Fig. 9.1 OPT showing idiopathic condylar resorption.
Trismus
• Classically, an inability to open mouth due to muscular spasm, but commonly used to refer to limited mouth opening.
• Normal inter-incisal mouth opening is 35–45mm.
• Extra-articular causes:
• odontogenic infection;
• facial trauma including dento-alveolar surgery;
• myofascial pain/TMJDS;
• following ID LA block;
• depressed fractured zygoma/arch;
• radiation fibrosis;
• tetanus;
• quinsy;
• local malignancy;
• submucous fibrosis;
• coronoid hyperplasia;
• malignant hyperpyrexia.
• Intra-articular causes:
• ankylosis—bony/fibrous;
• facial trauma—effusion, fracture;
• meniscus displacement;
• osteophyte formation;
• septic arthritis.
Myofascial pain
• Synonyms: myofacial pain/facial arthromyalgia.
• Spectrum of facial pain disorders secondary to parafunctional habits, without signs and symptoms of TMJ internal derangement.
Temporomandibular joint dysfunction
• Most common non-infective pain disorder of the oro-facial region.
• Meta-analysis show that the overall prevalence of TMJDS in population studies ranges from 30–45%.
• More common in ![]() ;
; ![]() :
:![]() ratio of 1:3.
ratio of 1:3.
• Mean age is between 30 and 40 years.
• Pain is typically diffuse, cyclical and distributed in multiple sites, especially the muscles of mastication; it is frequently worse in the morning.
• Related to stress and parafunctional habits.
• Associations: depression, back pain, tension headaches, migraine, irritable bowel syndrome, fibromyalgia.
Features
• Pain.
• Clicking.
• Locking.
• Crepitus.
• Trismus.
Clinical findings
• Tenderness of the pre-auricular region and muscles of mastication.
• Clicking, usually with abnormal path of opening.
• Evidence of parafunctional activity—such as clenching causing dental attrition, linea alba affecting the buccal mucosa, scalloped tongue, masseteric hypertrophy, and biting of finger nails.
Internal derangement
• Occurs where the articular disc within the joint interferes with smooth functioning of the joint.
• Clicking usually indicates reducible displacement of the disc.
• Clicking is usually related to abnormal paths of opening, with protrusion and/or lateral deviation.
• Some patients will go on to develop locking.
• Closed lock: mouth cannot open beyond around 25mm as the head of the condyle impinges on an anteriorly displaced disc.
• Open lock: patient unable to close the mouth without manipulation, since condyle is trapped in front of posteriorly displaced disc.
• Locks may be reducible (patient can manipulate the jaw to regain mobility) or irreducible.
• Disc may perforate (associated with joint crepitus and the development of osteoarthritis).
Investigations
• Routine radiography does not change management in classical TMJDS.
• An OPT may eliminate dental pathology radiating to the ear in a non-classical pain pattern.
• Radiographic features of OA:
• narrowing of joint space;
• bone cyst (geode) formation;
• remodelling;
• osteophyte formation.
• MRI is the gold standard imaging for the TMJs. It can be useful in the assessment of patients with trismus where a closed lock (or other pathology) is suspected (Fig. 9.2).
• Approximately a third of asymptomatic patients have anterior displacement of their discs on MRI scan.
• CT scanning is superior for assessing bone detail.
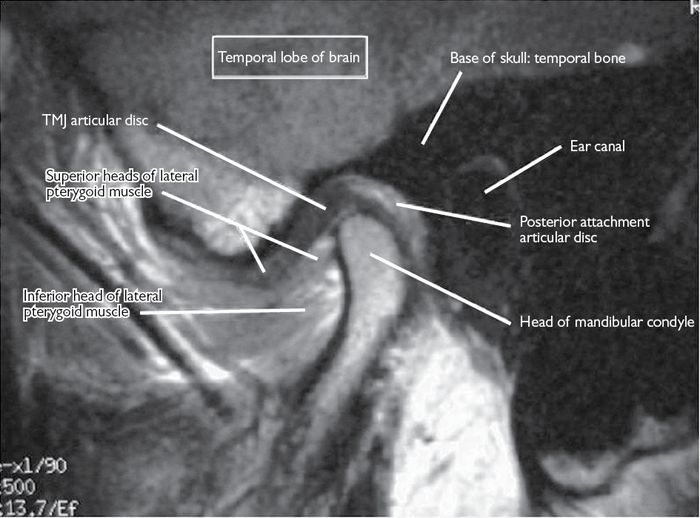
Fig. 9.2 MRI of the right temporomandibular joint.
Management/treatment
• Reassurance and explanation.
• Education regarding parafunctional habits.
• Jaw exercises, e.g. straight line to eliminate click.
• Physiotherapy.
• Analgesia.
• Heat.
• Rest/soft diet/relaxation.
• Splints/bite guards/bite raising appliances:
• variety of materials, designs, and for either jaw;
• possible mechanisms of action include reduction of bruxism and other parafunctional habits, production of a gap between the condyle and fossa to free the disc, and possible placebo effect.
Other interventions
Tricyclic antidepressants
• Have analgesic and muscle relaxant effects independent of their antidepressant action.
• No RCTs show efficacy in TMJDS.
Occlusal rehabilitation
• Most patients with abnormal occlusions do not suffer TMJ pain.
• No evidence of benefit.
• Orthodontic treatment or orthognathic surgery is not a treatment for TMJDS.
Arthrocentesis and manipulation
•
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


