Previously dentists focused on repair and maintenance of function. However, the emphasis of many patients and dentists is now on esthetics. Often there is a need for the disciplines of orthodontics, periodontics, restorative dentistry, and maxillofacial surgery to work together in order to achieve optimum results. Currently the sequencing planning process begins with esthetics and then function, structure, and ultimately biology.
Key points
- •
Previously dentists focused on repair and maintenance of function.
- •
The emphasis of many patients and dentists is now on esthetics.
- •
Often there is a need for the disciplines of orthodontics, periodontics, restorative dentistry, and maxillofacial surgery to work together in order to achieve optimum results.
- •
Currently the planning process begins with esthetics and then function, structure, and ultimately biology.
The past 20 to 30 years have seen substantial changes in the practice of dentistry. In admittedly economically advantaged populations, the daily routine has largely shifted from the unrelenting need to repair the ravages of disease to one of providing elective and to large extent cosmetic services. One could, perhaps, ascribe this change to the advent of sealants, fluorides, and the awareness of the role of bacteria in causing decay and periodontal disease. Whatever the cause, the condition of the mouth can have a strong impact on a patient’s psychological, social, and functional health. To optimize outcomes, there is often a need to integrate the disciplines of orthodontics, periodontics, restorative dentistry, and maxillofacial surgery. Improvement in esthetic satisfaction due to orthodontic or orthodontic-surgical treatment seems to lead to improvement in oral health and related quality of life. Sarver and Ackerman recommended ascertaining the positive characteristics of a patient’s smile to be sure that one shields the patient as treatment is directed at the more challenging aspects. A visualized treatment strategy must then be created to address the patient’s chief concerns. But in the end it is the restorative practitioner who is responsible for the final case outcome. Therefore an appreciation of the dental disciplines required to plan a properly sequenced treatment plan is essential. An increasing number of adult orthodontic patients who present with periodontal problems have been reported. The orthodontic problems that can often be found in patients with periodontal involvement include: proclination of the maxillary anterior teeth, irregular dental spacing, rotation, overeruption, migration, loss of teeth, or traumatic occlusion. Orthodontics in conjunction with periodontal treatment can often add considerably to the esthetic outcome. It is both intellectually interesting and a challenge to traditional values that efficacious contemporary sequential treatment planning philosophy begins with esthetics. Function, structure, and ultimately biology must then be incorporated into the planning. To treat a patient solely on the basis of esthetic outcome is an open invitation to long-term failure.
Case report
The patient is a 53-year-old female professional singer. Her chief complaint revolved around old composite restorations that “make my front teeth appear darker” and made her unhappy with her smile. She expressed a desire to straighten her bottom teeth, whiten her upper teeth, have a better curvature of her upper teeth and for her mouth to appear more attractive. A medical history was taken, and a caries risk assessment and a comprehensive extraoral examination and intraoral examination were conducted.
Dental History
Occlusal composite restorations had been done on teeth #2, #3, #4, #5, #15, #18, #19, #30, and #31; distal-occlusal (DO) composite on tooth #5; and mesial composites only on teeth #8 and #9. Gingival recession was approximately 3 mm on teeth #10 and #11. The New York University College of Dentistry (NYUCD) smile evaluation form was utilized to evaluate the patient’s chief complaint and to provide macroesthetic and microesthetic information required to make a correct diagnosis and formulate a treatment plan that would address the patient’s concerns.
Upon completion of the smile analysis, the following problems were noted:
-
The patient’s dental maxillary midline was deviated and canted to the left.
-
Her lower midline was deviated to the right.
-
There were crowded lower anteriors.
-
There was proclination of the maxillary anteriors.
-
3 mm gingival recession on #’s 10 and11 were noted.
-
A minimal amount of tooth structure was displayed at rest ( Fig. 1 ).

Fig. 1 Rest position demonstrated no visibility of maxillary incisors. -
A reverse smile was present ( Fig. 2 ).

Fig. 2 Reverse smile and overeruption of lower anteriors.
Orthodontic, periodontal, and restorative therapies were indicated in order to address all of the patient’s needs.
Diagnostic Aids
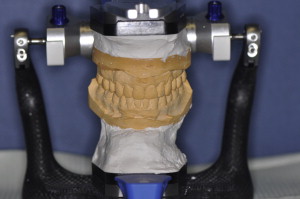
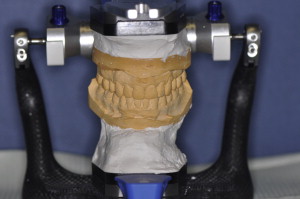
A full series of radiographs revealed recurrent caries under old composites on teeth #8, #9, and #11. Subsequently a full series of photographs was obtained in accordance with the guidelines established for the Advanced Program for International Dentists in Aesthetic Dentistry. Impressions were obtained with Reprosil (Dentsply Caulk, Milford, Delaware) for study models. A face bow record (Artex, Amann Girrbach AG, Koblach, Austria) and centric bite (Blu- Bite HP, Henry Schein, Melville, New York) were obtained to mount the study casts on a semiadjustable articulator (Artex) ( Fig. 3 ). A wax-up was fabricated based upon biomimetic principles and influenced by patient input. A putty index (Coltene Lab-Putty, Coltène/Whaledent Incorporated, Cuyahoga Falls, Ohio) was fabricated from the wax-up and an intraoral mock-up was done with a Bis-acryl material (Luxatemp Ultra, DMG America, Englewood, New Jersey) ( Fig. 4 ) so that the patent could visualize the final esthetic design. After discussion with the patient and laboratory, it was decided that feldspathic porcelain veneers from teeth #5 through #12 would achieve the patient’s desires. Because the patient desired lighter teeth, bleaching of the mandibular anterior teeth was to be completed after the veneer placement (Zoom, Philips Oral Healthcare, Stamford, Connecticut). Restorations fabricated using E Max (Ivoclar, Vivadent, Amherst, New York) were considered. After consultation with the laboratory technician, the authors jointly decided that feldspathic porcelain was the material of choice, as the preparations could be less invasive and result in veneers with superior optical qualities.

Case report
The patient is a 53-year-old female professional singer. Her chief complaint revolved around old composite restorations that “make my front teeth appear darker” and made her unhappy with her smile. She expressed a desire to straighten her bottom teeth, whiten her upper teeth, have a better curvature of her upper teeth and for her mouth to appear more attractive. A medical history was taken, and a caries risk assessment and a comprehensive extraoral examination and intraoral examination were conducted.
Dental History
Occlusal composite restorations had been done on teeth #2, #3, #4, #5, #15, #18, #19, #30, and #31; distal-occlusal (DO) composite on tooth #5; and mesial composites only on teeth #8 and #9. Gingival recession was approximately 3 mm on teeth #10 and #11. The New York University College of Dentistry (NYUCD) smile evaluation form was utilized to evaluate the patient’s chief complaint and to provide macroesthetic and microesthetic information required to make a correct diagnosis and formulate a treatment plan that would address the patient’s concerns.
Upon completion of the smile analysis, the following problems were noted:
-
The patient’s dental maxillary midline was deviated and canted to the left.
-
Her lower midline was deviated to the right.
-
There were crowded lower anteriors.
-
There was proclination of the maxillary anteriors.
-
3 mm gingival recession on #’s 10 and11 were noted.
-
A minimal amount of tooth structure was displayed at rest ( Fig. 1 ).

Fig. 1 Rest position demonstrated no visibility of maxillary incisors. -
A reverse smile was present ( Fig. 2 ).

Fig. 2 Reverse smile and overeruption of lower anteriors.
Orthodontic, periodontal, and restorative therapies were indicated in order to address all of the patient’s needs.
Diagnostic Aids
A full series of radiographs revealed recurrent caries under old composites on teeth #8, #9, and #11. Subsequently a full series of photographs was obtained in accordance with the guidelines established for the Advanced Program for International Dentists in Aesthetic Dentistry. Impressions were obtained with Reprosil (Dentsply Caulk, Milford, Delaware) for study models. A face bow record (Artex, Amann Girrbach AG, Koblach, Austria) and centric bite (Blu- Bite HP, Henry Schein, Melville, New York) were obtained to mount the study casts on a semiadjustable articulator (Artex) ( Fig. 3 ). A wax-up was fabricated based upon biomimetic principles and influenced by patient input. A putty index (Coltene Lab-Putty, Coltène/Whaledent Incorporated, Cuyahoga Falls, Ohio) was fabricated from the wax-up and an intraoral mock-up was done with a Bis-acryl material (Luxatemp Ultra, DMG America, Englewood, New Jersey) ( Fig. 4 ) so that the patent could visualize the final esthetic design. After discussion with the patient and laboratory, it was decided that feldspathic porcelain veneers from teeth #5 through #12 would achieve the patient’s desires. Because the patient desired lighter teeth, bleaching of the mandibular anterior teeth was to be completed after the veneer placement (Zoom, Philips Oral Healthcare, Stamford, Connecticut). Restorations fabricated using E Max (Ivoclar, Vivadent, Amherst, New York) were considered. After consultation with the laboratory technician, the authors jointly decided that feldspathic porcelain was the material of choice, as the preparations could be less invasive and result in veneers with superior optical qualities.

Treatment sequence
Orthodontic Considerations
The patient underwent Invisalign (Align Technology, San Jose, CA) treatment in the NYUCD Orthodontic Department. The goals were to correct the midline, procline the incisors, reduce the open bite in the right molar area, and intrude teeth #8 and #9. Invisalign uses a series of aligners created for the patient that are based upon proprietary computer program projections of the movement of the teeth over 2-week intervals. These aligner trays are worn over the teeth and gradually move them into predicted places. The authors believed that the positions of the teeth following orthodontics would permit more conservative preparation while providing the space required for veneer fabrication. The maxillary central incisors’ vertical position is critical in determining the smile arc. Ideally, the upper anterior incisal edges should be coincident with or follow the contour of the lower lip when smiling. After proper alignment of the maxillary anteriors (the new incisal edge position), the length-to-width ratio of the teeth can be considered to maximize the esthetics. The patient was an Angle Class I with 2 mm overjet and 1 to 2 mm overbite. No crowding was present in the maxillary arch, but there was a 3 mm space deficiency in the mandibular arch. Interproximal reduction (IPR) was utilized in the lower arch to create the required space.
Periodontal Considerations
Subsequent to scaling and root planning, the patient had a subepithelial connective tissue graft taken from the palate ( Fig. 5 ), with a full-thickness coronally positioned flap to correct the recession around teeth #10 and #11 ( Fig. 6 ). Preoperative intraoral antisepsis was achieved using 0,12% chlorhexidine digluconate solution (Colgate, New York, New York; Perioguard) rinsed for 1 minute. Prior to surgery, the root was lightly scaled with Gracey curettes (Hu-Friedy Manufacturing Company, Chicago, Illinois). The root surfaces were then conditioned with EDTA gel pH 6.70 (Straumann Pregel, Straumann, Basel, Switzerland) for 2 minutes to remove the smear layer, and the visible root was rinsed with copious amounts of sterile saline to remove all the EDTA remaining. This allowed the gingival margins to be symmetric prior to the restorative phase. Two oblique, divergent beveled incisions were made at the bordering teeth and were directed apically in the alveolar mucosa. A split-full thickness flap was used. A passive flap coronal mobilization needs to be achieved at the level of the cemento-enamel junction. The subepithelial connective tissue graft (SCTG) was obtained from the palatal area (see Fig. 5 ). The enamel matrix derivative (EMD) gel was then placed over the root surface, and the SCTG was placed over the gel at the level of the cemento-enamel junction. The graft was trimmed as needed to allow its extension over the bone apically and laterally 2.0 to 3.0 mm ( Fig. 7 ). The flap was then positioned coronally 2 mm past the cemento-enamel junction so as to completely cover the graft after suturing Fig. 8 . The graft enabled a more ideal crown length and gingival height compared with the contralateral side ( Fig. 9 ).



Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


