extensive tooth agenesis revealing the presence of 12 permanent teeth with malformation
The Molecular Basis of Nonsyndromic Selective Tooth Agenesis
Agenesis of one or more teeth is a result of errors in the earliest processes of development. The first morphological cues are found in the thickening of the oral epithelium to form to dental lamina, and the inductive, tooth-forming potential arises from the dental ectoderm. The next steps, now directed by the dental mesenchyme, lead to the formation of the epithelial bud, and shortly thereafter the enamel knot is formed and reacquires directed control of morphogenesis. Subsequently, the cap stage is recognized and progresses by mesenchymal-epithelial interactions to the bell stage in which fully committed ameloblastic cells and odontoblastic cells surrounding the dental papilla follow a complex genetic program leading to complete tooth development [17, 26]. The mesenchymal cells differentiate into odontoblasts. The opposing epithelial cells differentiate into ameloblasts.
The morphologic description of tooth development (proceeding from dental lamina, to bud, to cap, to bell stages) is temporally associated with a pattern of regulated gene expression. Prominent among these events is the expression of regulatory molecules that play key roles in differentiation and development. Evidence of the roles that specific genes play in the location, size, shape, and number of teeth has come from genetic investigations conducted in mice [21, 22]. Many others have recently reviewed the remarkable molecular events that direct the formation of teeth [27]. Over 300 genes, many of which encode growth factors, transcription factors, or receptors, have been identified to contribute in this process [22]. By way of a brief summary, several specific known genetic alterations have been associated with nonsyndromic selective tooth agenesis (Table 4.2).
Table 4.2
Gene mutations associated with nonsyndromic selective tooth agenesis
|
Gene
|
Phenotype
|
Inheritance
|
|---|---|---|
|
MSX1
|
Hypodontia
|
Autosomal dominant
|
|
Oligodontia
|
Autosomal recessive
|
|
|
PAX9
|
Molar hypodontia
|
Autosomal dominant
|
|
Oligodontia
|
||
|
AXIN2
|
Incisor agenesis
|
Autosomal dominant
|
|
EDA
|
Hypodontia
|
X-linked recessive
|
|
LTBP3
|
Oligodontia
|
Autosomal recessive
|
|
WNT10A
|
Oligodontia
|
Autosomal dominant
|
Development is fundamentally regulated by homeobox-encoding genes that serve as master transcriptional regulators or genes that produce proteins that orchestrate the expression of other genes and their protein products. Included are MSX1 and MSX2. In tooth development, MSX1 gene expression contributes to early stages of tooth development. The disruption of Msx1 in mice causes developmental arrest of incisor and molar teeth [7]. Deletion, frameshift, and nonsense mutations of MSX1 (OMIM #106600 – STHAG1) in humans are associated with inherited forms of nonsyndromic and syndromic forms (Witkop syndrome – OMIM #189500) of tooth agenesis [19, 24].
PAX9 gene mutations are also associated with nonsyndromic selective tooth agenesis (OMIM #604625 – STHAG3). PAX9 is another homeodomain protein that directly activates the MSX1 gene. A central and early regulatory role in tooth development is evidenced in Pax9 homozygous deficient mice that lack all teeth for which development is arrested in the bud stage. Severe hypodontia in humans can be a result of PAX9 haploinsufficiency (one gene allele produces no functional protein, while the other PAX9 allele produces normal protein) [10] or different frameshift, deletion, missense, or nonsense mutations in the PAX9 gene.
The WNT gene family of morphogens is broadly active in human development, especially where mesenchymal-epithelial interactions are prominent such as the process exemplified by tooth development. Inhibition of the WNT pathway causes arrest of tooth development prior to the bud stage [1]. Wnt protein-induced signaling culminates in transcriptional regulation involving β-catenin. AXIN2 is a Wnt-signaling pathway protein that regulates β-catenin activity. Mutations of AXIN2 were found among individuals with different tooth agenesis patterns, and these individuals were identified to have an increased risk of colon cancer. Therefore individuals with AXIN2 mutations are considered as having oligodontia-colorectal cancer syndrome (OMIM #608615). Interestingly, Gardner syndrome (OMIM # 175100) is associated with supernumerary teeth and increased risk of colon cancer and results from mutations in the APC gene which also is in the β-catenin pathway. In a recent study, mutations in the WNT10A gene accounted for almost a third of selective tooth agenesis cases (STHAG4 – OMIM #150400) [3]. WNT10A mutations also are associated with syndrome-associated missing teeth (odontoonychodermal dysplasia, OMIM # 257980, and Schopf-Schulz-Passarge syndrome, OMIM #224750). Diverse mutations of inherited and spontaneous nature have been identified and lead to varying degrees of oligodontia and hypodontia [26]. The association of missing teeth with very diverse syndromes, some of which have significant other potential occult manifestations such as colon cancer risk, amplifies the need for obtaining a correct diagnosis of the etiology in all cases of selective tooth agenesis.
The more common forms of ectodermal dysplasias and related tooth agenesis conditions are due to mutations of the ligands, receptors, and signaling molecules along a tumor necrosis factor-related pathway represented by EDA (the ligand), EDAR (the receptor), EDARADD (signaling adaptor), the IKK gamma (NEMO) kinase, and WNT10A [8, 14]. However, a nonsyndromic X-linked mutation was associated with an EDA gene mutation expressed as the congenital absence of maxillary and mandibular central incisors, lateral incisors, and canines [11].
Other genes may be implicated in nonsyndromic selective tooth agenesis. Recently, LTBP3 (latent TGF-β binding protein 3) mutation was identified as responsible for an autosomal recessive form of familial oligodontia. Because genetic evaluation of individuals with oligodontia or hypodontia has not yet become fully integrated in the management of these individuals, it is likely that – with further screening – other genes and mutations will be identified as responsible for the spontaneous and familial expression of nonsyndromic selective tooth agenesis.
Clinical Diagnosis and Genetic Evaluations
The phenotypic expression of nonsyndromic tooth agenesis is varied and latent. A clinical evaluation of the primary dentition may reveal subtle or no clues to the developmental changes in the permanent dentition. An early clue may be retention of primary teeth and alterations in lateral incisor morphology. Nonsyndromic tooth agenesis may be inherited, and a dental history should include inquiry regarding family member dental status. When developmentally missing teeth are suspected then radiographic evaluation of the mixed dentition will ultimately reveal the absence of the affected teeth.
Once the developmental absence of permanent teeth is revealed, early collaboration among dental specialists is essential to develop short-term and long-term treatment objectives and goals. As the severity of tooth agenesis increases, attendant alterations in alveolar bone volume ultimately influencing maxillary and mandibular dimension can occur. A proper diagnosis must account for more global, skeletal changes associated with oligodontias.
Proper management of nonsyndromic tooth agenesis focuses on preserving teeth and the replacement of missing teeth for aesthetic, functional, and social reasons. The prevention of caries and periodontal diseases is paramount. Thus, a proper diagnosis must include a caries risk assessment and the subsequent management of this risk. The preservation of teeth and their possible orthodontic movement and strategic utilization are vitally important in the management of nonsyndromic tooth agenesis.
Interdisciplinary Treatment Plans
Management of individuals with nonsyndromic selective tooth agenesis reflects its impact on the dentition and the specific clinical phenotype. Because the deciduous teeth are less commonly affected by nonsyndromic tooth agenesis, concern and related management typically begins with the mixed dentition. In most cases, size discrepancies between retained deciduous teeth and the positionally related permanent teeth are significant. To avoid restorative complications and aesthetic limitations, coordination between pediatric, orthodontic, and prosthodontic specialists should be initiated early in the process of management. This will allow management of the patient’s aesthetic and functional concerns while planning for the definitive future treatment plan. Depending on the extent of tooth agenesis, there may be more general concerns. The management of one or two single missing teeth requires consideration of local factors related to the retention of the primary tooth, primary tooth removal, and space maintenance, as well as general concerns related to caries prevention and orthodontic tooth movement. When the expressed mutation results in a growing number of missing teeth, additional concerns regarding possible malocclusion, alveolar bone growth, and related craniofacial growth and development (in the absence of any syndrome) become important.
Recommended is an early evaluation of the patient and consultation by the pediatric, orthodontic, and prosthodontic specialist. In the mixed dentition phase, the prosthodontist should offer a possible therapeutic goal(s) for missing tooth replacement. Depending on patient and parent concerns, finances, and oral and systemic health factors, the solutions offered can involve orthodontic solutions, simple removable prostheses, tooth-supported fixed prosthodontic solutions, and, more commonly today, dental implant-supported fixed prosthodontic solutions.
The primary prosthodontic concerns are to (1) preserve all teeth and maintain ideal periodontal health during the transition period from a mixed dentition to a permanent dentition, (2) maintain ideal dental midline and occlusal plane orientations throughout treatment, and (3) maximize (not reduce) alveolar dimensions to create more ideal tooth positions and facial aesthetics for the final prosthetic plan in adulthood. To achieve these goals, the pediatric dentist must optimize caries control, especially during orthodontic intervention. The orthodontist must provide realistic estimations of the extent to which teeth may be moved to maintain natural tooth dimensions of edentulous spaces and, in cases of oligodontias, how the reductions in alveolar dimension (both vertically and horizontally) may be influenced by orthodontics to reach or approximate an acceptable lower third facial height and to assist in providing acceptable maxillomandibular relationships. At this early period of intervention, the prosthodontist should help to guide treatment toward a clearly elucidated and invariant final therapeutic goal and provide interim solutions for aesthetic and phonetic (anterior) tooth replacement in the mixed dentition. An example of this early interaction, its outcome in the permanent dentition, and the eventual restoration is illustrated in Fig. 4.2.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



