Introduction
Interruption of treatment and poor compliance are problems in orthodontics, especially when the patient does not pay for treatment. The aim of this study was to develop a measure for orthodontists, regardless of type of practice, to assess their opinions about patient compliance.
Methods
A questionnaire, based on an orthodontic patient cooperation scale, was modified in 2 pilot phases. The piloted version was tested among 249 respondents. A principal component analysis was performed that included factors with an eigenvalue greater than 1. Reliability was assessed by means of internal consistency with Cronbach’s alphas and by test-retest (n = 40) measures, using an intraclass correlation coefficient. To assess construct validity, the responses of private and public practitioners were analyzed with chi-square and t tests.
Results
The response rate was 77%. The final questionnaire showed good reliability: Cronbach’s alpha coefficient was 0.878, and the intraclass correlation coefficient after the test-retest was 0.868. The participation rate was good, there were few missing values, and the study was multifaceted; thus the questionnaire also showed good validity for face, content, and construct. The differences between private and public practitioners were statistically significant. Five factors describing the different aspects of compliance were shown.
Conclusions
Observed differences between public and private orthodontists and dentists performing orthodontics indicated clearly the need to develop a specific measure for countries with a publicly funded system of oral health care. The measure showed good reliability and validity for face, content, and construct among Finnish orthodontists and dentists performing orthodontics. The predictive validity of the measure to assess actual patient compliance remains to be tested.
A general problem in orthodontics is that patients can interrupt their treatment. There are, however, few reported ways to predict patient cooperation. Interruption of orthodontic treatment could be a different problem in countries where the public sector provides the treatment, compared with countries where patients or parents pay for treatment in private clinics. In most Nordic countries, there is a publicly funded system in which children are entitled to free comprehensive oral health care that is orientated toward prevention. If needed, this also includes orthodontic treatment provided not only by specialists but also by general practitioners. In these countries, the need for orthodontic treatment is mostly defined by a dentist, not by the patient or his or her parents.
Since orthodontic treatment requires relatively extensive oral health resources, it is important that, to prevent disturbances and disruption of treatment, patient compliance can be evaluated and, if needed, enhanced. Of the different measures of compliance, some have been developed to monitor compliance based only on the reports of orthodontists and others by both patients and orthodontists. The general finding in these studies was the role of orthodontists in maintaining compliance by encouraging the patient, giving positive feedback, and communicating with the patient. It has even been stated that the relationship between patient and orthodontist is the most important factor in compliance. Of the practitioner-orientated measures of compliance applied in orthodontics, some are related to a special appliance. Compliance in wearing headgear has been measured, for example, by using a headgear timer or a headgear calendar. In studies with a broader and more general aspect, the overall compliance of the patient has been evaluated. According to Bartsch et al, compliance is associated with many variables, such as characteristics of the patient, family background, duration of treatment, and influence of the treatment provider. Sergl et al found that compliance in orthodontics can be predicted by the amount of initial pain and discomfort experienced. There are also reports that, in orthodontic treatment, female patients are generally more compliant than male patients.
A comprehensive and validated measure for testing patient cooperation in orthodontics was developed by Slakter et al in the United States. The orthodontic patient cooperation scale is based on a list of indicators related to patient compliance. Compliance in orthodontics has been relatively widely studied. To our knowledge, however, no measure of compliance has so far been developed for a context with emphasis on publicly funded orthodontic care. The list of indicators introduced by Slakter et al was chosen as the basis for this study because it is multifaceted and carefully developed, and it had been used previously in other studies.
The aim of this study was to develop a measure for orthodontists, regardless of type of practice, to assess their opinions about patient compliance.
Material and methods
The development of the measure, which was also to be suitable for the public health context, comprised several phases ( Fig ). In the first phase, the original 12-item indicator list of Slakter et al was translated into Finnish, and some items were edited ( Fig ). The following open-ended questions were included from the original indicator: “Can you name other indicators of noncooperation? Please list them below. Be as specific as possible. Also, if you believe that poor attitude is a major indicator of noncooperation, please list below some specific patient behaviors from which an orthodontist might infer poor attitude. Other comments?” The indicator was then tested with 8 orthodontists ( Fig ), who were asked to rank these 12 items in terms of their importance as indicators of cooperation and response to open-ended questions as in the original indicator study.
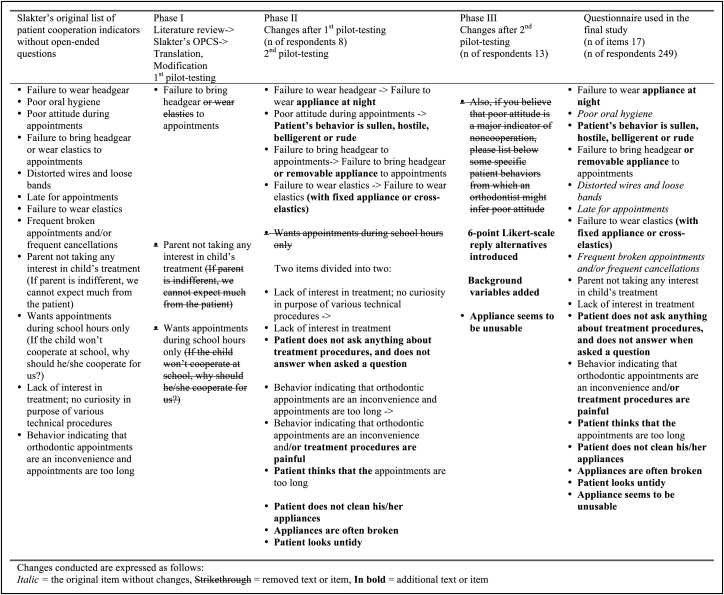
In the second phase, the items were modified based on the qualitative comments provided. Existing items were rephrased and edited. New items were added based on the comments of the respondents ( Fig ). In this phase, the modified indicator with 16 items and the open-ended questions of Slakter et al were tested among orthodontists and orthodontic residents (n = 5) as well as by public health care dentists (n = 8). The participants were again asked to rank these 16 items in terms of their importance as indicators of cooperation and to provide comments. In the third phase, and after the second pilot test, the indicator was further modified ( Fig ). At this point, to determine how much each item described a noncompliant patient according to the respondents, 6 Likert-scale reply alternatives were introduced for every item (1, not at all; 2, slightly; 3, somewhat; 4, quite a lot; 5, very much; and 6, I have no experience of this kind of behavior). In this phase, the following background variables concerning the participants were also added to the questionnaire: sex, age in years, information on specializing in orthodontics (yes or no), and type of practice (private or public health care).
The participants in the final study were members of the Orthodontic Section of the Finnish Dental Society Apollonia. The questionnaires were sent to all members (n = 249). Three sets of reminders were sent; finally, 192 (77.4%) questionnaires were returned. Of these questionnaires, 13 (6.8%) were not properly filled out, and the final number of questionnaires included in the analyses was 179 (72%). The mean ages were 51.9 years (SD, 10.7; range, 29-79 years) for all participants, 54.4 years (SD, 11.3; range, 33-76 years) for men, and 51.5 years (SD, 10.6; range, 29-79 years) for women ( Table I ). In addition, the test-retest questionnaires were collected from 40 respondents by using a 3-week mailing interval.
| Men, n (%) | Women, n (%) | All combined, n (%) | |
|---|---|---|---|
| 28 (15.6) | 151 (84.4) | 179 (100.0) | |
| Specialized in orthodontics | 24 (85.7) | 106 (70.2) | 130 (72.6) |
| General practitioners or other specialists, or specializing in orthodontics at that moment | 4 (14.3) | 45 (29.8) | 49 (27.4) |
| Working at private clinics, hospitals, or universities ∗ | 12 (42.9) | 32 (21.2) | 44 (24.6) |
| Working at public health centers |
14 (50.0) | 114 (75.5) | 128 (71.5) |
Statistical analysis
Reliability was assessed by means of internal consistency with Cronbach’s alphas and by test-retest measures with intraclass correlation coefficients. In the missing-value analysis, 6 items with missing replies were observed among the 179 participants and the total of 3043 items on the scale. To assess the construct validity, the responses of private and public practitioners were compared in cross tabulations. Statistical significance was evaluated by using chi-square and t tests. To determine whether there were any underlying constructs in this questionnaire, a principal component analysis was performed that included factors with an eigenvalue over one.
Results
The distribution of the participants is presented in Table I and the distribution of the responses in Table II . The most frequently reported characteristic of a noncompliant patient was that the appliance seemed to be unusable. Additional reported characteristics of a noncompliant patient were failure to wear the appliance at night and failure to wear intermaxillary elastics. These 3 characteristics, all of which describe a noncompliant patient, were related to appliances, whereas the 4 least important items were related mainly to appointments ( Table II ). Most respondents did not consider the patient looking untidy to be a characteristic of a noncompliant patient ( Table II ).
| Item | Mean | SD | No experience (%) |
|---|---|---|---|
| Failure to wear appliance at night | 4.60 | 0.666 | 0 |
| Poor oral hygiene | 3.79 | 0.835 | 0 |
| Patient’s behavior is sullen, hostile, belligerent, or rude | 4.15 | 1.065 | 10.6 |
| Lack of interest in treatment | 4.27 | 0.770 | 0.6 |
| Patient does not clean his or her appliances | 3.40 | 0.939 | 0 |
| Failure to bring headgear or removable appliance to appointments | 3.33 | 0.961 | 0.6 |
| Appliances are often broken | 3.51 | 0.903 | 1.7 |
| Distorted wires and loose bands | 3.87 | 1.033 | 5.6 |
| Late for appointments | 2.84 | 1.009 | 0.6 |
| Failure to wear rubber elastics (with fixed appliance or cross-elastics) | 4.41 | 0.692 | 0 |
| Frequent broken appointments or cancellations | 4.35 | 0.731 | 0.6 |
| Parent takes no interest in child’s treatment | 4.22 | 0.843 | 1.7 |
| Patient asks nothing about treatment procedures and does not answer when asked something | 3.44 | 0.975 | 3.4 |
| Patient’s behavior indicates that orthodontic appointments are an inconvenience or treatment procedures are painful | 3.39 | 0.919 | 2.3 |
| Patient thinks that appointments are too long | 2.76 | 1.156 | 25.3 |
| Appliance seems to be unusable | 4.61 | 0.717 | 1.7 |
| Patient looks untidy | 2.39 | 1.064 | 0.6 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


