Ankylosis is the fusion between the mineralized root surface and the alveolar bone. Tooth trauma is a common etiologic cause of ankylosis. In young patients, the ankylosed teeth fail to erupt along with the remaining alveolar process during vertical facial growth, resulting in submerged teeth and defects in the alveolar process. Extraction of the ankylosed teeth followed by prosthetic replacement is a common option for treatment. This case report presents the treatment of a woman with an anterior open bite and an ankylosed central incisor due to replantation of a traumatized tooth. We treated this ankylosed central incisor with subapical osteotomy and distraction osteogenesis for better tissue regeneration. After active orthodontic treatment and prosthetic restoration, her open bite was corrected, and she had a harmonious smile line.
Ankylosis is defined as the fusion of the mineralized root surface (cement or dentin) with the alveolar bone. Tooth ankylosis can occur in the deciduous or permanent dentition. Several factors, such as endocrine or metabolic diseases, periapical infections, trauma, and previous surgical procedures, are possible etiologies of ankylosed teeth. Severe luxation injuries such as avulsion or intrusion, which compromise periodontal ligament integrity, are the major etiologies of permanent incisor ankylosis. Ankylosed central incisors at a young age can become a restorative nightmare in later years. As the alveolus grows around the ankylosed teeth, both incisal and gingival discrepancies occur. Upon loss of these teeth, due to internal and external resorption, a large alveolar defect can remain and be an esthetic concern for both the patient and the restorative dentist.
There are several methods to treat tooth ankylosis: surgical resection and replacement with a fixed prosthetic tooth, implants, space closure through orthodontic tooth movement, surgical luxation to attempt to break the fusion between the cementum and the bone, and surgical block osteotomies to allow rapid movement of a tooth or teeth with the block of bone. However, with a severely ankylosed tooth, the tooth cannot be moved the entire distance necessary to reach the occlusal plane because of the limitations of the adjacent attached soft tissue. Therefore, surgical osteotomies in a severely ankylosed tooth are often followed by distraction osteogenesis. Distraction osteogenesis is a biologic process of new bone formation. This bone formation is between the surfaces of the bony segments, which are separated gradually by incremental traction. Distraction procedures can be used to reconstruct alveolar and gingival deformities with high efficiency and predictability. Bone regeneration can be also accomplished by moving the precut sections in any of the 3 dimensions.
Diagnosis and etiology
A 21-year-old woman came to our orthodontic department with a chief complaint of an anterior open bite. She had no apparent medical problems; however, she had a history of facial trauma when she was 8 years old. Her maxillary left lateral incisor was missing at that time. Avulsion of the maxillary right and left central incisors occurred from this trauma. These teeth were replanted and fixed with wire and resin.
This patient had a slightly convex facial profile with a recessive chin. She also had insufficient lip closure and an asymmetric smile caused by ankylosis of the maxillary left central incisor ( Fig 1 ). Intraorally, she had Class I molar and Class II canine relationships on both sides, with 0.5 mm of overjet and a 9-mm anterior open bite. Her maxillary arch form was ovoid, and the mandibular arch form was square. The maxillary dental midline was 1 mm to the left of the mandibular dental midline, which was coincident with the facial midline. There were 5 mm of spacing in the maxillary arch and 1.5 mm of spacing in the mandibular arch. Anterior open bite and uneven gingival margin levels from the maxillary right lateral incisor to left canine were noted. Crown fracture and tooth discoloration were seen on the maxillary right central incisor ( Figs 2 and 3 ). Ankylosis, infraocclusion, minimal buccal plate, and thin-scallop gingival biotype were noted with the maxillary left central incisor. The ankylosed tooth was displaced 9 mm short of the occlusal plane. Lack of a periodontal space was noted radiographically surrounding the maxillary left central incisor root ( Fig 4 ). The residual ridge in the maxillary left lateral incisor area was thin, and there was no vertical development of the surrounding alveolar process and soft tissue from the maxillary right central incisor to the left canine.


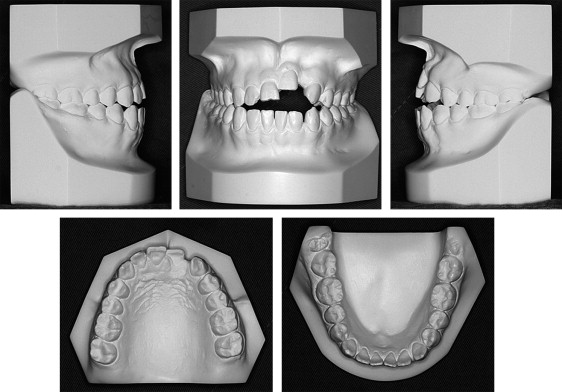
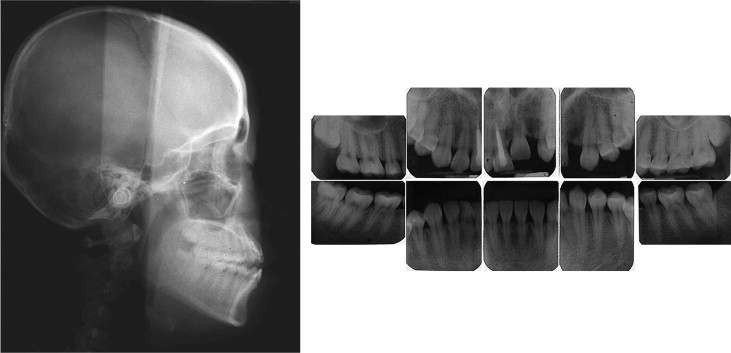
The cephalometric analysis ( Table ) showed a skeletal Class I relationship (ANB angle, 3°) and mildly recessive chin (Pg-NB, –1 mm) with an average mandibular plane angle (FMA, 25°). The maxillary and mandibular incisors were relatively proclined compared with the cranial base. The soft-tissue analysis showed a slightly retrusive upper lip position relative to Ricketts’ esthetic line (E-line, –3 mm) and a slightly protrusive position of the lower lip relative to the E line (E-line, 1.5 mm). The periapical radiographs showed that the maxillary right and left third molars and the mandibular right third molar were impacted. Normal root length and bone heights were present except around the ankylosed tooth ( Fig 4 ).
| Measurement | Norm | Pretreatment | Posttreatment |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 82 | 82.5 | 83 |
| A-N perpendicular (mm) | 3 | 3 | 3.5 |
| SNB (°) | 80 | 79.5 | 79 |
| ANB (°) | 2 | 3 | 4 |
| Wits (mm) | –1 | –3.5 | –2 |
| FMA (°) | 25 | 25 | 25.5 |
| PFH/AFH (%) | 66 | 65.3 | 65.1 |
| UAFH/LAFH (%) | 81.8 | 78.4 | 78.1 |
| LAFH (mm) | 71 | 73 | 74 |
| Pog-N perpendicular (mm) | 2 | –1 | –1.5 |
| Pog-NB (mm) | 2 | –1 | –1 |
| Dental | |||
| U1-SN (°) | 106 | 116 | 100 |
| U1-NA (°) | 25 | 33 | 16 |
| U1-NA (mm) | 5 | 6 | 5 |
| L1-MP (°) | 94 | 97 | 95 |
| L1-NB (°) | 25 | 34 | 31 |
| L1-NB (mm) | 5 | 9 | 9 |
| U1-L1 (°) | 128 | 110 | 129 |
| Soft tissue | |||
| Upper lip to E-line (mm) | 0 | –3 | 0 |
| Lower lip to E-line (mm) | 1 | 1.5 | 1.5 |
Treatment objectives
Our treatment objectives were to (1) correct the anterior open bite and dental midline by extrusion of the maxillary anterior teeth, (2) achieve a dental Class I relationship in the canines, (3) obtain a normal incisor relationship, and (4) improve anterior esthetics by correcting the alveolar and gingival margins in the ankylosed region.
Treatment objectives
Our treatment objectives were to (1) correct the anterior open bite and dental midline by extrusion of the maxillary anterior teeth, (2) achieve a dental Class I relationship in the canines, (3) obtain a normal incisor relationship, and (4) improve anterior esthetics by correcting the alveolar and gingival margins in the ankylosed region.
Treatment alternatives
The patient’s chief complaint was an anterior open bite, and it was mainly due to ankylosis of the maxillary left central incisor. There were 3 treatment alternatives for the ankylosed tooth: (1) extraction, (2) surgical luxation followed by orthodontic treatment, and (3) distraction of the tooth after single-tooth osteotomy.
Because the ankylosed tooth was in a high position with a thin buccal plate and a thin-scalloped gingival biotype, extraction of this tooth could have exaggerated the bone and soft-tissue deficiency. Moreover, it is an esthetic challenge to restore such a severe loss of bone and soft tissue in the maxillary anterior region.
Surgical luxation of this ankylosed tooth with an eruptive orthodontic force could also allow tooth movement. However, the tooth could reankylose even if the orthodontic force was applied immediately after surgical luxation. Therefore, a second surgery to loosen the ankylosed tooth would be needed.
Distraction of the ankylosed tooth after single-tooth osteotomy could bring the tooth and the adjacent alveolar process into the proper position. This procedure could solve the problems with the osseous and gingival margins. After the distraction and orthodontic treatment, a prosthesis could restore the maxillary anterior region to improve the patient’s smile.
After thorough deliberation of the advantages and disadvantages, the patient chose the third option.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


