Transoral vertical ramus osteotomy (TOVRO) is a typical osteotomy procedure that is used for the backward movement of dentition in cases of mandibular sagittal excess. It has commonly been called intraoral vertical ramus osteotomy (IVRO) and is used more frequently in correcting temporomandibular joint disorder (TMD) than for actual purposes of orthognathic control of mandibular excess. Historically, two representative techniques for ramus osteotomy for orthognathic purposes—TOVRO and SSRO (sagittal split ramus osteotomy)—have been used for backward movement of the distal segment, which includes the dentition, chin, and body of the mandible. As is illustrated in Table 4-1 , various differences are evident between TOVRO and SSRO in terms of the osteotomy procedure, the mechanism of bone healing, the method of fixation between proximal and distal segments, intraoperative management of the condylar head, and the protocol of postoperative physiotherapy for mandibular function.
| SSRO | TOVRO | |
|---|---|---|
| Osteotomy | Posteroanterior sagittal split | Lateromedial cut |
| Open procedure | Blind procedure | |
| Along IANV | Rear to IANV | |
| Frequent exposure of IANV | No exposure of IANV | |
| Bone healing | Contact on marrow to marrow | Contact on cortex to cortex |
| Bone fixation | Rigid internal fixation | No fixation |
| Condylar head | Original position | New equilibrated position |
| Postop MMF | None or shorter period | Required (for 7 to 10 days) |
| Prognosis | Weakly dependent on PT | Strongly dependent on PT |
SSRO, which was originally developed by Hugo Obwegeser and was improved by Dal Pont and modified by Hunsuck and many other authors, is a widely used orthognathic procedure that can be applied for both forward and backward movement of the distal segment of the mandible. It is well known as the technique of choice for advancement of the distal segment without the necessity of a bone graft. However, when the inherent anatomic structure of the mandible is considered, SSRO may not be favorable for backward movement of the dentition. As is illustrated in Figure 4-1 , the mandible has a geometrically special architecture. When seen on the horizontal plane, it has a triangular shape by which the two condylar heads are connected to the corpus by right and left rami, which flare toward each condyle. Therefore, during the SSRO procedure, the cut surface of the distal segment can be moved forward in a narrowing direction toward the apex of the triangular architecture without any bony interference with the proximal segment ( Figure 4-2, A ).
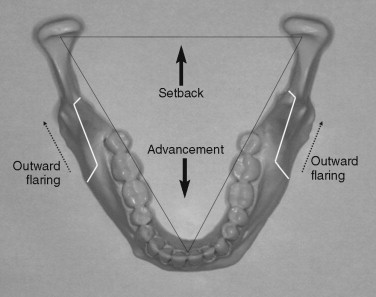
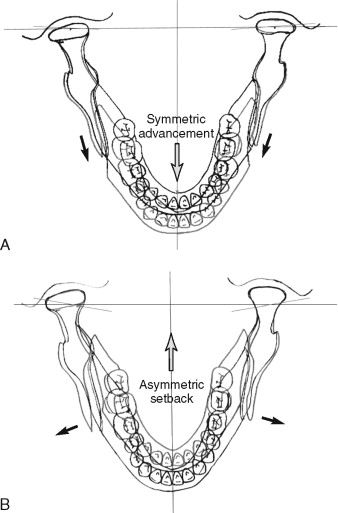
In contrast, during setback movement of the distal segment in SSRO, the cut surface of the distal segment inevitably faces bony interference with the cut surface of the proximal segment as it is moved toward the base of triangular architecture ( Figure 4-2, B ). To avoid such bony interference between the segments, the osteotomy line in BSSRO (bilateral SSRO) has to be parallel with the direction of setback movement, which is in fact impossible without injury to the inferior alveolar nerve (IANV), which runs mediolaterally from the mandibular foramen to the mental foramen within the ramus. Therefore, in cases of large backward or asymmetric repositioning of the distal segment in BSSRO, remarkable bony interference of the distal segment is inevitable and may result in wide bony gaps related to increased outward flaring of the proximal segments (see Figure 4-2, B ). In this situation, approximation of the two segments and stabilization with a rigid or semirigid fixation is very difficult. Unfavorable rigid fixation between segments can induce abnormal positioning of the condylar heads, which may result in irreversible TMD or postoperative relapse. Such stress from unfavorable rigid fixation increases as the severity of asymmetry or the degree of setback movement increases.
In the 1980s, several authors described unfavorable displacement of the condyle under rigid fixation in BSSRO. In contrast, Spitzer et al and Hackney et al reported favorable adaptation of the position and function of the condyle after BSSRO setback followed by rigid fixation. In addition, several authors have advocated that a modified technique of osteotomy and fixation in SSRO excludes the risk of TMD by placing the condyle in its proper position. Even these days, postoperative stability after BSSRO setback, its influence on TMD, and the functional adaptation related to the positioning and fixation methods of BSSRO setback are still in controversy. Nevertheless, our clinical experiences show that BSSRO setback frequently goes through unfavorable and perplexing postoperative consequences when a large setback greater than 10 mm or a remarkable asymmetric setback is performed.
TOVRO originating from the intraoral subcondylar osteotomy (ISO) was introduced by Moose (1964), and the current technique performed with Stryker’s oscillating saw was introduced by Winstanley (1968) and was modified by Herbert et al (1970).
Since the advent of TOVRO, many surgeons have tried to bind the proximal segment with the distal one using wires or screws, expecting a favorable bony union. On the basis of experimental research by Boyne and Reitzik, Hall described that the optimal situation for bony union after TOVRO would seem to be rigid fixation, with contact of cortical bone surfaces and decortication for the gaps between segments. However, nowadays, it is known that bony union occurs successfully through cortical overlapping without any means of intersegmental fixation, but with early allowance of mandibular movement within 2 weeks after TOVRO. In the experiment with adult dogs, bone healing between segments was observed when early mobilization of segments after vertical ramus osteotomy (VRO) was allowed. After TOVRO, the condylar head goes through immediate anterior and forward sagging, but it ultimately returns to its inherent position. Intersegmental fixation after TOVRO would be considered to have resulted in a prolonged open-bite tendency, which occurs as the condylar head position relapses back to its original position after immediate sagging. This also shows that any trial of fixation between segments in TOVRO can be hazardous, possibly leading to a postoperative open-bite tendency. Nowadays, intersegmental fixation is not recommended after TOVRO, and rather early release of maxillomandibular fixation (MMF) accompanying active physiotherapy is recommended. However, the required period of MMF has been variously applied from 1 week to 4 weeks; this is dependent on the surgeon.
ADVANTAGES AND DISADVANTAGES
TOVRO is an outpatient desk (OPD)-based procedure for backward movement of the prognathic mandible because it is very simple and quick. TOVRO has several advantages over BSSRO in various aspects. As was previously described, the inherent anatomic architecture of the mandible poses little interference on the cut surface of the TOVRO osteotomy site during mandibular setback, even in cases of severe asymmetry. In addition, because the segments are not fixed, no stress occurs while the distal segment is positioned with the condylar head during and after the osteotomy procedure. Moreover, TOVRO has less chance of damaging IANV during the osteotomy procedure than SSRO performed for the osteotomy cut line. In addition to advantages provided during the operation, this procedure has various postoperative advantages. It seems to have curable effects on most patients with preoperative TMD, in that it allows a physiologically equilibrated position of the condylar heads during the bone healing period ( Tables 4-2 and 4-3 ). It allows rapid recovery of mandibular function, which accompanies gradual and favorable esthetic changes of the lateral angle area in the mandible. In particular, long-term results on maintenance of the mandibular position and occlusion show the excellent postoperative stability of the TOVRO procedure.
| Preop | 1M | 3M | 6M | 12M | 18M | 24M |
|---|---|---|---|---|---|---|
| 158/434 | 14/434 | 29/420 | 26/396 | 23/256 | 17/156 | 10/112 |
| 37.3% | 3.2% * | 6.9% * | 6.6% * | 9.0% * | 10.9% * | 8.9% * |
| Click ( + )→( – ) | (−)→(−) 130 | Transient TMJ sound in 17 TMJs | ||||
| (149) | (−)→(+) 19 | 6M(13), 12M(3), 18M(3) | ||||
| Click ( + )→( + ) | (+)→(+) 4 | No improvement | ||||
| (9) | (+)→(−) 5 | Disappeared after POD #3M | ||||
| Click ( – )→( – ) | (−)→(−) 255 | No detectable TMJ sound | ||||
| (271) | (−)→(−) 16 | Transient TMJ sound | ||||
| Click ( – )→( + ) | (+)→(+) 1 | Remained still POD #12M | ||||
| (5) | (+)→(−) 4 | Disappeared after POD #12M | ||||
| Preop | 1M | 3M | 6M | 12M | 18M | 24M |
|---|---|---|---|---|---|---|
| 47/434 | 5/434 | 4/420 | 3/396 | 6/256 | 0/156 | 0/112 |
| 10.8% | 1.2% * | 1.0% * | 0.8% * | 2.3% * | 0.0% * | 0.0% * |
| Pain ( + )→( – ) | (−)→(−) | 40 | ||||
| (46) | Transient(+) | 6 | 3M(1), 6M(2), 12M(2), 18M(1) | |||
| Pain ( + )→( + ) | (+)→(+) | 0 | ||||
| (1) | (+)→(−) | 1 | Disappeared after POD #3M | |||
| Pain ( – )→( – ) | (−)→(−) | 375 | ||||
| (383) | Transient(+) | 8 | 3M(3), 6M(1), 12M(4) | |||
| Pain ( – )→( + ) | (+)→(+) | 0 | ||||
| (4) | (+)→(−) | 4 | Disappeared after POD #3M | |||
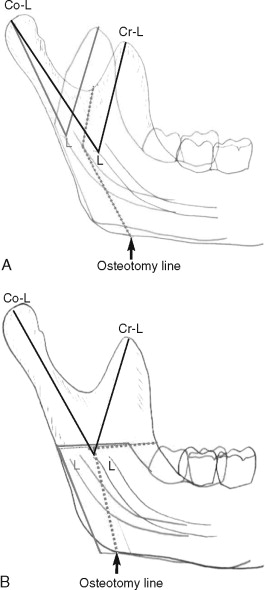
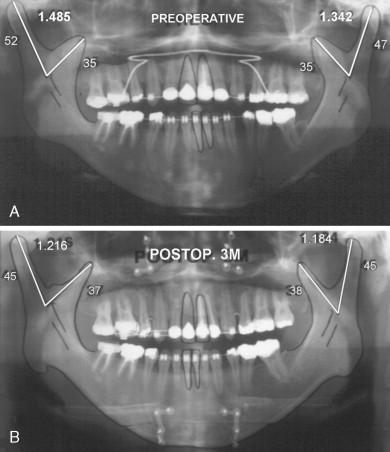
TOVRO also can be applied for the ethiopathogenesis of mandibular prognathism in cases of elongation of the condyle. In TOVRO, the osteotomy line vertically separates the condylar process from the coronoid process. In this way, the unbalanced lengths of the two processes, which are inadequate to act as one functional growth unit, can be harmonized through positional rearrangement of the two processes during setback of the distal segment ( Figures 4-3 and 4-4 ).
TOVRO offers many advantages, as has been discussed, along with a few disadvantages. The principal disadvantages of TOVRO include the need for MMF and the requirement of forcible physiotherapy by patients themselves. MMF is required for approximately 7 to 10 days after osteotomy, and application of the forcible and strict protocol of active physiotherapy is required for 1 or 2 weeks after release of MMF. Patients’ understanding and cooperation during physiotherapy are critically important during this period for a favorable treatment prognosis.
It is interesting to note that in spite of the many advantages of TOVRO over SSRO, TOVRO is not yet widely used for setback movement of the mandible. Many surgeons still prefer SSRO over TOVRO, and they choose TOVRO as the alternative to SSRO to treat patients with TMD or mandibular prognathism with remarkable asymmetry. Such a phenomenon seems to originate from a doubtful predilection about the prognosis for postoperative stability of TOVRO, which is based on poor previous experiences before the protocol for post-TOVRO management became available.
INDICATIONS AND CONTRAINDICATIONS
In most cases, no contraindication for TOVRO is noticeable in terms of the morphology of the mandibular ramus or the required amount of setback of the distal segment of the mandible. My clinical experience with more than 500 patients proves that interference during backward movement of the mandible does not depend on the amount of setback but on the degree of medial flaring or unfavorable thickness of the proximal part of the ramus. Such limitations can be easily overcome by reducing the medial volume of the proximal segment. Another limiting factor is the anatomic interference between the coronoid process and the skull base, or with the temporomandibular joint (TMJ) capsule when significant posterior impaction of the maxilla or significant setback of the mandible occurs concurrently. In these cases, coronoidotomy, a simple horizontal cut of the coronoid process above the mandibular foramen, is a useful modification that can be performed to prevent such interference. However, coronoidectomy, the removal of the coronoid process, should be avoided because it can impose difficulties in physiotherapy.
TOVRO should be considered for patients with previous TMJ disorder, except in cases of disk perforation or TMJ arthritis. Such preoperative TMD can be treated concurrently as the condylar heads freely move into a stable position through physiotherapy during the bone healing period after TOVRO. The most reliable advantage of TOVRO is that separation of the condyle from the corpus permits free repositioning of the condylar head until bone union between segments has been achieved. During this process, the condylar heads certainly go through initial sagging and torque for a while, but they gradually find their way into a physiologically equilibrated position. Concurrent remodeling occurs as well. In this manner, TOVRO provides an excellent treatment for TMD (see Table 4-2 ). Therefore, TMD treatment prior to TOVRO is unnecessary for patients with both TMD problems and mandibular prognathism.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


