Armamentarium
|
History of the Procedure
The anterolateral thigh (ALT) flap is a soft tissue perforator free flap normally pedicled on the descending branch of the lateral circumflex femoral artery (LCFA). It was first described by Song et al. as a septocutaneous flap in 1984. It did not initially gain widespread popularity because it was found that in most cases, the anterolateral thigh skin was supplied only by musculocutaneous perforators, and septocutaneous vessels were seldom present. However, as surgeons gained experience with perforator flaps and the skills for intramuscular perforator dissection improved, use of the flap became increasingly popular. Wei et al., in particular, have enthusiastically endorsed its versatility and reliability for head and neck reconstruction, pioneering the concept of the “freestyle flap.”
The flap may be raised as a fasciocutaneous or myocutaneous flap. It also can be raised with multiple skin paddles or as a chimeric flap with separate skin and muscle components. In this way, the flap can be custom-designed to fit almost any soft tissue defect in the head and neck. The perforators are reliably positioned, and the pedicle is long and wide. Two-team surgery is easily performed without the need for patient repositioning. Long-term donor site morbidity is low, and in all but the largest diameter skin harvest, the donor site may be closed primarily. In their study, Brown et al. reported that patients preferred the thigh donor site, which may be easily concealed, over the more visually apparent forearm donor site.
History of the Procedure
The anterolateral thigh (ALT) flap is a soft tissue perforator free flap normally pedicled on the descending branch of the lateral circumflex femoral artery (LCFA). It was first described by Song et al. as a septocutaneous flap in 1984. It did not initially gain widespread popularity because it was found that in most cases, the anterolateral thigh skin was supplied only by musculocutaneous perforators, and septocutaneous vessels were seldom present. However, as surgeons gained experience with perforator flaps and the skills for intramuscular perforator dissection improved, use of the flap became increasingly popular. Wei et al., in particular, have enthusiastically endorsed its versatility and reliability for head and neck reconstruction, pioneering the concept of the “freestyle flap.”
The flap may be raised as a fasciocutaneous or myocutaneous flap. It also can be raised with multiple skin paddles or as a chimeric flap with separate skin and muscle components. In this way, the flap can be custom-designed to fit almost any soft tissue defect in the head and neck. The perforators are reliably positioned, and the pedicle is long and wide. Two-team surgery is easily performed without the need for patient repositioning. Long-term donor site morbidity is low, and in all but the largest diameter skin harvest, the donor site may be closed primarily. In their study, Brown et al. reported that patients preferred the thigh donor site, which may be easily concealed, over the more visually apparent forearm donor site.
Indications for the Use of the Procedure
Intraoral Defects
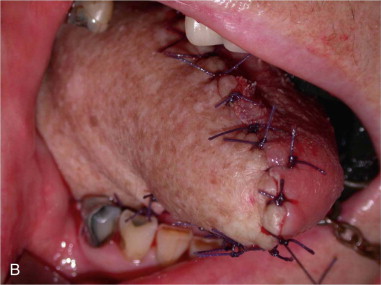
The ALT has replaced the radial forearm as the flap of choice for intraoral reconstruction in many centers, particularly in Asia. Caucasian patients have a greater amount of subcutaneous fat in the thigh, resulting in a thicker flap suitable for hemiglossectomy ( Figure 119-1 ) and larger oral cavity defects. However, it is probably too bulky for reconstruction of smaller oral cavity defects, especially defects affecting the ventral tongue, anterior floor of the mouth, and buccal mucosa, where the thinner, more pliable tissue of the radial forearm flap is often more appropriate.


Facial, Scalp, and Skull Base Defects
A large skin area may be harvested to reconstruct extensive defects resulting from cancer ablation or trauma. The skin is more pliable and may achieve a better contour compared with alternative donor sites, such as the latissimus dorsi and rectus abdominis. Flap thickness may be an advantage in reconstruction of defects of the skull base and those resulting from radical composite parotid resection ( Figure 119-2 ). The flap bulk may be further augmented in these cases, if desired, by harvesting a segment of vastus lateralis muscle with the flap.


Pharyngolaryngectomy Defects
The tubed ALT has gained in popularity over the jejunum for pharyngolaryngectomy reconstruction in recent years. The skin provides increased rigidity compared with the jejunum, and the ability to harvest a fascial flange surrounding the cutaneous aspect of the flap allows for two-layered, watertight closure. Some evidence suggests that the ALT is superior to jejunal flaps with regard to tracheoesophageal speech and swallowing and avoids the risks associated with a laparotomy. However, the enthusiasm to abandon the jejunal flap in favor of the ALT is not universal, and these authors have reported an increased stricture rate for ALT reconstruction of circumferential defects.
Surgical Anatomy
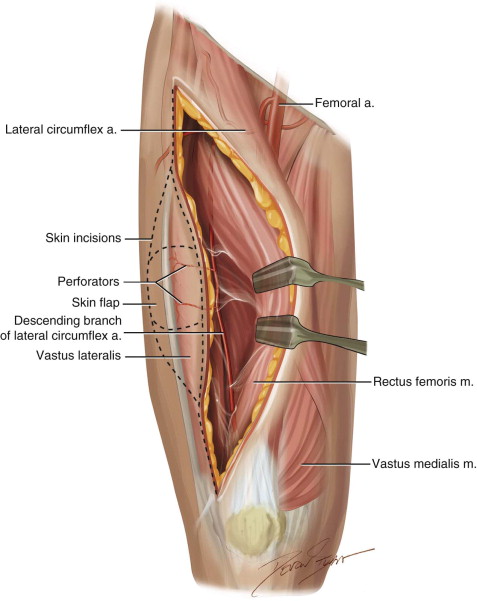
The ALT flap is pedicled on the descending branch of the LCFA, which is the largest branch of the profunda femoris system ( Figure 119-3 ). The pedicle is made up of one artery and usually two veins and runs in the intermuscular septum between the rectus femoris and vastus lateralis muscles, along with the motor nerve supply to the vastus lateralis. The pedicle length ranges from 8 to 16 cm. If harvested at its takeoff from the profunda femoral vessels, it has a vessel diameter of at least 2 mm, and typically 4 mm for the artery and 6 mm for the veins. The pedicle gives off perforating branches to the rectus femoris and vastus lateralis and septocutaneous branches to the skin of the anterolateral thigh (although, as already mentioned, these are not reliably present). Some of the vastus perforators terminate by piercing the deep fascia to supply the skin of the anterolateral thigh. These perforating branches are dissected to harvest the flap.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


