Introduction
This clinical study was designed to evaluate the efficacy of innovative fiber-reinforced-thermoplastic (FRP) bonded orthodontic retainers.
Methods
Anterior lingual retainers were formed by using a 2-step process from preimpregnated unidirectional long glass fibers (volume fraction, 0.25) in a thermoplastic resin matrix of either poly(ethylene terephthalate glycol) or polycarbonate. Seventy-six canine-to-canine retainers were placed in 56 patients by using the acid-etch technique over a 34-month period. They were evaluated for clinical acceptability to function as a retainer, structural integrity of the FRP, and integrity of the bonding. Variables examined included material composition, design factors, and mechanism of failure of the retainers. The results were analyzed by using the univariate Kaplan-Meier survival method and the multivariate Cox regression model.
Results
The overall median survival time was 7.6 months, with 33% surviving after 12 months. The retainer with the longest service was in use for over 24 months. The variables with the most significant effects and improved survival rates were FRP formulation (polycarbonate), retainer thickness (1.02 mm), and number of teeth overlapped (all 6 teeth). Failure was primarily due to bond failure at the enamel-adhesive or adhesive-FRP interface.
Conclusions
With improved survival times, FRP retainers could be a viable alternative to metal retainers.
The importance of retention after orthodontic treatment is well recognized. Fixed bonded retainers are preferred when long-term retention is indicated or patient compliance is questionable. Various techniques of fixed bonded retainers with different materials have been described in the literature. Most have braided and solid metallic wires bonded with Bis-GMA bonding adhesive. Fabricating retainers from aramid fibers (Kevlar, DuPont, Wilmington, Del) and glass fibers coated with bonding adhesive have also been suggested.
Composites, reinforced with long fibers, have successfully been used as structural components in a wide range of industries including aerospace, automotive, and recreational. The good engineering properties are primarily the result of their high stiffness-weight (specific modulus) and strength-weight (specific strength) ratios when compared with other structural materials. The ability to tailor-make composite materials with a specific modulus of elasticity and enhanced load-bearing capabilities offers exciting opportunities for many applications in dentistry. Furthermore, they offer improved esthetics, and ease of forming and manipulation over metal alloys. Work has been done since the late 1980s at the University of Connecticut to develop fiber-reinforced plastics (FRP) as structural components for various dental appliances by using a 2-step process. The first step involves forming an effective FRP material where, under controlled conditions, fibers are preimpregnated with the matrix resin. This results in good control of fiber wetting, fiber volume fraction, and effective coupling between the fiber and the matrix. The second step involves forming the structural unit such as a bar of the retainer. The FRP is manipulated to different shapes by heating to a temperature of approximately 24°C to 52°C above the glass transition temperature of the polymer resin ( Table I ). At this temperature range, no significant deterioration in the mechanical or structural properties occurs. This procedure allows for the optimum development of the mechanical properties of the FRP without concern relating to the formation of the dental appliance.
| Formulation | Fiber | V f | % wt | Matrix resin | Tg of resin | Clinical forming temperature range |
|---|---|---|---|---|---|---|
| A | E fiberglass ∗ | 0.25 | 40 | PETG | 74°C | 105°C-135°C |
| B | S2 fiberglass † | 0.25 | 40 | PC | 140°C | 170°C-200°C |
∗ Electric glass, 52% SiO 2 , 14% Al 2 O 3 , 20% CaO, 8% B 2 O 3 .
The mechanical properties and hydrolytic stability of FRPs based on 6 thermoplastic resins—poly(ethylene terephthalate glycol) (PETG), polycarbonate (PC), nylon 6, nylon 12 and 2 grades of polyurethane—and 3 types of fibers—E glass, S2 glass, and Kevlar—have been reported by Goldberg et al. Although the flexural modulus and strength of FRPs made of S2 glass fiber were about 20% higher than those made of E glass, this was not statistically significant. PETG and PC resins showed the highest strength, with PC FRP showing a reinforcing efficiency as high as 0.79 and the most resistance to stress relaxation. The lower glass transition temperature of 74°C for PETG resin makes secondary fabrication in the dental laboratory more convenient than that for the PC resin, with a glass transition temperature of 140°C. In another study, Jancar et al reported that an FRP of PC reinforced with bare E fibers exhibited superior resistance to moisture attack; they advocated this material for clinical applications. The findings from these extensive laboratory tests indicate that FRPs made with PC and PETG as the matrix resin and reinforced with E or S2 glass have the most potential for clinical applications. Clinical studies have also been conducted to examine the clinical performance of fiber-reinforced fixed bridges when the substructure is made of preimpregnated, unidirectional glass fiber in a PC matrix.
The purpose of this study was to clinically evaluate the efficacy of FRPs fabricated from PC and S2 glass fiber and PETG and E glass fiber for use as fixed bonded orthodontic retainers.
Material and methods
Fifty-one patients who were scheduled to have semipermanent retention were selected from the orthodontic clinic at the School of Dental Medicine, University of Connecticut Health Center. All had received treatment for various malocclusions under different providers. The patients were of all ages and both sexes. Those with poor oral hygiene were excluded. Admission into the study was on a rolling basis over a period of 3 years. The retainers were fabricated and placed by 1 clinician (A.P.A.). The characteristics of the 76 retainers placed are listed in Table II .
| FRC formulation | Arch | Retainer thickness | Teeth overlapped | Number in group |
|---|---|---|---|---|
| A | Maxillary | 0.53 mm | 6 | 1 |
| A | Maxillary | 1.02 mm | 6 | 1 |
| B | Maxillary | 0.53 mm | 6 | 6 |
| B | Maxillary | 1.02 mm | 6 | 8 |
| A | Mandibular | 0.53 mm | 6 | 1 |
| A | Mandibular | 0.53 mm | Canines | 6 |
| A | Mandibular | 0.53 mm | Missing data | 8 |
| A | Mandibular | 1.02 mm | 6 | 6 |
| B | Mandibular | 0.53 mm | 6 | 10 |
| B | Mandibular | 1.02 mm | 6 | 24 |
| B | Mandibular | 1.02 mm | Canines | 5 |
The experimental retainers were fabricated from either FRP formulation A or formulation B ( Table I ) by using a 2-step process. In the first step, a tape of continuous glass FRP with a thickness of approximately 0.53 mm was manufactured by pultrusion (Polymer Composites, Winona, Minn). The tape was cut into strips 1.52 mm wide and 7.6 cm long with the fibers oriented parallel to the long axis of the strip. When material thickness of 1.92 mm was required, the tape was doubled and compressed in a closed mold under approximately 9.8 N in a heated laboratory press (model C, Fred Carver, Wabash, Ind) at 177°C held for 5 minutes and then cooled to room temperature.
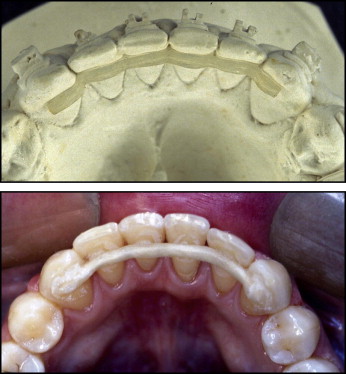
In the second step, the retainer was thermoformed by heating and adapting the FRP strip on a working model of the teeth ( Fig 1 ). The stone model was warmed in an oven set at 93°C for a minimum of 15 minutes. The strip was heated to a surface temperature of about 177°C (formulation B) and adapted to the lingual surfaces of the teeth by using a stream of hot air from a calibrated heat gun (model 6999C, Ungar, Division of Eldon Industries, Buena Park, Calif) and finger pressure. The formed retainer was trimmed to the required length and width, and the surfaces were lightly sanded with 600-grit silicon paper. Any debris was removed with an alcohol wipe.
A “retainer positioner” was fabricated to allow accurate placement of the retainer in the mouth by using a polysiloxane impression material (Permagum putty, 3M ESPE, Seefeld, Germany). The retainer surfaces were first primed with a thin coating of methylmethacrylate monomer and allowed to dry for 30 seconds before applying a thin coat of the unfilled resin. The methylmethacrylate monomer facilitates the penetration of the bonding resin into the FRP, by the process of interdiffusion. An acid technique with a chemical-cure adhesive system (Phase II, Reliance Orthodontic Products, Itasca, Ill) was used to bond the retainers. Additional adhesive was used to overlap (cover), to a thickness of 1 mm, the retainer on all 6 teeth or only the canines. Any adhesive flash was removed and smoothed with a scaler and polishing burs. The occlusion was checked with articulating paper, and any heavy contacts were reduced. All patients were instructed in proper oral hygiene.
Evaluations were made at baseline, 1 week, 1 month, and then at intervals of 3 months. At each recall, intraoral photographic slides were taken. The retainer and the alignment of the teeth were examined by using a dental mirror and an explorer after drying the area with a stream of air. The retainers were evaluated for clinical acceptability to function as retainers, structural integrity of the FRP material, integrity of the bonding and overlap sites, and surface texture of the overlap adhesive. The retainers were considered failed if any of the following were demonstrated: orthodontic relapse of any retained teeth, fracture of the FRP material, or complete or partial looseness of retainer caused by detachment from the bonded teeth or material breakage. Patients were also monitored for any carious or periodontal problems and asked for their satisfaction with the retainer.
Statistical analysis
Statistical analysis was done with SAS software (SAS, Cary, NC). The effects of the following variables on the survival rate of the retainers were evaluated: (1) FRP formulation (A vs B), (2) arch location of the retainer (maxillary vs mandibular), (3) retainer thickness (0.53 vs 1.02 mm), and (4) overlap (coverage) of the retainer with adhesive at bonding (all 6 teeth vs canines). Retainer survival (duration) was taken to be the time between the date of placement and date of failure or censoring. Retainers that were functional at the last contact were considered censored with respect to survival. Survival curves were generated by using the Kaplan-Meier product-limit method. Comparisons between 2 or more survival distributions were made with the log-rank test. Multivariate Cox proportional hazards regression models were used to compare survival times for individual variables and for several variables simultaneously. The latter gave a more appropriate assessment of the effect of a variable, because the model adjusts for differences in other variables. Significance was set at the 95% confidence level. Relative risks were calculated as exponents of corresponding coefficients in the Cox proportional hazards regression model.
Results
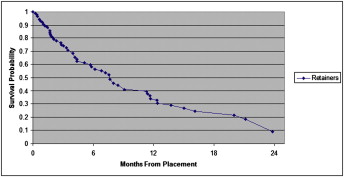
A Kaplan-Meier survival probability plot is shown in Figure 2 for all retainers. The overall median survival rate was 7.7 months, with a 1-year survival rate of 33%. Of the 76 retainers placed, 54 (71%) had failed and 22 (29%) were censored at the end of the study. The longest surviving retainers had passed the 24-month recall.
Univariate survival analyses and the number of retainers in the different groups are listed in Table III . Retainers fabricated from formulation B had significantly longer survival times than those of formulation A ( P = 0.0001). The median survival times were 11.37 and 2.97 months, respectively ( Fig 3 , A ). Retainers with a thickness of 1.02 mm survived significantly longer than those with a thickness of 0.53 mm ( P = 0.0278) ( Fig 3 , B ). The median survival times were 11.23 and 3.12 months, respectively. The mean survival time for mandibular retainers was 7.93 months compared with 7.55 months for maxillary retainers ( Fig 3 , C ), but this was not statistically significant. Retainers with all teeth overlapping had significantly longer survival times than those with only the canines were bonded and overlapped ( P = 0.0147). The median survival times were 9.03 and 3.27 months, respectively ( Fig 3 , D ).



