In nongrowing patients with skeletal Class II malocclusion, premolar extraction or maxillary molar distalization can be used as camouflage treatment. Orthodontic miniscrew implants are widely used for this purpose because they do not produce undesirable reciprocal effects and do not depend on the patient’s cooperation. This article reports on maxillary molar distalization by using miniscrew implants to correct a Class II problem. The main considerations of molar distalization treatment with miniscrew implants are discussed.
The treatment options for nongrowing skeletal Class II patients include camouflage treatment and surgical correction. In a skeletal Class II patient having a short vertical dimension with no transverse discrepancies, it has been reported that an increase in the vertical dimension by orthognathic surgery or molar extrusion is unstable after a long-term follow up. Therefore, if there is minimal skeletal discrepancy, a camouflage approach maintaining the vertical dimension after extraction would be an appropriate treatment alternative for stable treatment results.
In camouflage treatment, the premolars are extracted to relieve crowding, correct protrusion, and establish proper occlusion. Creating space by stripping and correction of the Class II molar relationship with maxillary molar distalization would be an alternative treatment. Distalization of maxillary molars can be accomplished by using a pendulum appliance, a distal jet, or a headgear. Recently, miniscrew implants and miniplates have become widely used to treat Class II problems.
In this case report, miniscrew implants were used to distalize the maxillary molars, relieve the crowding, and establish a Class I molar relationship.
Diagnosis and etiology
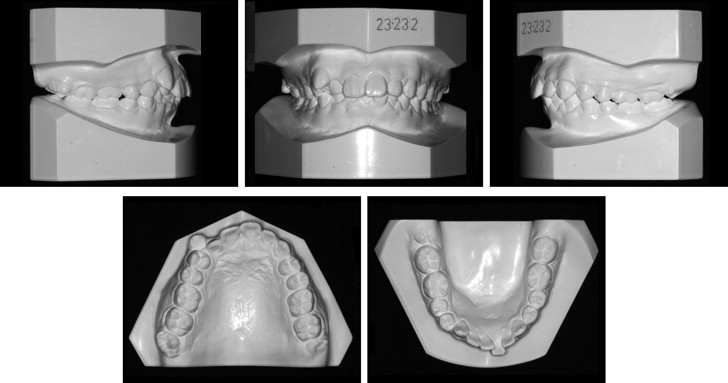
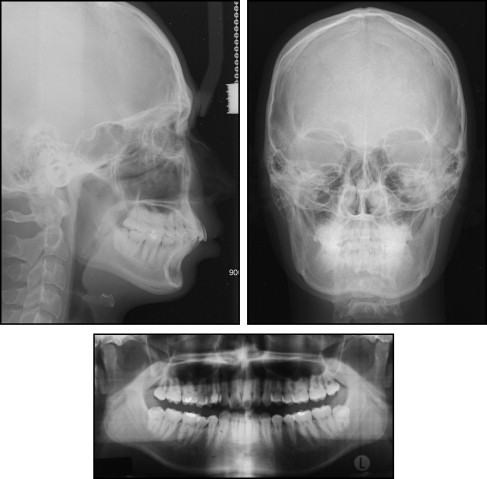
The patient was a 21-year old man with a chief complaint of dental crowding. The pretreatment facial photographs showed protrusion of both upper and lower lips, a deep mentolabial fold, and mandibular asymmetry around the chin area. This was the result of trauma when he was 6 years old ( Figs 1 and 2 ). In the frontal cephalogram, the chin was deviated to the left side, and an asymmetric mandibular lower border was observed. The lateral cephalometric analysis showed a Class II skeletal pattern with a low mandibular plane angle ( Fig 3 , Table ). The IMPA angle of 117.5° reflected a compensatory proclination of the mandibular incisors, although it was measured from the most labially positioned tooth, which was the left central incisor. The upper and lower lips were protrusive by 4.1 and 8.0 mm, respectively, from the esthetic line. The panoramic radiograph showed that both maxillary third molars were fully erupted, and the periodontal state was generally good. Molar relationships were Class II on both sides. The maxillary midline was 3.0 mm to the right of the facial midline, because of the ectopic right canine. The mandibular midline was 1.5 mm to the left of the facial midline with moderate anterior crowding. Overbite was 3.0 mm, and overjet was 2.5 mm. The Bolton tooth-ratio analysis (sum of incisors, 4:3.08; anterior ratio, 80.4%; overall ratio, 92.9%) indicated that the mandibular teeth were generally larger than the maxillary teeth.

| Measurement | Pretreatment | Posttreatment | 3 years of retention |
|---|---|---|---|
| SNA angle (°) | 86.6 | 87.2 | 87.0 |
| SNB angle (°) | 78.6 | 79.3 | 79.3 |
| ANB angle (°) | 8.0 | 7.9 | 7.7 |
| Wits appraisal (mm) | 7.1 | 5.8 | 5.5 |
| SN to mandibular plane (°) | 24.7 | 24.1 | 24.0 |
| Bjork sum (°) | 384.7 | 384.1 | 384.5 |
| U1 to SN (°) | 108.1 | 105.8 | 104.2 |
| IMPA (°) | 117.5 | 116.8 | 117.3 |
| U1 to facial plane (mm) | 16.2 | 11.8 | 12.1 |
| L1 to facial plane (mm) | 11.3 | 9.7 | 10.0 |
| Upper lip to Ricketts’ E-line (mm) | 4.1 | 1.7 | 1.6 |
| Lower lip to Ricketts’ E-line (mm) | 8.0 | 5.4 | 5.8 |
Based on these findings, the patient was diagnosed as skeletal Class II Division 1 with a hypodivergent profile and facial asymmetry.
Treatment objectives
The treatment objectives for this patient were to (1) relieve the crowding, which was his chief complaint; (2) correct the skeletal Class II facial asymmetry and hypodivergent profile; (3) establish Class I molar and canine relationships; (4) correct the midline shift; (5) create ideal overbite and overjet; and (6) ultimately establish a proper soft-tissue profile.
Treatment objectives
The treatment objectives for this patient were to (1) relieve the crowding, which was his chief complaint; (2) correct the skeletal Class II facial asymmetry and hypodivergent profile; (3) establish Class I molar and canine relationships; (4) correct the midline shift; (5) create ideal overbite and overjet; and (6) ultimately establish a proper soft-tissue profile.
Treatment alternatives
For the correction of the skeletal discrepancy and facial asymmetry, an orthognathic surgical treatment with extraction of the mandibular first premolars was initially discussed. A nonsurgical approach with extraction of the maxillary first premolars and the mandibular second premolars followed by genioplasty to improve his facial profile was also presented as an alternative. However, he refused all surgical treatments including premolar extraction and wanted only the crowding to be resolved. He was not interested in improving his occlusion and facial profile, and correcting the dental midline through orthodontic treatment.
Therefore, the treatment objectives for this patient were redirected to relieve crowding and maintain the sagittal position of the maxillary anterior teeth to prevent further protrusion of the upper and lower lips. With respect to the patient’s request, treatment alternatives excluding premolar extraction and orthognathic surgery were discussed.
The treatment plan involved molar distalization by orthodontic miniscrew implants after extraction of the third molars. This was because the treatment goal was to maintain the maxillary incisor position despite the severe maxillary arch-length discrepancy. Also, lateral expansion of the maxillary arch needed to be prevented because of unfavorable long-term stability issues and a possible adverse periodontal response. In the mandible, the treatment included intrusion of the anterior teeth to flatten the deep curve of Spee. Protraction of the left mandibular quadrant with a miniscrew implant to correct the midline deviation and establish proper incisor and molar relationships was planned as well.
In the maxillary arch, the planned amounts of distalization were 4.0 mm on the right side and 3.0 mm on the left. By moving the maxillary dentition superiorly and posteriorly, the occlusal plane angle would be maintained, and the vertical dimension would not be increased. In the mandibular arch, the incisors were to be intruded 2.0 mm, and the mandibular left quadrant was to be protracted by 1.5 mm. Because of tooth-size discrepancies, additional spaces of 0.5 mm in the maxilla and 2.5 mm in the mandible would be created by interproximal stripping.
Treatment progress
Before the orthodontic treatment, the maxillary third molars were extracted to distalize the maxillary dentition, and the mandibular third molars were also extracted because of partial impaction. To maintain the sagittal position of the maxillary anterior teeth, the second molars were distalized first by using a modified pendulum appliance before leveling and alignment with bracket bonding ( Fig 4 ). For molar distalization, a miniscrew implant (Orlus, Ortholution, Seoul, Korea) was placed in the midpalate, which is known to be the most stable and useful position in the maxilla. Five months later, interproximal spaces of 2 mm on the right side and 4 mm on the left were obtained between the first and second molars. To distalize the other teeth and relieve crowding simultaneously, 0.022 × 0.028-in edgewise brackets were bonded to both arches, and 2 miniscrew implants were placed in the buccal interradicular bone. The modified pendulum appliance was removed. In the maxilla, a 0.016 × 0.022-in nickel-titanium wire was engaged, and 200 g of distal driving force was applied with an elastomeric chain, which was intended to make space for a lingually positioned lateral incisor on the right side and to correct the midline and molar relationship on the left. In the mandible, the anterior teeth were intruded and proclined labially, and, during this period, interproximal stripping was performed several times.

Eight months after bracket bonding, leveling and alignment in the maxilla were almost complete. At this time, the molar and canine relationships were Class I on the right side and Class II on the left ( Fig 5 ). The maxillary dental midline was shifted 1.5 mm to the right of the facial midline, and the mandibular midline was shifted 1.5 mm to the left. Distalization of the maxillary left quadrant was continued, and a miniscrew implant was placed between the mandibular left first and second premolars to protract the left quadrant.




