Chapter 36 Transpalatal advancement pharyngoplasty
1 INTRODUCTION
The ultimate goal of surgical treatment for obstructive sleep apnea (OSA) is to improve symptoms and eliminate disease morbidity and mortality. This is accomplished by altering airway sizecompliance and shape. Successful surgery eliminates collapseairflow limitation and airway obstruction during sleep. The precise features of successful versus unsuccessful surgery remain poorly understood.
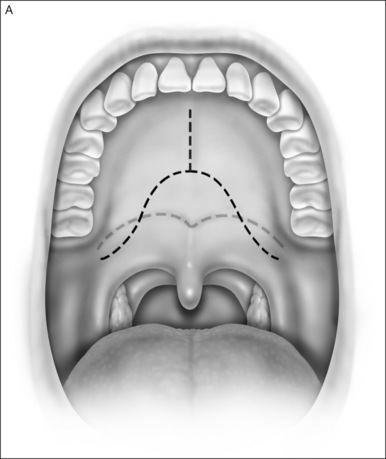
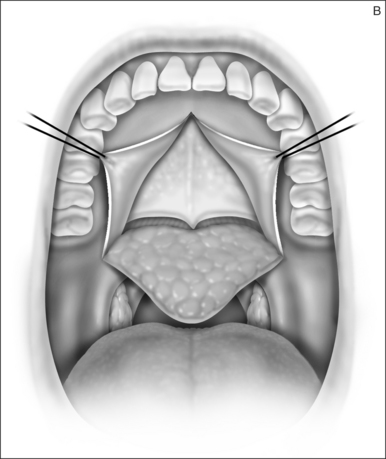
2 SURGICAL TECHNIQUE
2.1 EVALUATION
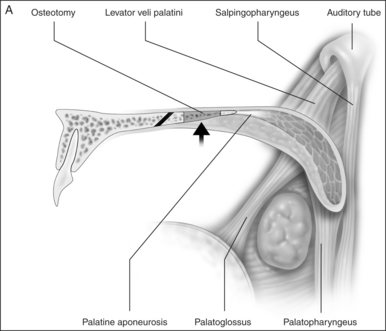
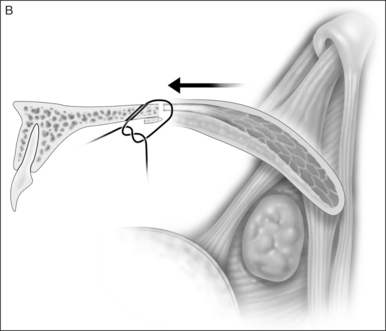
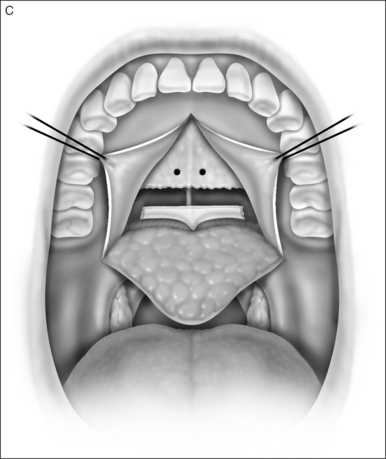
Preoperativelynasopharyngeal endoscopy is currently the primary method of airway evaluation and is performed in both a sitting and supine body position. Features evaluated include sizeshapeareas of collapseand pharyngeal swallow. During endoscopyclose attention is focused on the size and the shape of the proximal pharyngeal isthmus. Narrowing of the airway proximal to this point of estimated excision of traditional UPPP is an indication for primary transpalatal advancement pharyngoplasty. The shape of the pharyngeal isthmus indicates whether narrowing is from anterior–posterior compression (transversely shaped) or from collapse of the lateral walls (sagittally shaped). The locations of the levator muscle and palatopharyngeal sphincter are identified by visualizing the anterior fold of the torus tubarus (torus levatorius) which leads to the position of the levator muscle in the soft palate (Fig. 36.1). A narrow anterior to posterior airway at this level indicates retromaxillary airway narrowing. Such an abnormality cannot be addressed by traditional palatopharyngoplasty without aggressive excision of the levator muscle.
Evaluation of the oropalatal airway is also needed. Since the palate relative to the tongue base is pulled forward a small oropalatal airway space may be worsened. This requires additional surgery even if the pharyngeal retroglossal airway space is not severely abnormal. The oropalatal airway is assessed initially with routine oral examination. A modified Malampatti 1 or 2 position indicates excellent oropalatal airway space. Modified Malampatti 3 and 4 have a compromised oropalatal airway. Those patients with very small oral airways who are primarily mouth breathers need this segment treated prior to palatal surgery.