The clinical example presented in this article demonstrates a risk-based, diagnostically driven treatment planning approach by focusing on 4 key categories: periodontal, biomechanical, functional, dentofacial. In addition, our unique approach allowed the comprehensive clinical management of a patient with complex restorative needs. A full-mouth rehabilitation was completed sequentially without sacrificing the amount of dentistry necessary to restore health, comfort, function, and esthetics. The result exceeded the patient’s expectation and was made financially possible by extending treatment over numerous years.
Key points
- •
Develop a systematic approach for comprehensive treatment planning.
- •
Focus on the 4 most important diagnostic categories: periodontal, biomechanical, functional, dentofacial.
- •
Develop and utilize critical risk parameters to minimize failure and maximize successful treatment strategies.
- •
Utilize minimally invasive strategies to minimize tooth reduction and future tooth sequelae.
- •
Use a sequential management strategy for large restorative cases so finances are not a barrier to executing necessary comprehensive care.
Dental health care is evolving by improving tooth mortality through advances in technology and preventative services. Unfortunately, dentists continue to primarily base treatment on a reparative model, in which therapy merely fixes the result of disease without addressing the cause of disease. The alternative or medical model is the term coined by psychiatrist R.D. Laing for the “set of procedures in which all doctors are trained.” The concept of disease is central to the medical model. In general, disease refers to some deviation from normal body functioning that has undesirable consequences for the affected individual. An important aspect of the medical model is that it regards disease signs (objective indicators such as an increased temperature) and symptoms (subjective feelings of distress expressed by the patient) as indicative of an underlying physical abnormality (pathology) within the individual. Understanding disease expression can be confusing due to inaccurately understanding science, practitioner bias, or patient adaptation. According to the medical model, whenever possible medical treatment should be directed at the underlying pathology in an attempt to correct the abnormality and cure the disease. A comprehensive evaluation to determine the underlying cause of the disease will necessarily include chief concern, history, physical examination, ancillary tests if needed, diagnosis, treatment, and prognosis with and without treatment. “There can be several ways to treat a problem but there can only be one diagnosis”. When evaluating a fractured tooth, the reparative model would restore or fix the tooth without a definitive understanding of the underlying causes for the fracture. Did it fracture from an old restoration that structurally compromised the tooth, an unhealthy habit, tooth position, or some other reason or combination? The why must be both discovered and addressed to reduce the future risk and improve the prognosis of the diseased area or the tooth. For optimal outcomes this level of judgment may be more important than the operator’s skill level.
The fundamental rationale for a comprehensive treatment approach is a long-term strategy for dental health commensurate with an enhanced level of wellness for patients. Dental care must therefore be directed through a comprehensive system that identifies health and disease as well as the potential risks to a patient undergoing treatment or refusing it. Risk to the dentition is identified by collecting objective data in an organized system. A diagnosis is formulated first and necessary treatment can be recommended thereafter. Treatment should always mitigate future risk and improve prognoses of the teeth and therefore decrease tooth mortality.
The following clinical example demonstrates a risk-based, diagnostically driven treatment planning approach by focusing on 4 key categories: periodontal, biomechanical, functional, dentofacial. In addition, our unique approach allowed the comprehensive clinical management of a patient with complex restorative needs. A full-mouth rehabilitation was completed sequentially without sacrificing the amount of dentistry necessary to restore health, comfort, function, and esthetics. The result exceeded the patient’s expectation and was made financially possible by extending treatment over numerous years.
Patient background
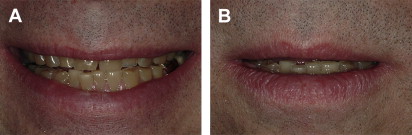
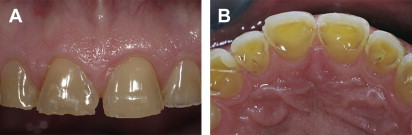
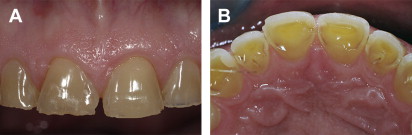
The patient was a white male engineer in his late 40s ( Fig. 1 ). His immediate chief concerns were the wear of his teeth, and the potholes on the biting surface of the posterior teeth. He stated that he could “see through the front teeth” ( Fig. 2 ). The patient stated that the wear started many years ago but had been stable until recently, when he noticed that it had worsened. He has become increasingly more self-conscious about his smile, and reported that his “bite feels unstable and uneven”. He also noted that he must consciously make an effort to find the “correct place” where his teeth fit together, and states that, “where my teeth fit together is not where my jaw feels most comfortable” ( Fig. 3 ).


He was primarily concerned with functional longevity and future protection of his remaining teeth with esthetic improvement as a secondary benefit. He had been to several dental specialists seeking care and all had recommended a full-mouth reconstruction that would need to be done all at one time. The cost of this option had prevented him from proceeding with treatment. Using the diagnostically driven treatment planning approach, the full-mouth restoration could be completed sequentially, making it financially feasible.
Patient background
The patient was a white male engineer in his late 40s ( Fig. 1 ). His immediate chief concerns were the wear of his teeth, and the potholes on the biting surface of the posterior teeth. He stated that he could “see through the front teeth” ( Fig. 2 ). The patient stated that the wear started many years ago but had been stable until recently, when he noticed that it had worsened. He has become increasingly more self-conscious about his smile, and reported that his “bite feels unstable and uneven”. He also noted that he must consciously make an effort to find the “correct place” where his teeth fit together, and states that, “where my teeth fit together is not where my jaw feels most comfortable” ( Fig. 3 ).


He was primarily concerned with functional longevity and future protection of his remaining teeth with esthetic improvement as a secondary benefit. He had been to several dental specialists seeking care and all had recommended a full-mouth reconstruction that would need to be done all at one time. The cost of this option had prevented him from proceeding with treatment. Using the diagnostically driven treatment planning approach, the full-mouth restoration could be completed sequentially, making it financially feasible.
Medical history
The only remarkable finding in the medical history was a positive response to digestive disorders. The patient was diagnosed with gastroesophageal reflux disease (GERD) in 1996 with an endoscopic procedure and, subsequently, proton pump inhibitor medication was used for 7 years. He reported no current medications except daily multivitamins.
Dental history
Overall, the patient reported favorable dental experiences. Minimal restorative care had been performed in the recent years. He had a nightguard fabricated 7 years previously in order to “protect his teeth from bruxism”, but had not worn it.
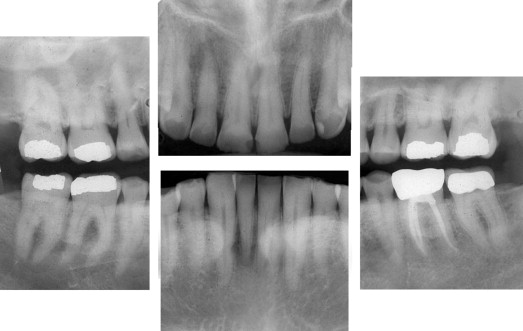
Periodontal
The patient has maintained 6-month recare intervals for many years. He had isolated 4 mm probing depths in the maxillary and mandibular molars with little to no bleeding on probing and minimal attachment loss with no areas of site-specific bone loss (vertical defects) ( Fig. 4 ). No increased genetic susceptibility was uncovered. There was no secondary occlusal traumatism. Mandibular tori and mandibular buccal exostoses were noted on teeth 19, 20, 29, and 30.
Biomechanical
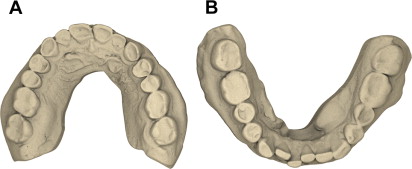
All molars were structurally compromised with large multisurface alloy restorations present on teeth 2, 3, 14, 15, 30, and 31, and full coverage cast restorations on teeth 18 and 19 with an existing root canal therapy for tooth 19. The alloy restorations were over 30 years old with visible marginal discoloration. A caries risk assessment was performed and results were negative. No cavitations or defects were determined due to caries and he reported excessive soda consumption throughout the day. However, significant biocorrosion was evident on teeth 4–13, 20–22, and 27–29 ( Fig. 5 ). The patient also reported tooth sensitivity on teeth 5, 8, and 20 and possible future pulpal pathology on teeth 2–5, 12–15, 30, and 31; significant loss of tooth structure from environmental damage was noted.
Functional
Severe attrition was noted on the anterior teeth ( Fig. 6 ), although no primary occlusal traumatism could be detected. The patient reported pain in the muscles of mastication on the right side. Both the mandibular maximal opening (46 mm) and range of motion were within normal limits. During the assessment of the temporomandibular joint, no popping, clicking, or crepitus in the joints was noted. The immobilization test was positive on the right side and negative on the left side; the load test was negative bilaterally. No additional imaging of the joints was performed.

Dentofacial
The patient was unhappy with the color of his teeth. He considered them to be “too yellow” and wanted them whiter. His face height was normal with a slightly longer inferior third. A smile evaluation determined that the dental midlines were coincident. Tooth display was −4 mm in repose and 4 mm in high smile in the right cuspid region. The lip length was within normal limits at 22 mm. He showed medium lip dynamics in the maxillary arch with 8 mm of movement and medium lip dynamics with 5 mm of movement in the mandibular arch. The gingival architecture presented with horizontal symmetry and normal gingival scallop ( Fig. 7 ). The gingival scallop form was normal and mild crowding and rotations of the mandibular anterior teeth were present.