Fig. 8.1
Scheme of the professional structure of a multi-/interdisciplinary craniofacial team
Management of Newborns with OFC
Immediately after birth, feeding instructions, counseling, diagnosis by a geneticist, and a pediatric consultation should be arranged for the family. The newborn will need a hearing test while in the hospital, and assessment of the cleft is also provided. In the case of wide clefts, lip taping can start immediately [31, 32] The American Cleft Palate-Craniofacial Association advocates cleft repair by 18 months in a normally developing infant [20]. The timing of palatal repair must consider the potential for speech delay if the repair is performed too late against the possible interference with normal craniofacial growth if performed too early. Certain centers support earlier repair to reduce the risk of velopharyngeal insufficiency, which has been shown to increase by 6 % for each month the repair is delayed beyond 7 months [33]. Surgical repair is a critical, time-sensitive event early in the care of patients with cleft palate; palatal integrity is essential during the key periods of speech development [34]. Parents of infants with OFC should begin discussions with a pediatric dentist to provide parental information and support; develop a strategy of caries prevention, growth, and development monitoring; and consider a referral to an orthodontist for presurgical infant orthopedics (e.g., nasal alveolar molding, NAM) when appropriate.
Nasal Alveolar Molding (NAM)
Nasal alveolar molding (NAM) is increasingly being used for treatment of orofacial cleft nose deformity before primary repair [35]. Nasal alveolar molding is used effectively to enable tension-free reconstruction of cleft lips and reshape the nasal cartilage and mold the maxillary arch before cleft lip repair and primary rhinoplasty. It provides esthetic and functional benefits of nasal tip and alar symmetry and improved dental arch form [35–37]. The conventional NAM protocol includes alignment and approximation of the alveolar segments, repositioning deformed nasal cartilages, effective retraction of the protruded premaxilla, and lengthening of the deficient columella to achieve surgical soft tissue repair under minimal tension, with optimal conditions for minimal scar formation and increased nose symmetry [35–43]. NAM has significantly enhanced the ability of the interdisciplinary team to improve and maintain adequate nasolabial esthetics after the primary lip/nasal surgery in children with orofacial clefts. Infants are evaluated as early as possible, ideally within the first 2 weeks of life.
After the infant is examined to investigate whether any respiratory difficulties exist and to ensure that he/she is in good general health, the orthodontist/dentist takes an impression of the maxillary arch using an impression tray of acrylic resin that is slightly larger than the maxillary arch (Fig. 8.2). This is chosen from a collection of variously sized trays made from previously obtained maxillary dental casts. After the impression is taken, a stone cast is obtained from the impression and duplicated. The original cast is preserved for the patient record, and the second cast is used for fabrication of the appliance. A palatal plate is made of light-cured or thermo-cured resin, and the modified nasal stent is then added to the plate [35, 44, 45]. On the delivery appointment, the appliance is fit to the maxillary arch; a retentive loop is placed at the distal end of the wire; and a small piece of light-cured resin is cured to the tip of the nasal stent. Once the appliance is adjusted, the parents or guardians are given detailed oral and written instructions for placement, removal, and care of the appliance. They are also instructed to look for signs of irritation caused by the prosthesis. The appliance is retained with denture paste adhesive.
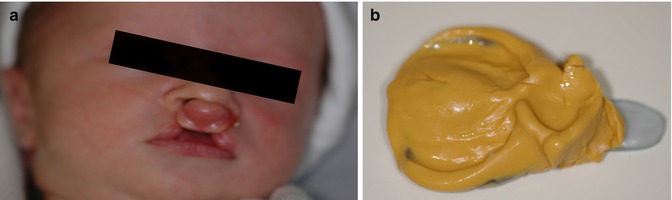
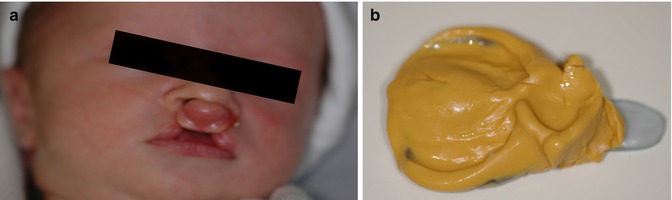
Fig. 8.2
(a) A 2-week old child with bilateral complete cleft lip and palate. (b) Impression in preparation for NAM
The patients are followed weekly for adjustments; nasal and alveolar moldings are initiated at the same time. Adjustments are made to improve comfort, guide alveolar segments’ reposition, and readjust the molding pressure on the nasal cartilage. The goals are, initially, to lengthen the deficient columella and to reposition the apex of the alar cartilages toward the tip of the nose and, later, to maintain the achieved morphologic changes. The appliance is worn continuously except for cleaning after feeding until cleft lip surgery is performed, usually at age 3 or 4 months. Timing for surgery may be guided by the progress of nasal and alveolar molding [46].
Management of Toddlers and Preschool Children with OFC
OFC children often experience issues with feeding, swallowing, esthetics, and poor oral health [47, 48]. The American Academy of Pediatric Dentistry recommends that during this period, it is important to inform parents and/or guardians how important it is to establish a dental home for all infants, children, adolescents, and persons with special health-care needs. Establishing the dental home is initiated by the identification and interaction of caregivers and family members, resulting in a heightened awareness of all issues impacting the patient’s oral health.
It is recommended to establish a dental home when the first primary tooth erupts in the mouth or within the first year of age. Ideally, parents should contact a dental clinic where comprehensive, continuously accessible, family-centered, coordinated, compassionate, and culturally effective care is available and delivered or supervised by qualified child health specialists. Preventative strategies can be implemented at this period with oral hygiene instructions, diet counseling, and application of fluoride varnish. The water source also needs to be evaluated (well or city water) to assure ideal levels of fluoride in water. Fluoridated tooth paste can also be used, but in a limited amount (a grain rice size smear until 3 years of age) so the child will experience the benefits of fluoride in dental caries prevention with a reduced risk of enamel damage due to dental fluorosis [49, 50]. Limitation in frequency and sugar-based food intake is very important to reduce the risk of developing dental caries [51]. It is recommended that until 6 years of age, sweet milk (such as chocolate milk), sodas, and juices should be limited to no more than 4 oz per day, and ideally children should drink these beverages at main meals and have their teeth clean afterwards.
In summary, pediatric dentists would continue working with strategies for preventing dental caries, diet counseling, perioperative care, infant orthopedics when indicated, and growth and development monitoring and provide surgical and restorative care if necessary.
Tooth Development in the Cleft Region
Subjects with OFC have been found to have a higher prevalence of dental anomalies, such as variations in tooth number and position and reduced tooth dimensions, predominantly localized in the area of the cleft defect [52–54]. Also, a higher prevalence of enamel discoloration in children with OFC has been found when compared with a normal control group; this defect has been mainly attributed to trauma at the time of cleft surgery [55]. Hypodontia of the cleft-side permanent lateral incisor (49.8 %) and delayed root development in comparison with the contralateral tooth are also common issues reported in OFC subjects [53]. Therefore, the dentists should explain to parents and guardians the potential problems associated with missing teeth and the orthodontic/prosthetic possibilities for habilitation in the future.
Management of School Children with OFC
In addition to anticipatory guidance and preventative care already provided at preschool age, pediatric dentists will provide surgical and restorative care for OFC children as needed. Children with clefts are at a significant risk for caries of the primary incisors [56]. The prevalence of dental caries in the deciduous dentition was found to be greater in a group of children with OFC compared to children with OFC [57].
Children in the mixed dentition should be evaluated for determining optimal timing for secondary alveolar bone grafting. Patients with cleft lip and palate have a bony deficiency in the tooth-bearing alveolar region of the palate. To repair this bony deficiency, secondary alveolar bone grafting is carried out to provide adequate periodontal and bony support in to which the canine can erupt [58]. The ideal time for performing alveolar bone grafting in patients with OFC varies. However, grafting is highly successful in subjects with age ranging from 9 to 12 years and when the canine root is one fourth to one half formed, which means, before canine eruption [59, 60]. After surgery, canines in the cleft area will present normal root development in most cases with spontaneous eruption through autogenous bone grafting. Also, it can be expected that the canines may erupt more slowly through the bone graft, and in some cases surgical and/or orthodontic intervention (exposure and bonding) will be required to complete eruption.
In patients with bilateral cleft lip and palate, the premaxilla projects itself up and forward in various degrees because it is separated from the maxillary processes, which can be collapsed or distant from each other. The teeth adjacent to the cleft can present a deficiency in the alveolar bone thickness and height, restricting the possibilities of orthodontic treatment. Depsit these developmental deficiencies and issues the teeth adjacent to the cleft often present with good periodontal bone support during the stage of mixed dentition [59, 61–63]. Buccal and mesiodistal orthodontic movement as well as rotational movements of maxillary anterior teeth before alveolar bone graft should be avoided or carefully conducted in these patients [63, 64].
Speech remains a critical consideration: when surgical correction is not an option or has to be delayed for medical reasons or by parent’s choice, then appliances can be fabricate to help with speech. Although surgery is the most frequently chosen approach for improving velopharyngeal function, a prosthetic device can be an option for some patients. These appliances are fabricated to be placed in the mouth, like an orthodontic retainer. Basically there are two types of speech appliances for children: the speech bulb and the palatal lift. When patients present with short palate, the speech bulb can be fabricated to partially close off the space between the soft palate and the throat [65, 66]. When there is inadequate palatal muscle function, even with appropriate palatal length, the palatal lift appliance can serve to lift the soft palate to a position that makes palatal closure possible [67]. It is recommended that prosthetic appliances be fabricated for children at least 5 years of age, and parents should closely supervise the use of these appliances [68, 69]. Children with submucous cleft palates (SMCPs) frequently suffer from delayed diagnosis that can result in poor speech outcomes. Furthermore, variability in the clinical severity of SMCPs can make treatment decisions challenging. Studies have established magnetic resonance imaging (MRI) as a reliable method to identify abnormalities in velopharyngeal muscle position, information that has potential to assist with treatment decisions (Fig. 8.3).
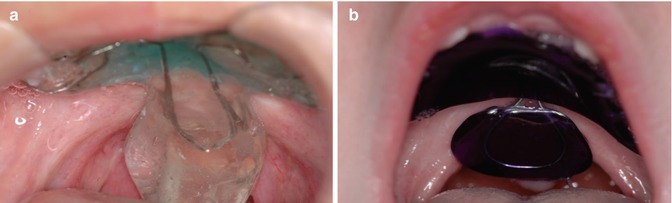
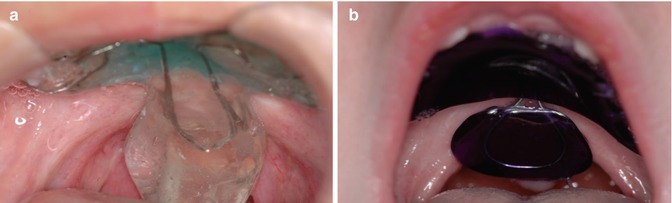
Fig. 8.3
(a) Palatal obturator in an 8-year-old child with short soft palate. Family would like to postpone surgical correction. (b) Palatal lift appliance of a 7-year-old child, appliance is used to help in elevating the palate to achieve palatal closure and reduce nasal air leakage
The pediatric dentist should work in coordination with orthodontists and oral maxillofacial surgeons in preparation for alveolar bone graft when necessary. They also will work with speech pathologists when a speech appliance is recommended and continue with measures for preventing dental caries and surgically remove primary teeth in surgical sites when indicated.
Management of Adolescents with OFC
Optimal management of patients with OFC is a continuous challenge. The surgical and clinical procedures carried out during infancy and childhood aim to create a foundation for development of normal speech, improvement of facial appearance, establishment of functional occlusion, and to strengthen self-esteem. However, there are reports showing that these early interventions can result in maxillary growth restriction that produce secondary deformities of the jaw and malocclusion, which also affect speech and self-esteem [70].
Adolescents with OFC not only have to deal with the developmental changes that naturally occur at this age, but also they must cope with special concerns common to their chronic condition such as: integrating their facial differences into an already changing body image, establishing interpersonal relationships despite possible dissatisfaction with facial appearance, relating to medical staff as young adults rather than children, and coping with surgeries that can alter and improve their facial appearance, but probably will not eliminate facial scarring.
Adolescents commonly recieve orthodontic treatment for alignment of their teeth and optimizing their occlusion. Additionally, they can have orthodontic treatment in preparation for orthognathic surgery that will occur at skeletal maturity. Orthognathic surgery is used to treat patients with cleft lip and palate who have a large skeletal class III malocclusion with variable degrees of anteroposterior, vertical, and transverse maxillary growth deficiency. Therefore, many of these patients will need orthognathic surgery at late teenage years when pubertal growth is complete.
During this phase, pediatric dentists and or general dentists have an important role in preventing dental caries and gingival inflammation by providing professional cleaning and oral hygiene instructions to the adolescents and their parents or guardians. Also, restorative treatment might be needed in cavitated caries lesions or in some cases for esthetic modifications of anterior teeth with resin composite direct restorations.
Management of Adults with OFC
There are still some adult patients with unrepaired OFC who will require oral care. Most of these individuals did not have a chance to have their clefts repaired surgically, or they presented with large clefts that could not be completely correct with surgical procedures, resulting in residual oronasal fistulas. Many of these patients are adults or elderly, and at their younger ages, there was no surgical alternative for repair, or they did not have access to proper care during childhood. In addition, they may have missing permanent teeth, deformed teeth, or even supernumerary teeth in the cleft area. Some patients reach adolescence or adulthood with unrepaired oronasal fistulas and alveolar clefts (bone discontinuity defects in the alveolus), even though the primary cleft defect has been repaired. The severity of residual deformities of the repaired cleft lip and nose may contribute to functional (mainly speech) and esthetic concerns. In adolescents and adults who have undergone cleft defect repair, common consequences include anterior and posterior crossbites; midface hypoplasia; anteroposterior, vertical, and transverse maxillary deficiency; residual lip and nasal deformities; and speech problems [73, 74].
Since orthognathic surgery (corrective jaw surgery) can affect significantly affect facial growth and development in patients with cleft lip and palate, end-stage reconstruction should be considered when these patients have reached skeletal maturity, which is usually age 15 years for females and 16–18 years or older for males [75–77]. If surgery is performed prior to completion of facial growth, the adverse effect on maxillary growth and continued growth of the mandible can result in recurrence of the facial deformity and malocclusion [76, 77]. In some cases, for esthetic and psychosocial reasons, surgery can be done at an earlier age with the understanding that it may need to be repeated after growth is complete [78–80].
Prosthetic Reconstruction
Adult patients who did not receive proper treatment for cleft palate are challenging for clinicians in terms of prosthetic rehabilitation. Moreover, during the late stages of adulthood when patients become edentulous, prosthetic reconstruction becomes even more challenging [81, 82]. Prosthetic rehabilitation requires adequate hard and soft tissue support. This aspect is of particular importance when the relationship of various anatomic structures is considered after reconstructive surgery [83, 84].
Patients who did not receive proper treatment for OFC often have several disorders such as: immature and collapsed maxillary arch, dysphagia, hypernasal speech, compromised chewing ability, palate with scar tissue, resorbed alveolar ridges, loss of vestibular depth, and oronasal fistulas. In addition, during the later stages of life when patients become edentulous, those issues related with OFC become troubling and more challenging in terms of prosthetic rehabilitation [81, 84].
Alveolar clefts are frequently associated with missing teeth [85, 86]. Management of the cleft after grafting involves either eruption of the canine in substitution for the missing tooth or tooth replacement using prosthetic means. Prosthetic methods include removable prosthesis, a fixed dental prosthesis (FDP), or a single tooth dental implant. The basic objectives of prosthodontic therapy include providing a comfortable, esthetically acceptable prosthesis that restores the impaired physiologic activities of speech, deglutition, mastication, and occlusion and preserving the remaining teeth and tissue [87].
Palatal Obturator
A residual oronasal communication (fistula) may be present even after surgical correction of the cleft in some cases. When that occurs, either on the palate or in the alveolar ridge or labial vestibule, they can result in speech, with undesirable nasal air emission or contribute to compromised articulation [88]. The main goal of a palatal obturator is to cover the fistula, to improve speech. Most of the time, it reduces hypernasality and corrects compensatory articulations.
The obturator can be used as a temporary appliance, while surgical correction is not possible or in some adult patients as a definitive prosthodontic appliance. As a temporary appliance, the obturator can be fabricated with resin acrylic, and it will cover the palate (palatal plate), and the retention is obtained with clasps fabricated with orthodontic wire. Most of the time, in those cases, the design will be similar to an orthodontic retainer.
However, in adult patients, when surgical correction is not an alternative, the prosthodontic obturator can be fabricated following the same principles applied for the fabrication of removable partial prostheses, with the metal infrastructure been fabricated with titanium or Co-Cr alloy [89] (Fig. 8.4). Removable prostheses are commonly indicated when clefts were not surgically closed, for oronasal fistula closure, and when a speech appliance is indicated [90, 91].
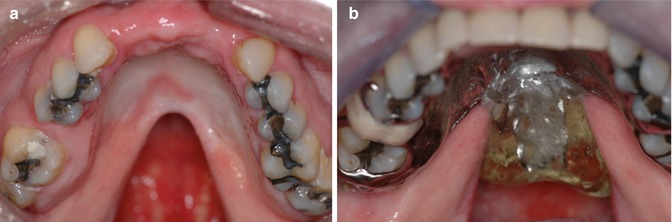
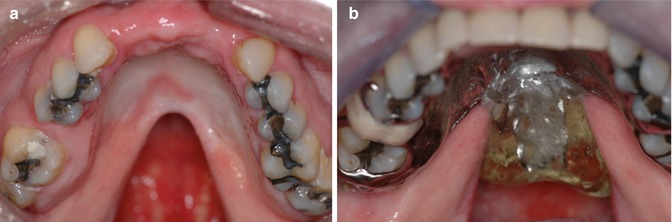
Fig. 8.4
(a) Adult patient with unrepaired V-shaped cleft of the hard and soft palate. (b) Partial removable prosthesis with palatal obturator repairing not only the cleft palate as well as missing teeth, resulting in functional and esthetic rehabilitation
Fixed dental prostheses (FDPs) have an historic basis, but present many limitations for managing OFC patients. A small cohort treated using FDP (n = 18) revealed no patients with failed teeth but a 22 % complication rate over an extended observation period (7.4–24.9 years). The authors contend that local conditions render implant placement difficult and conventional FDP therapy remains the treatment of choice. However, esthetic parameters and patient-reported outcomes were not defined [92].
While dental implants and three-unit FDPs share similar 10-year survival rates [93], the use of an FDP for the OFC patient requires a more complex FDP involving more teeth. Complex FDPs do not enjoy equally high survival rates and suffer far greater complications [94]. Endosseous dental implant therapy does not involve destruction of adjacent teeth for a fixed dental prosthesis (FDP) or involvement of removable prostheses. A single dental implant eliminates destruction of adjacent teeth for FDPs, potentially avoiding the greater risks reported for the larger FDP. Further, the use of FDPs without attendant regrafting of the alveolus is possible, but fails to structurally address the underlying tissue deficiency that support lip, alar, and general facial architecture.
Dental implants have been used for tooth replacement in OFC patients [95], but truly comprehensive assessments of this therapy have not been reported. Prospective studies of dental implant outcomes in OFC patients have typically involved fewer than 50 subjects and examined implant survival only general terms such as patient age, gender, and the type of cleft.
Future Directions
With the development of new technologies for early diagnosis of craniofacial anomalies, families could be informed about the orofacial cleft before birth. Molecular genetics advances and evaluation of families around the world have led to identification of the causative genes of numerous syndromes and conditions involving OFCs (e.g., Van der Woude syndrome OMIM #119300, ectrodactyly, ectodermal dysplasia cleft syndrome OMIM #129900). While high-resolution 2D scanning remains the cornerstone of prenatal diagnosis, new 3D approaches continue to expand our ability to assess the craniofacial complex and clefts prenatally with great accuracy than ever before. Early diagnosis allows parents, family members, and their friends to be better oriented about the management of orofacial clefts regarding the steps to be followed and the potential costs involved for therapy to adulthood. In addition, parents can be in contact with other families of children born with orofacial cleft to develop a network of support [96, 97].
Adjunctive therapeutic strategies based on tissue engineering are being developed that will improve soft surgical outcomes such as bone augmentation and muscle development to enhance palate function. New intervention methods for cleft repair using stem cells could bring new alternative treatments in the future [98]. However, the most important aspect of the treatment of children born with orofacial cleft is to provide comprehensive care that can be effectively provided by craniofacial teams. Cleft and craniofacial teams are widely seen as an effective mean to avoid fragmentation and dehumanization in the delivery of highly specialized health care [99–101].
References
1.
Grosen D, et al. A cohort study of recurrence patterns among more than 54,000 relatives of oral cleft cases in Denmark: support for the multifactorial threshold model of inheritance. J Med Genet. 2010;47(3):162–8.PubMedCentralPubMedCrossRef
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


