Armamentarium
|
History of the Procedure
The tongue flap is a specialized, pedicled flap for reconstruction of the oral cavity that frequently is used to correct congenital or acquired defects. The tongue has a robust vasculature supply, making the flap durable and readily used as a primary method of reconstruction or as a salvage procedure when other reconstruction efforts have failed. Inherent flap effects on oral function limit the tongue flap’s clinical application and tolerance by patients; however, the technique has been documented since the early 1900s. In 1901, Eiselsberg described a pedicled tongue flap for reconstruction of intraoral defects, and Lexer reported the use of a tongue flap for retromolar and tonsillar defects in 1909. In 1956, Klopp and Schurter reintroduced the technique in the reconstruction of soft palate defects, and in 1966, Guerrero-Santos and Altamirano discussed use of the technique for closure of hard palatal fistulas. In 1972, Jackson suggested the use of tongue flaps for closure of palatal fistulas in children. Subsequent articles have reviewed the use of tongue flaps for correction of floor of the mouth defects, lip defects, cleft-related fistulas, and tongue defects. Specifically, Lam et al. described a sliding anterior hemitongue flap for hemitongue glossectomy defects after squamous cell carcinoma resection, and Buchbinder and St-Hilaire described a sliding posterior tongue flap for lateral defects up to 6 cm.
History of the Procedure
The tongue flap is a specialized, pedicled flap for reconstruction of the oral cavity that frequently is used to correct congenital or acquired defects. The tongue has a robust vasculature supply, making the flap durable and readily used as a primary method of reconstruction or as a salvage procedure when other reconstruction efforts have failed. Inherent flap effects on oral function limit the tongue flap’s clinical application and tolerance by patients; however, the technique has been documented since the early 1900s. In 1901, Eiselsberg described a pedicled tongue flap for reconstruction of intraoral defects, and Lexer reported the use of a tongue flap for retromolar and tonsillar defects in 1909. In 1956, Klopp and Schurter reintroduced the technique in the reconstruction of soft palate defects, and in 1966, Guerrero-Santos and Altamirano discussed use of the technique for closure of hard palatal fistulas. In 1972, Jackson suggested the use of tongue flaps for closure of palatal fistulas in children. Subsequent articles have reviewed the use of tongue flaps for correction of floor of the mouth defects, lip defects, cleft-related fistulas, and tongue defects. Specifically, Lam et al. described a sliding anterior hemitongue flap for hemitongue glossectomy defects after squamous cell carcinoma resection, and Buchbinder and St-Hilaire described a sliding posterior tongue flap for lateral defects up to 6 cm.
Indications for the Use of the Procedure
The tongue flap is indicated in the treatment of congenital and acquired defects of the oral cavity, such as residual fistulas in cleft palate patients; for reconstruction after tumor resection; and for traumatic injury repair. General categories for which use of a pedicled tongue flap can be considered include :
- •
Oronasal communications
- •
Oroantral communications
- •
Floor of the mouth or buccal mucosal defects
- •
Lip defects
- •
Tongue defects
Limitations and Contraindications
Patient tolerance is likely to be the main limitation on the use of a tongue flap in reconstructive surgery. No absolute contraindications exist, but relative contraindications include (1) creation of a previous tongue flap; (2) tobacco use, due to its effects on wound healing; and (3) significant medical comorbidities, such as anxiety disorders, diabetes, seizures, and severe malnutrition, which may be affected by tongue flap surgery and associated maxillomandibular fixation, if used.
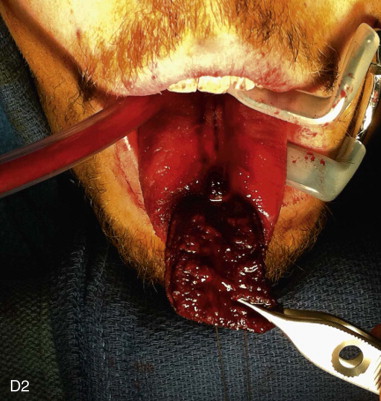
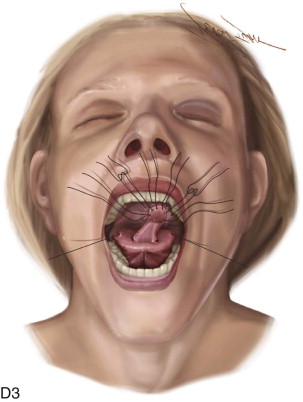
Technique: Tongue Flap
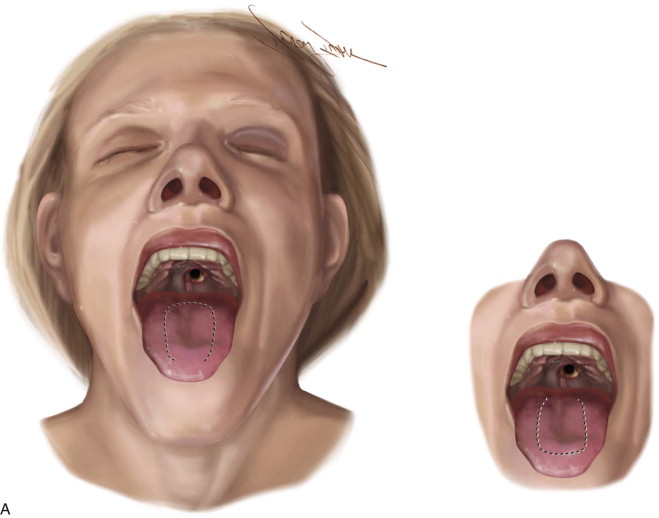
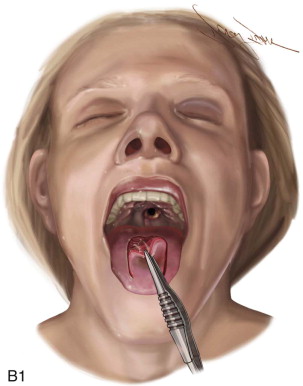
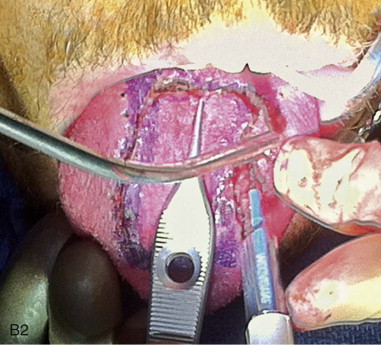
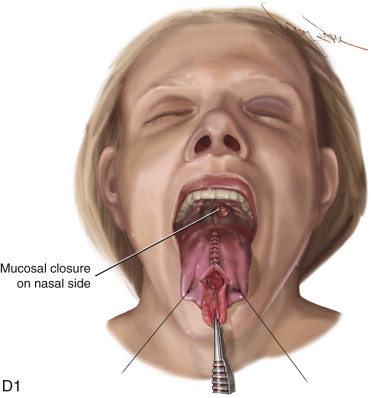
The surgical design of a tongue flap is dictated by the defect. The two main types of flaps are anterior-based flaps and posterior-based flaps. Posterior-based flaps typically are used for defects of the soft palate, retromolar area, and posterior buccal mucosa. Anterior-based flaps are more ideal for defects of the hard palate, upper and lower lips, and anterior buccal mucosa. The central or paramedial tongue flap, either anterior or posterior dorsal, is a random pattern flap with robust vascularity from branches of the lingual artery. The lateral tongue flap, however, may be an axial pattern flap if the dorsal lingual artery is included ( Figure 108-1, A ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


