40 Trauma-Induced Problems in the Salivary Glands
Introduction
Salivary gland trauma is uncommon and is usually associated with other injuries to adjoining structures. Owing to its relatively superficial location, the parotid gland is more prone to trauma in comparison with the submandibular salivary gland. Trauma to the parotid gland may be localized or may occur in concert with other polytrauma, as in road traffic accidents. In the latter scenario, the presence of other life-threatening issues may distract attention from parotid injuries. If parotid gland trauma is not recognized and dealt with promptly, some of the resulting complications can be a source of long-term morbidity. This chapter discusses the various types of trauma, describes pitfalls in clinical assessment, and suggests the best management options for acute cases and long-term sequelae.
Clinical Anatomy
The main trunk of the facial nerve is rarely susceptible to injury by trauma, and the relevant anatomy is discussed elsewhere in this book. This section deals with the anatomy as it pertains to the parotid duct and its interrelationships with some of the terminal branches of the nerve, as these structures are more prone to injury.
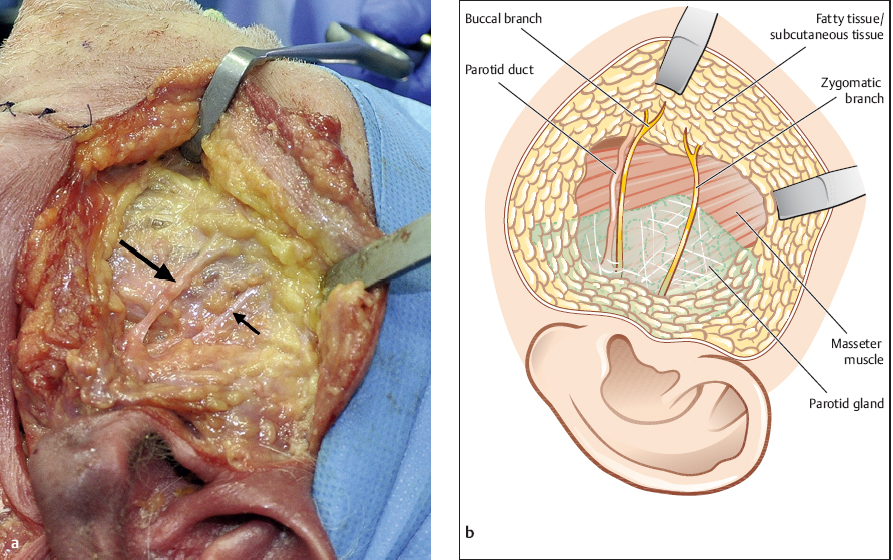
The parotid duct arises from the anterior aspect of the parotid gland. The vast majority of parotid ducts (93%) emerge from the anterior part of the gland as a single tributary; about 7% of the time, two large tributaries emerge from the parotid gland, forming the parotid duct 1 cm beyond the anterior border of the parotid gland (Fig. 40.1).1
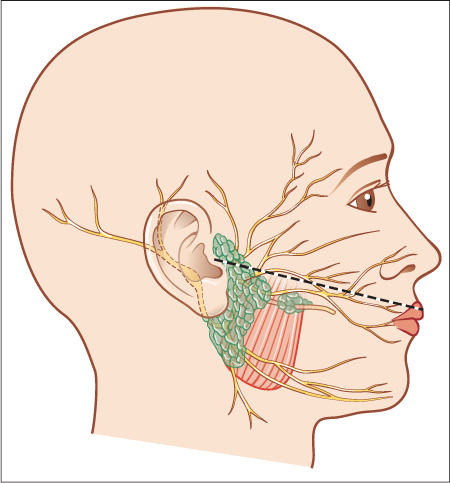
After exiting the gland, the duct runs anteriorly with the transverse facial artery, superficial to the masseter; this is a point at which it is most susceptible to penetrating facial trauma. At the anterior border of the masseter, the duct turns in a medial direction to pierce the buccinator and enters the oral cavity at the parotid duct papilla, seen opposite the second maxillary molar. The surface anatomy of the duct can be identified by the middle third of a line drawn from the tragus to the midpoint of the upper lip (Fig. 40.2). Penetrating trauma crossing this surface landmark should be considered to have potentially damaged the parotid duct.
The buccal branch of the facial nerve lies in close relation to the parotid duct. The buccal branch usually runs 0.5 cm below the parotid duct, in a more superficial plane.2 Anastomotic branches are frequent, and if present also travel superficial to the duct.1 The temporal branch and the marginal mandibular branch have no anastomotic branches and thus show a relatively lower rate of recovery if injured.
 The relationship between the anatomic landmarks and the site of injury allows analysis of the potential risk of salivary gland trauma.
The relationship between the anatomic landmarks and the site of injury allows analysis of the potential risk of salivary gland trauma.
Definition
Several types of trauma can cause injury to the parotid gland. Penetrating and blunt injury are common and usually occur in the setting of personal assault or road traffic accidents. Traumatic injuries to the gland and duct can also be seen secondary to facial cosmetic procedures, and pneumoparotitis occurs when air is forced up the ductal orifice.
Fig. 40.1 a, b a A cadaver dissection, showing that the buccal branch of the facial nerve is almost inseparable from the parotid duct (thick arrow). Distally, the nerve can be seen to veer away from the duct. The thin arrow indicates the zygomatic branch. b Schematic drawing of cadaveric specimen showing the parotid duct and the zygomatic branch of the facial nerve.
Penetrating trauma appears to be the major cause of salivary gland injury in the majority of reports.5 Penetrating trauma is more likely to present a management problem and lead to long-term sequelae, with a reporting bias in favor of these injuries. In this scenario, salivary gland injuries may be associated with other types of facial trauma. Facial rejuvenation procedures have also been reported to cause salivary gland and duct trauma.6 The nature of trauma can be secondary to compression of the duct caused by postoperative edema or direct surgical injury to the gland and/or the duct. Injury during the procedure is caused by poor attention to the plane between the superficial muscular aponeurotic system and the parotid capsule, and by the use of hooks. Unlike penetrating trauma, in which the injury is often limited to the site of penetration, the site and nature of the injury can be difficult to predict in this scenario, unless they are recognized during the procedure. Injury to the duct has also been reported following conventional and Mohs surgical excision of skin malignancies.7,8
Blunt trauma is uncommonly seen, and although it does cause injury to salivary acinar tissue, it is less likely to need active management. These injuries are less likely to cause problems, apart from self-resolving swelling and pain. However, radiological evidence of salivary dysfunction can be found following blunt trauma.9 Intraoral trauma to the duct orifice can occur due to cheek biting. Iatrogenic trauma to the duct or the parenchyma can occur during open surgical procedures on the gland. Forced entry of air through the parotid duct orifice can cause pneumatic trauma and subsequent inflammation. Radiation delivered to the region of the parotid gland, either to treat malignancies in the gland or if the gland lies in the radiation field for other tumors, can lead to radiation-induced trauma to the gland.
Fig. 40.2 The course of the parotid duct in the buccal region (on a line between the tragus and the midportion of the upper lip).
Epidemiology
The incidence of trauma-induced problems in the parotid gland varies significantly in relation to geographical location and socioeconomic factors. For obvious reasons, case series of penetrating trauma tend to be reported during times of war3 and from regions of conflict.4 Reviewing all published cases of post-traumatic late-onset sequelae in the parotid gland, Akinbami et al.5 identified 70 cases in the literature between 1963 and 2006. Some of the demographic data identified in this review suggested that these lesions were commoner in males in the majority of studies, with males representing 55–90% of the published cohort, with an age range in most studies of between 20 and 45 years.
Clinical Features
As trauma to the parotid gland can be seen in the setting of injury to other nearby structures, the clinical examination following a general survey should include the ear, eye, and maxillofacial skeleton. Blunt trauma to the parenchyma usually results in edema or hematoma. Thus, the most common presentation of blunt trauma to the gland is a swollen, painful gland. Facial weakness is rare in this setting. Minimal swelling and the absence of any other features suggesting injury to other structures do not warrant further investigations.
Diagnostic Work-Up
 Clinical Assessment
Clinical Assessment
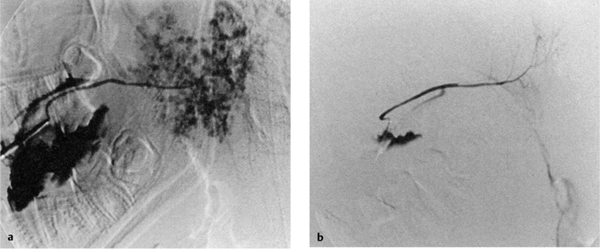
Investigation may be appropriate if the cheek is grossly swollen. In such cases, clinical assessment is difficult, and imaging will identify the presence of deep-seated hematomas, or rarely rupture of the acinar system. Computed tomography or magnetic resonance imaging will identify hematomas, and sialography is necessary to assess gland rupture (Fig. 40.3).
Fig. 40.3 a, b
a Left parotid sialogram, 24 hours after injury, showing an intact duct system but disruption of the normal acinar pattern. (Reproduced with permission of BMJ Publishing Group from Smith et al., Emergency Medicine 2001;18: 402–403.)
b Left parotid sialogram, 6 weeks after injury, showing normal anatomy. Other images in the series were also normal. Although they are less filled than in a, the acini are clearly visible, confirming that adequate pressure was applied when the contrast was injected. (Reproduced with permission of BMJ Publishing Group from Smith et al., Emergency Medicine 2001;18: 402–403.)
 Sialography
Sialography
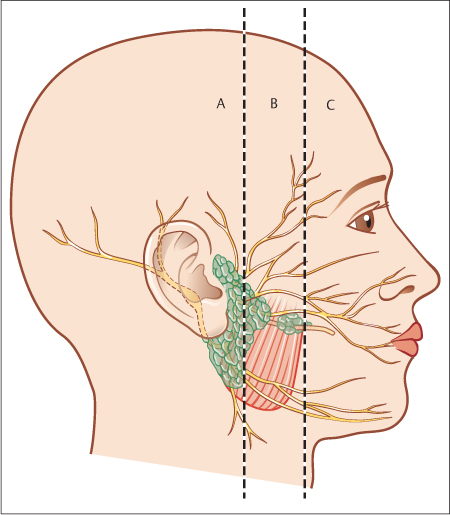
The duct is traditionally cannulated after dilation with a lacrimal probe, but this can be difficult in the presence of edema. A guide wire found in arterial line insertion packs can be used to aid this procedure, followed by railroading an 18-gauge or 20-gauge arterial cannula over the guide wire. The guide wire also makes it easier to negotiate a path through the curve of the duct where it pierces through the buccinator muscle. Care should be taken not to use too much dye, as this can stain the tissues. An alternative is to use other sterile fluids such as saline or propofol, which is readily obtained and has the advantage of being easily washed off.10 On the basis of the site of injury seen on exploration, Van Sickels has classified parotid duct injuries into three types11 (Fig. 40.4):
 Type A: intraglandular injury
Type A: intraglandular injury
 Type B: injury to the duct over the masseter muscle
Type B: injury to the duct over the masseter muscle
 Type C: injury to the duct anterior to the masseter, where it pierces the buccinator
Type C: injury to the duct anterior to the masseter, where it pierces the buccinator
Sialograms are less frequently used to diagnose parotid duct trauma, as good wound exploration combined with magnification makes this investigation unnecessary in the acute setting in many instances. It may be of use in scenarios in which ductal injury is missed on initial examination and the wound has been closed, leading to a collection of saliva (see below). Following their experience with a series of 51 patients with post-traumatic parotid fistula and sialocele, Parekh et al.12 classified the parotid injury into two types on the basis of sialographic appearances. This is shown in Table 40.1. This classification does have prognostic significance, in that destruction of a duct glandular junction (types 2a and 2b) takes longer to heal if managed conservatively (Table 40.1).
Fig. 40.4 The Van Sickels classification of parotid duct site injuries. A, glandular portion; B, duct over the masseter muscle; C, duct distal to the anterior border of the masseter muscle.
|
Type |
|
Glandular injury |
|
1 Glandular injury to the parenchyma or to the minor ducts |
|
2 Injury to a major intraparotid duct |
|
Ductal injury |
|
1a Partial transection of the parotid duct. |
|
1b Complete transection of the parotid duct |
|
2a Partial destruction of the parotid duct and gland junction |
|
2b Complete destruction of the parotid duct and gland junction |
 Facial Nerve Function Testing
Facial Nerve Function Testing
Facial nerve injury may occur to the main trunk or to the terminal or anastomotic branches. The facial nerve function should be documented, focusing on each of the five terminal branches. Although superficial trauma is unlikely to damage the main trunk of the facial nerve, deep penetrating trauma that occurs in the region of the retromandibular fossa in the posterior aspect of the parotid gland can potentially damage the main trunk. Injury to the buccal branch of the facial nerve can be quite subtle, with loss of the nasolabial fold and diminished mobility of the upper lip on animation. When the marginal mandibular branch is injured, the lower lip curls inward on smiling. In the presence of significant facial edema following the trauma, this may be quite difficult to recognize. The presence of facial weakness following blunt trauma is usually secondary to bruising of the nerve and the pressure caused by post-traumatic edema. The weakness should resolve, but electrical tests of function can be used for prognostication (see Chapter 39)
 Computed Tomography
Computed Tomography
Computed-tomographic imaging is necessary in all but the most minor injuries and is especially required in the presence of any of the complications mentioned above.
Treatment
 Blunt Trauma
Blunt Trauma
A superficial hematoma can be drained through a parotidectomy approach. In the absence of concurrent facial nerve weakness, deep-seated, intraglandular hematomas are best left to resolve spontaneously, as open drainage can put the facial nerve in jeopardy. If an infection occurs, open drainage may be necessary. Rarely, rupture of the gland can occur in isolation. Conservative measures to reduce salivary flow (anticholinergics) and supportive care are sufficient.
 Penetrating Trauma
Penetrating Trauma
Penetrating wounds are best surgically explored, and the management will depend on the findings at the time of exploration.
Parenchymal Injury
Penetrating parenchymal injury should be managed by wound exploration to exclude duct and facial nerve injury, followed by meticulous wound closure. Pressure dressing, antisialagogues, and stenting of the parotid duct (for the duration of the pressure dressing to prevent stenosis) have been variably recommended. The advantage afforded by these measures has not been confirmed, and it is very likely that the symptoms will resolve with symptomatic treatment alone.
Parotid Duct Injury
Partial duct transection should be repaired under magnification. In the event of complete transection of the duct, it is best repaired by primary end-to-end anastomosis using 8–0or9–0 nylon sutures; using microvascular clamps may aid the process. A suitably sized silicone catheter is best sutured to the buccal mucosa to serve as a stent and removed after 2 weeks (Fig. 40.5). There have been reports of successful repair of the duct without any stenting.13,14 If primary anastomosis is not possible owing to the loss of duct tissue, several alternative management strategies are available; these include diversion of the proximal segment into the oral cavity (Fig. 40.6), microsurgical repair of the duct with a vein graft,15 or using adjacent oral mucosa16 to tube the missing part of the duct and ligation of the proximal duct to cause glandular atrophy. If the last option is being considered, botulinum toxin can be used as an adjunct to reduce salivary secretion. There is experimental evidence for the success of vein grafts in the salivary duct in dogs,17 and this was shown to be successful in one case by Ananthakrishnan and Parkash.15 Sialendoscopic stenting of the transected duct after facial rejuvenation procedures has been reported,6 but experience is limited with this treatment modality at present.
If primary repair of the duct is not performed, resolution will occur, but healing is prolonged and complicated by the occurrence of fistulas and sialoceles. In a prospective study of 19 patients with parotid duct injury managed conservatively, Lewis and Knottenbelt reported that all cases resolved with conservative management; healing without complications was observed in only nine.18 Salivary fistulas occurred in seven patients and wounds and a sialocele occurred in four.
However, in certain types of trauma, especially with gunshot wounds, the extent of trauma may make any attempts at conservative treatment impossible and surgical repair of the wound may be the only option. Majid4 reported a series of 10 patients in whom duct repair was not undertaken following gunshot wounds; two patients developed salivary fistulas and one developed a sialocele.
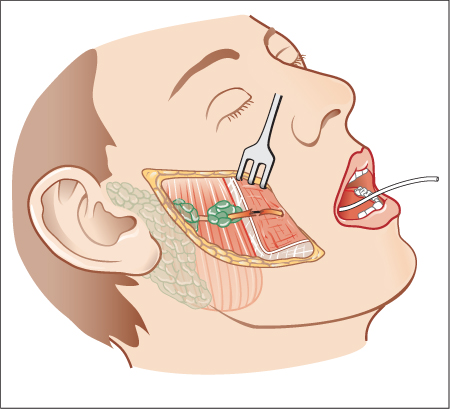
Fig. 40.5 Transoral stenting of the parotid duct to aid with freshening and suturing of the traumatized duct.
Facial Nerve Injury
The clinical presentation will dictate whether exploration in the main trunk or the branches is needed. This is best done under magnification, and if the nerve is seen to be in continuity, no further intervention is needed. End-toend anastomosis is performed if there is a complete nerve transection for the main trunk and the temporal and mandibular branches (further details on facial nerve repair are given in Chapter 38).
 Expertise in microsurgical techniques is an added advantage in dealing with penetrating injury to the parotid gland.
Expertise in microsurgical techniques is an added advantage in dealing with penetrating injury to the parotid gland.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses