Introduction
The aim of this study was to analyze the very long-term effects of Herbst treatment on tooth position and occlusion.
Subjects
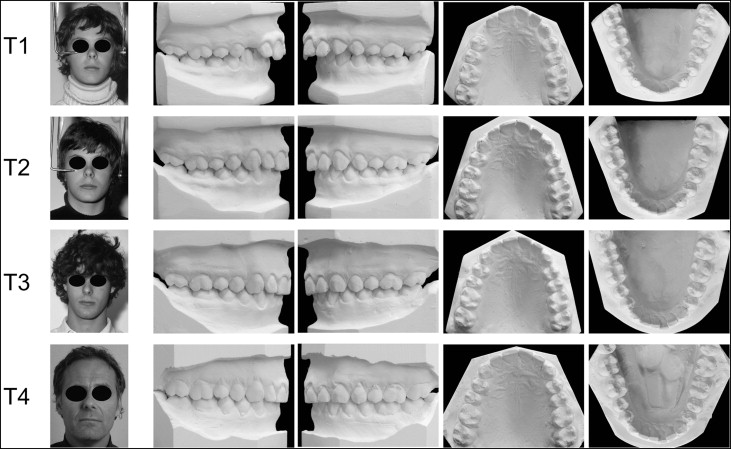
Fourteen patients from a sample of 22 with Class II Division 1 malocclusions consecutively treated with the banded Herbst appliance were reexamined 32 years after therapy.
Methods
Dental casts were analyzed from before (T1) and after (T2) treatment, and at 6 years (T3) and 32 years (T4) after treatment.
Results
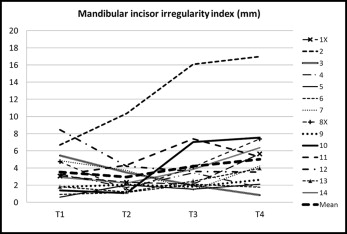
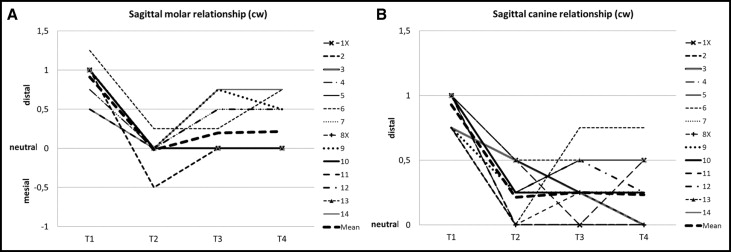
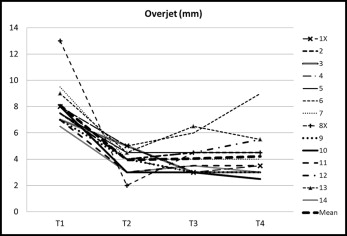
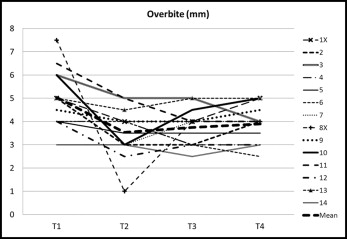
Minor changes in maxillary and mandibular dental arch perimeters and arch widths were seen during treatment (T1-T2) and posttreatment (T2-T4). Mandibular incisor irregularity remained, on average, unchanged from T1 to T2 but increased continuously during the 32-year follow-up period (T2-T4). Class II molar and canine relationships were normalized in most patients from T1 to T2. During the early posttreatment period (T2-T3), there was a minor relapse; during the late posttreatment period (T3-T4), molar and canine relationships remained, on average, unchanged. Overjet and overbite were reduced to normal values in all subjects during treatment (T1-T2). After treatment (T2-T4), overjet remained, on average, unchanged, but overbite increased insignificantly.
Conclusions
Thirty-two years after Herbst therapy, overall, acceptable long-term results were seen. Stability was found in 64% of the patients for sagittal molar relationships, in 14% for sagittal canine relationships, in 86% for overjet, and in 86% for overbite. A Class II relapse seemed to be caused by an unstable interdigitation of the occluding teeth, a persisting oral habit, or an insufficient retention regimen after treatment. Most posttreatment changes occurred during the first 6 years after treatment. After the age of 20 years, only minor changes were noted. Long-term posttreatment changes in maxillary and mandibular dental arch perimeters and widths as well as in mandibular incisor irregularity seemed to be independent of treatment and a result of physiologic dentoskeletal changes throughout adulthood.
The great potential of the Herbst appliance in the clinical management of Class II malocclusions has been documented in several investigations and summarized in the textbook of Pancherz and Ruf. Corrections of the Class II dental arch relationship and overjet are mainly accomplished by anterior advancement of the mandible (stimulation of condylar growth), distal movement of the maxillary lateral teeth, and proclination of the mandibular incisors. Overbite reduction results from extrusion of the mandibular molars and intrusion of the mandibular incisors. The Herbst appliance cannot relieve mandibular crowding. Thus, in crowded Class II malocclusion cases, extractions of teeth (mostly the 4 premolars) must often be performed; after that, the Class II problem has been solved with the Herbst appliance. In previous articles on changes after Herbst therapy, the follow-up periods varied between 1 and 10 years, and they usually end in late adolescence or early adulthood, when growth-related dentoskeletal changes still can occur.
To date, there has been no long-term follow-up study after Herbst therapy in adolescent patients in which the follow-up period ends in the patients’ middle life, when growth-related changes in tooth position and occlusion must be considered to be at a minimum or at an end.
Therefore, the aim of this very long-term follow-up investigation after Herbst treatment was to reexamine previous adolescent patients (age, 12-14 years) at least 30 years after treatment. The study was planned to comprise 3 parts: (1) a biometric analysis of dental casts, (2) a cephalometric radiographic analysis of lateral head films, and (3) a functional analysis of the masticatory system with special reference to the temporomandibular joint.
Material and methods
The patients in this study were derived from a well-defined sample of 22 consecutive patients with Class II Division 1 malocclusion treated with the Herbst appliance at the University of Malmö in Lund, Sweden, in 1977 and 1978. These subjects were presented in 2 articles in 1982. However, in these articles, only cephalometric changes from before treatment to the end of active treatment were considered. Superimposed head-film tracings from every patient were shown.
In 2011 and 2012, 30 to 33 years after Herbst therapy, these 22 subjects were recalled to the orthodontic department in Malmö for a follow-up investigation. At this time, they were 42 to 48 years of age. Two persons were deceased, and 6 did not come, for several reasons. Thus, the final follow-up sample comprised 14 subjects (12 men, 2 women) and is presented in detail in Table I . Before Herbst treatment, 12 subjects had a bilateral distal molar relationship greater than 0.75 cusp width, and 2 had a 0.5 cusp-width distal molar relationship. All 14 subjects had a bilateral distal canine relationship greater than 0.75 cusp width. Overjets ranged from 6.5 to 13 mm, and overbites from 3 to 7.5 mm.
| Patient | Sex | Treatment | Age (y) | Follow-up periods (y) | Retention | Treatment result | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T2-T3 | T3-T4 | T2-T4 | Fixed (F) or removable (R) | Stable (S) or relapsed (R) | |||
| 1X | Male | Herbst/extraction | 13 | 17 ∗ | 21 | 48 | 4 | 27 | 31 | F/R (2 y) | S |
| 2 | Male | Herbst | 13 | 14.5 | 20.5 | 48 | 6 | 27.5 | 33.5 | No retention | S |
| 3 | Male | Herbst | 11 | 12.5 | 19 | 45 | 6.5 | 26 | 32.5 | No retention | S |
| 4 | Male | Herbst | 13 | 14.5 | 20.5 | 47.5 | 6 | 27 | 33 | R (4 y) | S |
| 5 | Male | Herbst | 13.5 | 15 | 19 | 46.5 | 4 | 27.5 | 31.5 | R (3 y) | R (partial) |
| 6 | Male | Herbst | 13 | 14.5 | 20.5 | 47.5 | 6 | 27 | 33 | No retention | R (total) |
| 7 | Female | Herbst | 13 | 14.5 | 20.5 | 48 | 6 | 27.5 | 33.5 | R (2 y) | S |
| 8X | Male | Herbst/extraction | 13 | 15 | 22 | 48 | 7 | 26 | 33 | F/R (4 years) | S |
| 9 | Male | Herbst | 12.5 | 14 | 20 | 45 | 6 | 25 | 31 | R (2 y) | S |
| 10 | Male | Herbst | 12 | 14 | 20 | 44 | 6 | 24 | 30 | No retention | S |
| 11 | Female | Herbst | 11 | 12.5 | 18.5 | 42.5 | 6 | 24 | 30 | R (2 y) | S |
| 12 | Male | Herbst | 12.5 | 14 | 21 | 46 | 7 | 25 | 32 | F/R (3 y) | R (1 side) |
| 13 | Male | Herbst | 12.5 | 14 | 21 | 45 | 7 | 24 | 31 | R (2 y) | R (partial) |
| 14 | Male | Herbst | 12.5 | 14 | 22 | 45 | 8 | 23 | 31 | R (2 y) | R (1 side) |
| Summary/Mean | 12 men 2 women | 12 Herbst 2 Herbst/extraction | 12.5 | 14.3 | 20.4 | 46.1 | 6.1 | 25.7 | 31.8 | 4 no retention 10 retention | 9 stable 5 relapsed |
∗ Includes a 2-year break in treatment during the period T1-T2.
Treatment of all subjects was performed by an author (H.P.) using a banded-type Herbst appliance with a simple anchorage system. Because of major tooth irregularities after Herbst therapy in 2 patients (patients 1X and 8X), extractions of 4 premolars were performed, and maxillary and mandibular multibracket appliances were placed for about a year. Furthermore, for tooth alignment in a nonextraction patient (patient 12), a maxillary multibracket appliance treatment phase was instituted for 6 months after the Herbst phase. In these 3 patients, multibracket treatment after the Herbst phase did not aim to affect the occlusion but only to align the teeth, after the Class II dental arch and overjet corrections were achieved by the Herbst appliance.
Dental casts in centric occlusion secured by a wax bite were analyzed at 4 occasions: T1, before Herbst treatment; T2, after treatment, about 12 months after the Herbst appliance was removed and the occlusion had settled (for the 2 extraction patients [1X and 8X], T2 implied that the dental casts were analyzed after removal of the multibracket appliance); T3, 6 years after treatment at an average age of 20 years when the radius epiphysis/diaphysis plate was closed (hand-wrist stage R-J, according to Hägg and Taranger ); and T4, 32 years after treatment at an average age of 46 years.
The changes in tooth position and occlusion were analyzed during the following observation periods: T1-T2, treatment changes; T2-T3, early posttreatment changes; T3-T4, late posttreatment changes; and T2-T4, total posttreatment changes.
The dental casts from T1, T2, T3, and T4 were digitally photographed using a standard setup. The pictures were then evaluated with measurement analysis software (FACAD; Illexis AB, Linköping, Sweden). A millimeter ruler was included in the photographic setup and used for calibrating the photographic illustrations of the casts.
The biometric analysis comprised the following variables.
- 1.
Arch perimeter: the maxillary and mandibular arch perimeters were measured sectionally with (a) the distance from the distal contact point of the second premolar (or deciduous second molar) to the mesial contact point of the first premolar (or deciduous first molar); (b) the distance from the mesial contact point of the first premolar (or deciduous first molar) to the distal contact point of the lateral incisor; and (c) the distance from the distal contact point of the lateral incisor to the midline point between the 2 central incisors. Arch perimeter was calculated as the sum of these 3 measurements.
- 2.
Maxillary and mandibular arch widths: intermolar arch width is the distance between the mesiobuccal cusp tips of the first molars, and intercanine arch width is the distance between the cusp tips or estimated cusp tips in case of wear facets.
- 3.
Mandibular incisor irregularity index: the linear displacement of the anatomic contact points of the mandibular incisors mesially to the canines according to the method of Little.
- 4.
Sagittal dental arch relationships: molar and canine relationships of the left and right sides were recorded with the precision of half a cusp. Normal, mesial, or distal relationships were assessed. The results from the left and right sides were pooled and averaged.
- 5.
Overjet: the distance from the incisal edge of the most labial maxillary incisor to the opposing mandibular central incisor was recorded with a steel ruler with a precision of 0.5 mm.
- 6.
Overbite: the vertical overlap of the maxillary and mandibular incisors was measured with a steel ruler with a precision of 0.5 mm.
Maxillary and mandibular arch perimeters, intermolar and intercanine widths, and the mandibular incisor irregularity index were measured by an observer (B.L.S.) using the FACAD analysis software. Sagittal molar and canine relationships as well as overjet and overbite were measured directly on the dental casts by another observer (K.H.).
Statistical analysis
The data generated from the FACAD program and the direct cast measurements were imported to the SPSS software package (version 20.0; IBM, Armonk, NY) for statistical analysis.
The arithmetic means and standard deviations were calculated. Paired t tests were performed to assess the statistical significance of changes during the different observation periods. The levels of significance used were P <0.001, P <0.01, and P <0.05. P ≥0.05 was considered not significant.
The error of the method, determined according to Dahlberg’s formula, was negligible for the assessment of sagittal molar and canine relationships. For the other variables, the errors ranged from 0.2 to 0.8 mm. The precision of the registrations was tested by double measurements of 10 randomly selected photos and dental casts.
The study was approved by the ethical committee at the University of Lund in Sweden (number 2012/44).
Results
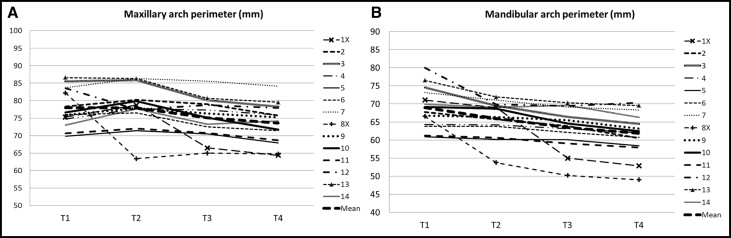
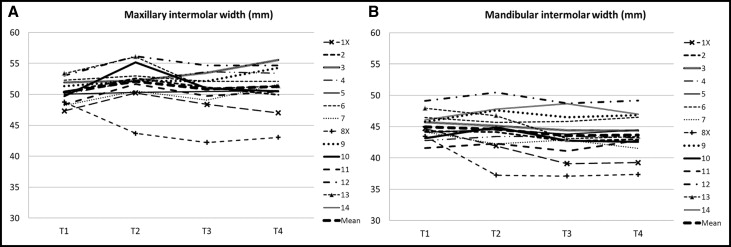
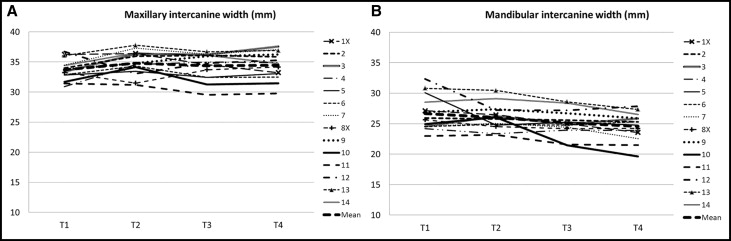
For each variable, the changes are shown graphically in Figures 1 through 7 . The arithmetic means and standard deviations at each time of examination as well as the statistical evaluations of changes during the different examination periods are given in Table II . Because treatment (T1-T2) changes for the variables of arch perimeter and arch width have been reported extensively in earlier Herbst studies, for these parameters in the discussion below, emphasis will be placed on the posttreatment (T2-T4) changes. However, for the mandibular incisor irregularity and occlusion variables, attention will be placed on both the treatment and posttreatment changes.
| Variable (mm or cusp width) | T1 | T2 | T3 | T4 | T1-T2 | T2-T3 | T3-T4 | T2-T4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | t | P | t | P | t | P | t | P | |
| Maxillary arch perimeter | 78.0 | 5.45 | 78.0 | 6.23 | 75.1 | 5.73 | 73.6 | 5.75 | 0.04 | NS | 2.95 | <0.05 | 5.07 | <0.001 | 4.15 | <0.01 |
| Mandibular arch perimeter | 69.0 | 5.67 | 66.0 | 5.20 | 63.5 | 5.85 | 63.4 | 5.18 | 0.01 | <0.05 | 2.67 | <0.05 | 0.06 | NS | 1.47 | NS |
| Maxillary intermolar width | 50.3 | 1.85 | 52.1 | 3.09 | 50.8 | 3.06 | 51.3 | 3.26 | −2.72 | <0.05 | 2.61 | <0.05 | −1.33 | NS | 1.30 | NS |
| Mandibular intermolar width | 44.9 | 2.05 | 44.6 | 3.20 | 43.6 | 3.24 | 44.4 | 2.74 | 0.63 | NS | 2.87 | <0.05 | −1.01 | NS | 0.15 | NS |
| Maxillary intercanine width | 33.7 | 1.79 | 34.8 | 2.03 | 34.4 | 2.19 | 34.5 | 2.27 | −2.07 | NS | 1.13 | NS | −0.58 | NS | 0.69 | NS |
| Mandibular intercanine width | 26.6 | 2.80 | 26.0 | 2.03 | 25.1 | 2.12 | 24.6 | 2.26 | 1.12 | NS | 2.56 | <0.05 | 2.14 | NS | 2.78 | <0.05 |
| Irregularity index | 3.5 | 2.28 | 3.0 | 2.40 | 4.2 | 3.89 | 5.0 | 4.06 | 1.06 | NS | −1.91 | NS | −1.66 | NS | −2.66 | <0.05 |
| Sagittal molar relationship ∗ | +0.9 | 0.21 | 0.0 | 0.15 | +0.2 | 0.30 | +0.2 | 0.30 | 13.98 | <0.001 | −2.60 | <0.05 | 0.43 | NS | −3.05 | <0.01 |
| Sagittal canine relationship ∗ | +0.9 | 0.15 | +0.2 | 0.22 | +0.3 | 0.24 | +0.2 | 0.24 | 11.11 | <0.001 | −0.45 | NS | 0.37 | NS | 0.25 | NS |
| Overjet | 8.1 | 1.62 | 3.9 | 0.89 | 4.0 | 1.13 | 4.2 | 1.67 | 7.23 | <0.001 | −0.31 | NS | −0.72 | NS | −0.67 | NS |
| Overbite | 5.0 | 1.23 | 3.5 | 1.06 | 3.8 | 0.78 | 3.8 | 0.83 | 3.20 | <0.01 | −0.74 | NS | −1.00 | NS | −0.36 | NS |
∗ + indicates distal (Class II) molar and canine relationships (in cusp width); 0 indicates neutral (Class I) molar relationship.
For the arch perimeter changes in the posttreatment period (T2-T4), we found the following. For the maxillary arch perimeter in the 14 subjects, except for an extraction patient (8X), the arch perimeter decreased continuously during both the early follow-up period of 6 years (T2-T3) (mean, 2.9 mm; P <0.05) and the late follow-up period of 26 years (T3-T4) (mean, 1.5 mm; P <0.001) ( Table II ; Fig 1 , A ). For the mandibular arch perimeter in the 14 subjects, the arch perimeter decreased during the early follow-up period of 6 years (mean, 2.5 mm; P <0.05) and remained unchanged during the late follow-up period of 26 years (T3-T4) ( Table II ; Fig 1 , B ).
For the arch width changes in the posttreatment period (T2-T4), we found the following. For the maxillary intermolar arch width in the 14 subjects, arch width decreased during the early follow-up period of 6 years (T2-T3) (mean, 1.3 mm; P <0.05) and increased insignificantly (mean, 0.5 mm) during the late follow-up period of 26 years (T3-T4) ( Table II ). In the 2 extraction subjects (1X and 8X), there were, for natural reasons, larger decreases in maxillary intermolar arch width than in the 12 nonextraction subjects ( Fig 2 , A ).
For the mandibular intermolar arch width in the 14 subjects, arch width decreased during the early follow-up period of 6 years (mean, 1.0 mm; P <0.05) and increased insignificantly (mean, 0.8 mm) during the late follow-up period of 26 years (T3-T4) ( Table II ). In 1 extraction subject (1X), there was a decrease in arch width during the first follow-up period (T2-T3), whereas it remained unchanged during the second follow-up period (T3-T4). In the other extraction subject (8X), no change in intermolar arch width was seen in either follow-up period ( Fig 2 , B ).
For maxillary intercanine arch width in the 14 subjects, there were insignificant changes, during both the early follow-up period of 6 years (T2-T3) and the late follow-up period of 26 years (T2-T4) ( Table II ). No difference existed between the 2 extraction and the 12 nonextraction subjects ( Fig 3 , A ).
The mandibular intercanine arch width in the 14 subjects decreased during the early follow-up period (T2-T3) of 6 years (mean, 0.9 mm; P <0.05) and the late follow-up period (T3-T4) of 26 years (mean, 0.5 mm) ( Table II ). No differences existed between the 2 extraction and the 12 nonextraction patients ( Fig 3 , B ).
We measured the mandibular incisor irregularity index for the treatment (T1-T2) and posttreatment (T2-T4) changes. For the 14 subjects, the irregularity index decreased insignificantly during the treatment and settling period of 19 months (mean, 0.5 mm) and increased continuously during the 2 follow-up periods T2-T3 (mean, 1.2 mm, not significant) and T3-T4 (mean, 0.8 mm; not significant). During the total follow-up period of 32 years (T2-T4), however, there was a significant increase (mean, 2.0 mm; P <0.05) in the mandibular incisor irregularity index ( Table II ). In 1 nonextraction subject (patient 2), incisor tooth irregularity increased more than in any other subject ( Fig 4 ). There were no real differences between the 2 extraction subjects and the remaining 11 nonextraction subjects ( Fig 4 ).
We measured the sagittal molar relationship for the treatment (T1-T2) and posttreatment (T2-T4) changes in the 14 subjects. The Class II sagittal molar relationship changed to a Class I relationship in all but 1 subject during the treatment and settling period of 19 months (T1-T2) (mean, 0.9 cusp width; P <0.001) ( Table II ). The molar relationship rebounded minimally in the direction of a Class II relationship during the early follow-up period (T2-T3) of 6 years (mean, 0.2 cusp width; P <0.05) and remained unchanged during the late follow-up period (T3-T4) of 26 years ( Table II ). During the total follow-up period (T2-T4) of 32 years, the molar relationship remained Class I in 9 subjects (64%) and rebounded partially (0.5 cusp width) in the direction of a Class II relationship in 5 subjects ( Fig 5 , A ). From T1 to T4, there was an average improvement in the Class II molar relationship toward a Class I relationship of 0.7 cusp width ( Table II ).
We measured the sagittal canine relationship for the treatment (T1-T2) and posttreatment (T2-T4) changes in the 14 subjects. The sagittal Class II canine relationship changed to a Class I relationship in 6 subjects and improved by 0.5 cusp width in 8 subjects during the treatment and settling period of 19 months (T1-T2) (mean, 0.7 cusp width; P <0.001). The canine relationship rebounded insignificantly in the direction of a Class II relationship (mean, 0.1 cusp width) during the early follow-up period (T2-T3) of 6 years and improved again to a Class I relationship (mean, 0.1 cusp width; not significant) during the late follow-up period (T3-T4) of 26 years ( Table II ). During the total follow-up period (T2-T4) of 32 years, the canine relationship remained Class I in 2 subjects (14%) and rebounded partially (0.5 cusp width) to a Class II in 12 subjects (86%) ( Fig 5 , B ). From T1 to T4, there was an average improvement in canine relationship toward a Class I relationship of 0.7 cusp width ( Table II ).
We measured overjet for treatment (T1-T2) and posttreatment (T2-T4) changes in the 14 subjects. Overjet was reduced in all subjects during the treatment and settling period of 19 months (T1-T2). The average reduction of overjet was 4.2 mm ( P <0.001) ( Table II ). During the total follow-up period (T2-T4) of 32 years, there was an insignificant rebound (0.3 mm) in overjet ( Table II ). Overjet increased by less than 1.5 mm in 5 subjects (36%), increased by 2.5 mm in 1 subject and by 4.0 mm in another (patient 6), and was stable or further reduced in the remaining 7 subjects (50%) ( Fig 6 ). Thus, an acceptable and stable long-term result in overjet was found in 86% of the subjects.
We measured overbite for treatment (T1-T2) and posttreatment (T2-T4) changes in the 14 subjects. Overbite was reduced in 11 subjects and remained unchanged in 3 subjects during the treatment and settling period of 19 months (T1-T2). The average reduction in overbite was 1.5 mm ( P <0.01). During the total follow-up period (T2-T4) of 32 years, there occurred an insignificant rebound (0.3 mm). Overbite increased by less than 1.0 mm in 5 subjects (36%), increased by 2 mm (patient 10) and by 3.0 mm (patient 8X) in 2 subjects, and was stable or further reduced in the remaining 7 subjects (50%) ( Fig 7 ). Thus, an acceptable and stable long-term result in overbite was found in 86% of the subjects.
The dental casts of 4 representative subjects (patients 4, 8X, 10, and 13) are shown to demonstrate the very long-term effects of Herbst treatment on the dental arches and arch relationships ( Figs 8-11 ).