18 Epidemiology of Benign Salivary Gland Neoplasms
Etiology of Benign Salivary Gland Tumors
Karolinska Hospital, Stockholm, Sweden
Memorial Sloan-Kettering Cancer Center, New York
The Armed Forces Institute of Pathology, Washington, DC
Incidence Reports of Benign Salivary Tumors
Introduction
Benign tumors of the salivary glands represent the majority of salivary gland diseases. Like malignant tumors, they are made up of a heterogeneous group of pathologies. The 2005 World Health Organization Classification describes 10 subtypes of benign salivary gland tumor, with some further subclassifications among these (see Table 20.1). Determining the true incidence of benign salivary gland tumors in populations is made difficult by the fact that there is no indication for establishing registries such as those available for malignant disease. Much of the literature discussed in this chapter therefore consists of case series from clinicians, institutions, or pathology databases. The chapter presents a brief examination of the pertinent positive findings in the literature regarding the etiology of benign salivary gland tumors, along with some epidemiological findings.
Etiology of Benign Salivary Gland Tumors
 Ionizing Radiation
Ionizing Radiation
Ionizing radiation exposure has been clearly identified as a risk factor for the development of salivary gland tumors.1–4 Case–control studies have shown that therapeutic radiation treatment to the head and neck region is associated with more than a doubling of the risk of developing salivary gland cancer.4 Individuals who received radiation to the scalp as children have been shown to have a 4.5-fold increased risk for developing salivary gland cancer.2 An increased risk of developing salivary gland malignancy has been reported in Japanese atomic bomb survivors in comparison with unexposed individuals.5–7 However, not all patients with salivary gland tumors have a history of exposure to ionizing radiation, and it is likely that a spectrum of susceptibility and predisposing genetic factors exists.8,9 In addition, some authors have concluded that among the benign tumors found in the exposed populations, there was an increasing trend, matching increasing radiation dosages, in the ratio of papillary cystadenoma lymphomatosum (Warthin tumor) in comparison with other benign salivary tumors.10
 Smoking
Smoking
There is controversy over the precise role of tobacco as a salivary gland carcinogen.11 In benign tumors, several studies have explored the role of smoking specifically in parotid gland tumors and found a significantly increased risk of developing Warthin tumors in comparison with other benign parotid neoplasms.12–16 A national case–control study in Israel examined smoking habits in patients diagnosed with parotid gland tumors and found that Warthin tumors comprised 25% of all tumors; 94% of those diagnosed with a Warthin tumor reported “ever smoking cigarettes.” There was no such link between the most common tumor, pleomorphic adenoma (50% of all cases in the study) and “ever smoking.”11 A further analysis by the same group17 examined the temporal relationship of smoking history parameters—age when starting to smoke and intensity, duration, and latency of smoking—to the risk of developing a Warthin tumor. The authors studied 117 patients with Warthin tumor and 336 matched controls. They found a strong positive linear effect of the duration of smoking and a positive nonlinear effect of the intensity of smoking, similar to effects reported for lung cancer.
 Cellular Telephones
Cellular Telephones
The rapid global expansion of mobile telephone use has alerted scientists to the potential dangers of radiofrequency electromagnetic fields produced by their antennae. The World Health Organization18,19 carried out a multicenter international study, the Interphone Study, to examine the incidence of intracranial tumors and salivary gland tumors and any link with cellular phone use. The study concluded that for brain tumors, there was no increase in the risk of developing a glioma or meningioma with the use of mobile phones. The study did not report outcomes relating to salivary gland pathology, but the authors concluded that the effects of long-term heavy use of mobile phones require further investigation.
Several studies have published both independent and national Interphone data. Results from Scandinavia examining Danish20 and Swedish21 populations demonstrate no consistent pattern of association between the use of mobile telephones and the development of salivary gland tumors. For regular mobile phone use, regardless of duration, the risk estimates for malignant and benign salivary tumors were 0.7 (95% confidence intervals, 0.4 to 1.3) and 0.9 (95% CI, 0.5 to 1.5), respectively. Similar results were found for more than 10 years’ duration of mobile phone use. The risk estimates did not increase, regardless of the type of phone and amount of use. The authors concluded20,21 that the data do not support the hypothesis that mobile phone use is related to an increased risk of parotid gland tumors.
Another study in Israel22 including participants with heavier use of cellular phones and with analysis relative to the side of the tumor and the side on which the phone was used reported an odds ratio of 1.52 (95% CI, 1.05 to 2.20) for all benign tumors and side of phone use and an odds ratio of 1.44 (95% CI, 0.99 to 2.09) for all benign tumors and heavy use. There is continuing controversy23,24 over a possible link between radiofrequency field exposure from mobile phone use and tumor risk, with issues including methodological problems relating particularly to inaccuracies and bias in recall of phone use.
 The role of cellular phones, especially with heavier use, as a risk factor for developing a benign salivary gland tumor is still unclear. There is no clear evidence to date that using cellular phones increases the risk for developing a benign salivary gland tumor.
The role of cellular phones, especially with heavier use, as a risk factor for developing a benign salivary gland tumor is still unclear. There is no clear evidence to date that using cellular phones increases the risk for developing a benign salivary gland tumor.
Classification
Diversity in the histopathological appearance of salivary neoplasms has led to several attempts to develop pathological classification systems. In 1953, Foote and Frazell46 published a report of almost 900 cases of salivary gland tumors and classified them into nine main histological types. As new pathological entities have been recognized over the years, several revised classifications have been proposed. The first World Health Organization (WHO) classification was published in 1972.25 However, new pathological variants continued to be described and a further update to the WHO classification of salivary gland tumors appeared in 1990.26 The most recent revision of the WHO classification27 was published in 2005 (see Table 20.1) and recognizes 13 types of benign salivary gland tumor.
Data and Site Distribution
The true incidence of benign tumors of the salivary glands will most likely continue to elude us. As there is no population-based registry system, there is heavy reliance on historic case series and reports from individual clinical and pathological institutions. In 1968, Thackray28 presented a useful approximation, based on experience in the United Kingdom, that for every 100 parotid tumors there will be 10 in the submandibular gland, 10 in the minor salivary glands, and one in the sublingual gland. He also commented that there are striking variations in the overall incidence of tumors and in the distribution of the histological types, with the proportion of frankly malignant growths being lowest in the parotid (15%) and highest in the minor salivary glands (60%).
As pathological data inevitably include only surgical cases, the number of asymptomatic benign tumors is probably underreported. Any busy clinician will testify to the growing incidence of “incidentalomas” that are found with modern imaging methods.29 The implications of this unmeasured disease for the true incidence of salivary gland tumors are not known. A number of historical large series investigating benign and malignant salivary gland tumors include valuable discussions of the histological types and sites of benign salivary tumors. More recently, smaller studies from around the world have investigated the trends and variations in this diverse group of diseases.
 The true incidence of benign salivary gland tumors is unknown, as no epidemiological registries for this tumor entity have been established anywhere in the world.
The true incidence of benign salivary gland tumors is unknown, as no epidemiological registries for this tumor entity have been established anywhere in the world.
 Karolinska Hospital, Stockholm, Sweden
Karolinska Hospital, Stockholm, Sweden
The Karolinska Hospital reported a series of 1985 benign salivary gland tumors30 collected from 1919 to 1969. The histological types described in the series were pleomorphic adenoma, papillary cystadenolymphoma (Warthin tumors), and oncocytoma. Most benign tumors reported were pleomorphic adenomas (n = 1658, 94%), followed by papillary cystadenolymphomas (Warthin tumors), (n = 105, 5.3%), and oncocytomas (n = 22, 1%). The most common site for benign salivary gland tumors was the parotid gland (n = 1780, 89.6%). One hundred and seven tumors (5.4%) were found in the submandibular gland and 98 (4.9%) in the minor salivary glands of the palate.
In the parotid gland, pleomorphic adenomas accounted for 1658 of 2158 tumors overall (benign and malignant; 77%). Warthin tumors represented 101 of the 2158 parotid tumors overall (5%). As only tumors located in the parotid gland, submandibular gland, and palate were reported, it is not possible to extrapolate the true distribution of salivary gland tumors from this series, as the sublingual gland and other sites in the head and neck were not included in the dataset. In addition, solid undifferentiated carcinomas and epidermoid carcinomas were included in the parotid salivary gland category, so that the overall data no not represent purely salivary gland tumors.
 United Kingdom
United Kingdom
Along with others, Eveson and Cawson31 set up the British Salivary Gland Tumor Panel in the early 1970s in order to provide a pathology service for nonspecialist pathologists working outside of tertiary centers in the United Kingdom and for clinicians requiring a second opinion on the diagnosis of salivary gland pathology, mostly neoplasms. They reported their experience of 2410 cases of primary epithelial salivary gland tumors during the period 1975–1984. Accurate anatomic sites and types of histological diagnosis—benign or malignant—were available for 2356 of the 2410 cases. There were 1756 parotid tumors, 1498 of which (85.3%) were benign; 257 submandibular tumors, 161 of which (63%) were benign; seven sublingual tumors, one of which (14.3%) was benign; and 336 minor salivary gland tumors, 180 of which (53.6%) were benign.
Jones et al.32 reported the distribution of salivary gland tumors recorded in a database in the Department of Oral Pathology in the Dental School in Sheffield, United Kingdom, between 1974 and 2005. The population is not clearly defined but is described as being drawn from hospitals in Sheffield and South Yorkshire, from the East Midlands region, occasional hospitals elsewhere, and general dental practitioners. It is therefore not possible to define the population basis for the data. The authors also note that in the period 1974–1994 they provided a diagnostic service for a surgical practice predominantly concerned with minor salivary gland lesions. A total of 741 salivary gland tumors were diagnosed, 481 of which (64.9%) were benign. Pleomorphic adenoma was the most common benign tumor, accounting for 329 cases (68.4%) and 44.4% of salivary gland tumors overall. Thirty-four of the benign tumors were Warthin tumors (7%), representing 4.6% of salivary tumors overall. Reporting bias complicates further analysis of these data, with a higher than usual proportion of benign tumors in the minor salivary glands (n = 283, 60%). The authors conclude that “in the last decade we have received more specimens from major salivary glands. This may be in part due to the formal establishment in the UK of the specialty Oral and Maxillofacial Surgery (OMFS) and the fact that more recently, ENT and general surgeons have probably carried out less salivary gland surgery. Therefore our results reported for major salivary glands may not accurately reflect the true distribution of salivary gland tumours in the general population.”
 Memorial Sloan-Kettering Cancer Center, New York
Memorial Sloan-Kettering Cancer Center, New York
Spiro reported on 35 years’ experience of salivary gland neoplasms at the Memorial Sloan-Kettering Cancer Center in New York.33 A total of 2807 patients received definitive treatment for salivary gland tumors, including 1966 with no previous treatment. Among the 1966 new patients, 1529 had benign tumors; 1062 of the benign tumors (69.6%) occurred in the parotid gland, while 92 (6%) arose in the submandibular gland and one (0.06%) was in the sublingual gland. Seventy-two of the 1966 tumors were in minor salivary gland sites (3.66%). The majority of the 1529 benign tumors were pleomorphic adenomas (n = 1274, 83.3%) and Warthin tumors represented 183 (11.9%) of the benign tumors found in the salivary glands overall.
 The Armed Forces Institute of Pathology, Washington, DC
The Armed Forces Institute of Pathology, Washington, DC
The largest series reporting the histological and anatomic locations of salivary gland disease is from the Armed Forces Institute of Pathology (AFIP),34 which presented a 45-year experience including more than 15 000 salivary gland tumors. Of the 13 749 epithelial salivary gland tumors, 8696 (63%) were benign. The most frequent site for the 8696 benign tumors was the parotid gland (n = 5566, 64%), followed by the submandibular gland (n = 725, 8%). Fourteen of the 8696 benign tumors (< 0.2%) were located in the sublingual gland. There were 2252 (26%) benign tumors located in the minor salivary glands. The majority of these 2252 lesions (n = 786, 35%) were located in the palate, 518 (23%) were found in the lip, 206 (9%) were reported in the cheek, 65 (3%) in the tonsil/oropharynx, and 25 (1%) in the tongue. Pleomorphic adenoma (mixed tumor) was the most common histological diagnosis, representing 6880 of the 8696 benign epithelial salivary gland tumors (79%). In the parotid gland, 4359 of the 5566 benign tumors (78%) were pleomorphic adenomas, representing 53% of parotid tumors overall (including mesenchymal tumors and metastases). Warthin tumors in the parotid represented 630 of the 5566 benign tumors (11%) and 7.7% of parotid tumors overall. Oncocytomas represented 156 of the 5566 benign parotid tumors (3%) and 1.9% of parotid tumors overall. Among 725 benign tumors in the submandibular gland, pleomorphic adenomas were the most common at 657 (91%), followed by oncocytomas (n = 18, 2.5%) and Warthin tumors (n = 16, 2%). Among benign and malignant epithelial tumors of the submandibular gland overall, pleomorphic adenomas represent 53%, oncocytomas 1.5%, and Warthin tumors 1.3%. Although these numbers are small, some interesting trends were observed, including a predilection for canalicular adenoma in the lip, representing 96 of 518 benign tumors (19%) in the minor salivary glands in the lip and 26% of minor salivary gland tumors overall.
 Brazil
Brazil
A review of salivary gland epithelial neoplasms by a group in the Department of Pathology at the Londrina Cancer Institute in Brazil identified 496 cases in the period 1972–2001.35 Among these tumors, 335 were benign (67.5%) and 161 (32.5%) were malignant. The most common site was the parotid gland (n = 336), followed by the minor salivary glands (n = 113) and submandibular gland (n = 47); there were no cases involving the sublingual gland. Pleomorphic adenoma was the most frequent tumor encountered, with 269 cases, representing 54.2% of all tumors and 80.3% of the benign tumors in the series. Warthin tumors were the second most frequent salivary gland tumor (12.5%), and all were located in the parotid gland. Only 42 of the 113 tumors in the minor salivary glands (37.2%) were benign, while 37 of the 47 submandibular gland tumors (78.7%) were benign. The peak incidence of benign tumors was in the fifth decade of life, with a slight predominance among women (58.5%).
Another study in Brazil reviewed 245 cases that were examined pathologically during the period 1980–1999 in the Pathology and Cytology Laboratory in Aracaju.36 Pleomorphic adenomas accounted for 168 of the 245 cases (68.6%), followed by Warthin tumors (n = 17, 7%) and canalicular adenomas (n = 2, 0.8%). The majority of the 187 lesions in the parotid gland were benign (n = 123, 65.7%), with pleomorphic adenoma being diagnosed in 106 of these cases (86.2%), followed by Warthin tumor in 16 (13.01%). Almost all of the 38 benign tumors in the submandibular gland were pleomorphic adenomas (n = 37, 97.4%), with one Warthin tumor. Two pleomorphic adenomas were located in the sublingual gland, and 23 of 24 pleomorphic adenomas (95.8%) were located in the minor salivary glands. Benign neoplasms occurred mainly in the second and third decades of life, with a predominance in women (114 of 168, 97.4%), while malignant neoplasms were mainly diagnosed in the sixth and seventh decades of life. The other interesting fact was that there was a predominance of salivary gland neoplasms among Caucasians, a finding that the authors considered difficult to interpret in view of variations in this ethnic group and the country’s significant miscegenation.
 China
China
For contemporary data, only the Chinese can rival the numbers reported in the historic series from the 1970s to 1990s described above. A 50-year series from western China describes 2069 benign salivary gland tumors.37 A total of 1449 of the 2069 benign tumors (70%) were in the parotid, followed by the palate (n = 343, 16.6%), submandibular gland (n = 238, 11.5%) and minor salivary glands (n = 34, 1.6%). Pleomorphic adenomas were reported in 1776 of the 2069 benign tumors (86%), Warthin tumors in 151 (7.3%), and basal cell adenomas in 58 (2.8%).
Tian et al.38 reported on a 23-year study including 6982 salivary gland neoplasms in an eastern Chinese population. In this series, 4743 of the 6982 lesions (68%) were benign tumors. Pleomorphic adenoma was the most common type, accounting for 69% (n = 3281) of the 4743 benign tumors, followed by Warthin tumor (n = 961, 20%). Basal cell adenoma and myoepithelioma represented 5% (n = 255) and 4% (n = 174) of the benign tumors, respectively, followed by cystadenoma (n = 28, 0.6%), oncocytoma (n = 23, 0.5%), and ductal papillomas (n = 10, 0.2%). Sebaceous and nonsebaceous lymphadenoma, canalicular adenoma, and sebaceous adenoma were rare, each accounting for less than 0.1% of all benign tumors. Among 3500 benign tumors in the parotid gland, 2126 (61%) were pleomorphic adenomas, representing 50% of parotid tumors overall, and 957 (27%) were Warthin tumors, representing 22% of parotid tumors overall. Interestingly, 92% of the Warthin tumors were found in males, possibly reflecting the population’s tobacco habits.
 India
India
A series of 684 patients were treated for salivary gland neoplasms at the Jawaharlal Institute of Postgraduate Medical Education and Research in Pondicherry, India,39 between 1991 and 2006; 422 of the patients (62%) had benign lesions. Most of the benign tumors were found in the 41–50-year-old age group (mean age 43 years). The male–female ratio was equal in both benign and malignant cases. Pleomorphic adenoma was the most frequently diagnosed benign tumor, with 203 of 253 lesions (80%) occurring in the parotid, 72 of 76 (94.7%) in the submandibular gland, one of two (50%) in the sublingual gland, and 87 of 91 (95.6%) in minor salivary glands. Other benign tumors identified included basal cell adenoma (n = 11), lymphadenoma (n = 5), cystadenoma (n = 5), oncocytoma (n = 4), and cystadenoma (n = 3), most frequently in the parotid gland and occasionally in the submandibular gland.
Incidence Reports of Benign Salivary Tumors
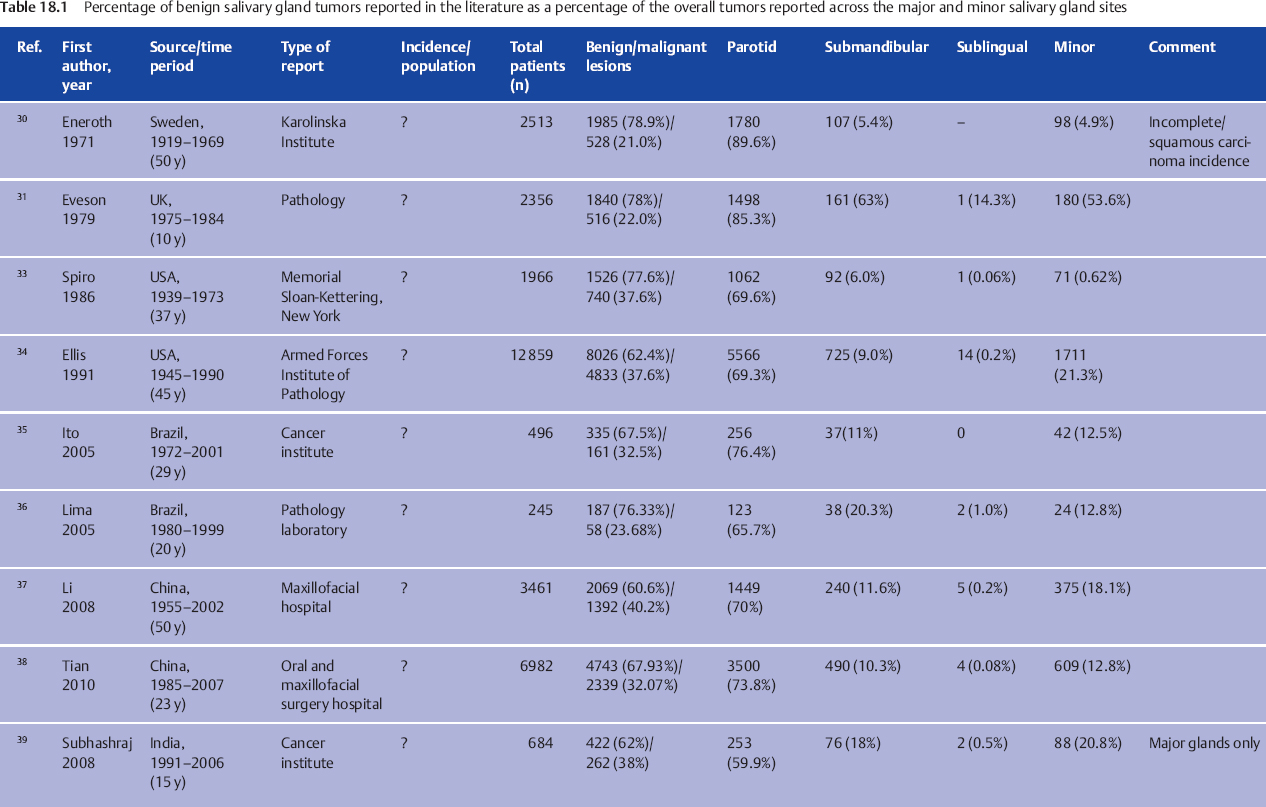
To allow reporting of the true incidence of neoplasms, a fixed population base relative to which the data are calculated is required (Table 18.1). The available data discussed above are from large tertiary surgical or pathology institutions which have a small, fixed population base. However, many of the referrals to such institutions are for clinical opinions or for histopathological diagnosis of specimens, and the data are consequently unsuitable for estimating the actual incidence. There are also no databases available, either regional or national, on benign neoplasms. The annual incidence of all salivary gland neoplasms is reported to be in the range of 0.4–13.5 cases per 100 000 population throughout the world, and it has been reported that 21.0%–36.8% of these are diagnosed as malignant.40 Calculating the annual incidence of benign lesions on the basis of these often-quoted figures would result in an extremely wide range of 0.25–10.66 per annum. An attempt to report the incidence was made on the basis of data held by the National Health Service in Scotland.41 The authors encountered difficulties due to many inaccuracies in the hospital discharge data on which the estimates were to be based. However, they estimated that throughout the five regions of Scotland, an overall incidence of more than four per 100 000 population can be assumed in the period 1968–1974.
 United States
United States
A report on the incidence of major salivary gland tumors in Jefferson County Hospitals, Alabama, between 1968 and 1989 attempted to overcome these problems.42 Medical records were reviewed for all cases of histologically confirmed epithelial tumors in the major salivary glands—parotid, submandibular, and sublingual glands—over the 22-year period. The authors found that 248 tumors (84.3%) were benign, with 181 (86.6%) located in the parotid gland, 28 (13.4%) in the submandibular gland, and no cases of either benign or malignant lesions in the sublingual gland. This gave an average annual incidence of benign major salivary gland tumors of 4.7 per 100 000 per year and an overall incidence of 5.6 per 100 000 per year. The authors concluded that “the true incidence rates may be underestimated, particularly those for benign tumors.”
 Denmark
Denmark
The incidence of major salivary gland tumors was calculated in a retrospective analysis of the salivary gland surgery performed and histopathology reports available on patients treated over the period 1984–2003 (20 years) in the county of Funen, Denmark.43 A total of 682 patients were identified; 621 (91%) had a benign tumor, 571 lesions (92%) were located in the parotid, 73 (11.7%) were located in the submandibular gland, and no benign tumors were located in the sublingual gland. This gives an incidence of major salivary gland tumors in the county of Funen of 7.3 per 100 000 population per year, which would give an estimate of the incidence of benign tumors of the major salivary glands of 6.6 per 100 000 per year.
 Poland
Poland
Another report on patients treated for parotid gland neoplasms in the province of Pomerania, Poland,44 in the 10-year period 1991–2000 identified 417 new cases. The most frequent benign neoplasm was pleomorphic adenoma (65.5%), followed by adenolymphoma (24.0%) and rarely basal cell adenoma (4.2%). A steady increase in the numbers of benign parotid tumors was observed during the period reviewed. The authors estimated that the age-standardized incidence rates were 0.23 and 1.35 per 100 000 population for malignant and benign tumors, respectively.
 United Kingdom
United Kingdom
In a “stable population” in Nottingham, Bradley45 has reported that the incidence of benign salivary gland neoplasm over the 20-year period 1988–2007 was 6.2–7.2 per 100 000 population. There were site-specific incidences of 5.3–6.2 for the parotid gland, 0.5–0.55 for the submandibular gland, 0 for the sublingual gland, and 0.47–0.5 for minor salivary gland sites. A total of 916 benign salivary gland neoplasms were diagnosed during the period; 649 (70.6%) were pleomorphic adenomas, 203 (22.1%) were Warthin tumors, 22 (2.4%) were basal cell adenomas, and 10 (1.0%) each were oncocytomas, monomorphic adenomas, and myoepitheliomas. Of the 649 pleomorphic adenomas diagnosed, 537 (82.7%) were in the parotid gland, 67 (10.3%) in the submandibular gland, and 45 (6.9%) in minor salivary gland locations. Of the 203 Warthin tumors diagnosed, 200 were located in the parotid gland and three were said to be located in the submandibular gland. The data used for these calculations were drawn from histopathology and fine-needle aspiration cytology reports for the 20-year period in a central pathology laboratory. All patients were residents in Nottingham’s four-hospital catchment area. The patients were managed in a variety of different specialities during the period: otorhinolaryngology/head and neck surgery (n = 603, 56.6%), oral and maxillofacial surgery (n = 266, 24.5%), general surgery (n = 117, 10.9%), plastic surgery (6.5%), and other specialties including pediatric surgery, dermatology, etc. (n = 11, 1.03%), due to shifts in clinical responsibilities. The majority of salivary gland neoplasms were treated by clinicians in otorhinolaryngology/head and neck surgery or oral and maxillofacial surgery.
 Parotid pleomorphic adenoma is the most common histological type and location for benign salivary gland tumors.
Parotid pleomorphic adenoma is the most common histological type and location for benign salivary gland tumors.
 Pleomorphic adenomas and Warthin tumors account for 69%–94% and 5%–29% of all benign salivary neoplasms, respectively. A benign parotid tumor will be a pleomorphic adenoma in 53%–77% of patients and a Warthin tumor in 5%–27%.
Pleomorphic adenomas and Warthin tumors account for 69%–94% and 5%–29% of all benign salivary neoplasms, respectively. A benign parotid tumor will be a pleomorphic adenoma in 53%–77% of patients and a Warthin tumor in 5%–27%.
 The parotid gland is the most commonly affected anatomic site, followed by the submandibular gland and then least commonly the minor salivary glands. Benign disease is extremely rare in the sublingual gland.
The parotid gland is the most commonly affected anatomic site, followed by the submandibular gland and then least commonly the minor salivary glands. Benign disease is extremely rare in the sublingual gland.
 Ionizing radiation and smoking are associated with an increased risk of developing Warthin tumors of the salivary glands. Warthin tumors are almost exclusively found in the parotid gland.
Ionizing radiation and smoking are associated with an increased risk of developing Warthin tumors of the salivary glands. Warthin tumors are almost exclusively found in the parotid gland.
 There is currently no evidence to suggest an association between the use of cellular phones or other devices generating local radiofrequency electromagnetic fields and the development of benign salivary gland neoplasms.
There is currently no evidence to suggest an association between the use of cellular phones or other devices generating local radiofrequency electromagnetic fields and the development of benign salivary gland neoplasms.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses