Chapter 34 The uvulopalatal flap
1 INTRODUCTION
This book includes a number of chapters which describe a variety of palatal surgical procedures for sleep disordered breathing, including traditional uvulopalatopharyngoplasty (UPPP) techniques, Z-palatoplasty (ZPPP), transpalatal advancement pharyngoplasty, laser-assisted uvulopalatoplasy (LAUP), pillar implantation, etc. Most of these procedures can be divided into two mutually exclusive groups based upon several different criteria: by their action on the palate, the setting in which they are performed, and how the surgeon is reimbursed. First, these various procedures usually work by one of two different ways: by either shortening the soft palate or by stiffening it. They also differ in where they are performed: those that are more invasive and which are used for more significant obstructive sleep apnea (OSA) are generally done in the operating room under general anesthesia, and those that are less invasive and which are advocated for less severe forms of sleep disordered breathing (such as primary snoring) are done in the office under local anesthesia. Furthermore, the insurance industry makes a distinction between these two groups of procedures in regards to reimbursement: those done in the OR for OSA are generally reimbursed by insurance, while those done in the office for primary snoring and mild OSA are relegated to self-pay status.
2 THE PROCEDURE
The UPF procedure was first described by Powell et al.2 in 1996 as a UPPP variation for the operating room. A similar technique was described in 1993 by Bresalier and Brandes,3 referred to as the imbrication technique of UPPP in 1999. In 2000, I described the use of this technique in the office under local anesthetic,4 which was presented in more detail in 2003 by Neruntarat.5 The procedure can also be expanded under general anesthesia to include greater effects in the laterally, by including concurrent tonsillectomy with tonsillar pillar closure4,6 or by extending incisions superolaterally from the apices of the tonsillar fossas toward the third molar region;4 Li et al.7 call this modification an extended uvulopalatal flap. The principles of the UPF have been further extended by Friedman with the Z-palatoplasty,8 which is the subject of Chapter 33. The Z-palatoplasty is essentially a UPF procedure in which the uvula and distal soft palate are split in the midline. This creates two flaps which are advanced not only anteriorly but laterally to further augment the retropalatal airway in its lateral dimensions. Because of the versatility of the procedure, therefore, the UPF is a useful tool which should be part of the armamentarium of all surgeons who treat sleep disordered breathing.
3 TECHNIQUE
3.1 AWAKE, LOCAL ANESTHESIA, OFFICE PROCEDURE
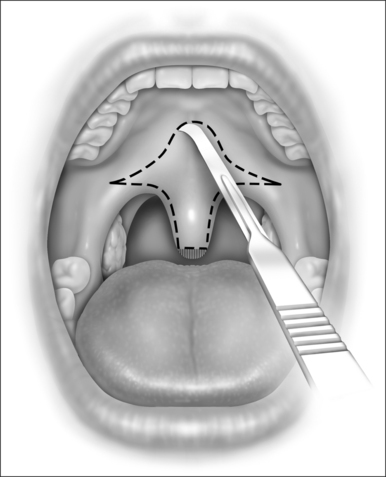
While still grasping the uvula in its new position, the planned incision is outlined with a marker or with a number 12 blade, as shown in Figure 34.1. This gothic arch-shaped incision generally has its apex within 5–10 mm of the hard–soft palate junction and flares laterally to allow for advancement of the lateral palate. The farther laterally these incisions extend, the greater the elevation of the lateral aspects of the palate. The incision will be carried caudally onto the uvula in a mirror image of the palatal incision. Unless vertical relaxing incisions are necessary, as described previously, it is recommended that the incisions be kept away from the free edge of the palate, to lessen the chance of scar contracture.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses