INTRODUCTION
Temporomandibular joint (TMJ) reconstruction presents unique problems because of the integral and complex roles the TMJ plays in establishing and maintaining proper form and function within the stomatognathic system. The TMJ not only acts as a secondary growth center for the mandible in prepuberty, but also is essential to the functions of mastication, speech, airway support, and deglutition in both childhood and adulthood.
Before the early to mid-1980s, the primary reasons for TMJ reconstruction were the management of developmental maxillofacial deformities, ankylosis, severe inflammatory joint disease, or TMJ replacement after ablative tumor surgery or trauma.
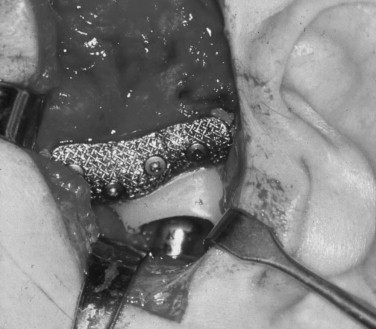
Thereafter, along with these form and function challenges, there arose a group of patients who presented requiring TMJ reconstruction having previously undergone multiple failed TMJ surgical procedures. Many of these patients’ TMJs were anatomically distorted and functionless secondary to the failure of interpositional materials such as Proplast-Teflon (Vitek, Houston, TX) and/or Silastic (Dow-Corning-Wright, Arlington, TX) ( Figure 51-1 ).

As more of these unfortunate patients presented for management, interested reconstructive surgeons began developing goals to reach physiologically reasonable, biologically rational, and technically achievable outcomes, considering not only form and function but also these patients’ neurologic and psychologic issues.
Hence, based on decades of orthopedic joint replacement experience, the following goals for any TMJ reconstruction modality were developed :
- 1.
Improvement of mandibular function and form
- 2.
Reduction of further suffering and disability
- 3.
Containment of excessive treatment and cost
- 4.
Prevention of further morbidity
TMJ pathology with anatomic form and physiologic function distortions dictates the need for reconstruction. Because of the complex nature of joint anatomic and related masticatory muscle functional relationships, it is an unreasonable expectation that a reconstructed TMJ can be returned to “normal” premorbid function. Therefore there will always be some functional disability involved with any reconstructed TMJ.
Further, in the multiply operated, anatomically distorted patients, chronic neuropathic centrally mediated pain will be a major component of their disability. Therefore it is important for both the surgeon and the patient to understand that the primary goal of any type of TMJ reconstruction is the restoration of objective mandibular form and function. Any subjective pain relief gained must only be considered as of secondary benefit.
HISTORIC PERSPECTIVE OF TMJ RECONSTRUCTION
AUTOGENOUS TMJ RECONSTRUCTION
Bone—Vascularized and Nonvascularized
Early attempts at TMJ reconstruction involved the use of autogenous tissues. In 1909 Bardenheuer performed a mandibular condyle replacement with the fourth metatarsal. This technique was also reported in 1920 by Gillies. The use of an autogenous metatarsal head to reconstruct the mandibular condyle was also reported by Dingman in 1964, Glahn in 1967, and Spiessl in 1972. Use of a nonvascularized metatarsophalangeal joint to correct a facial deformity was reported by Entin in 1958 ( Figure 51-2 ). Datillo in 1986 and Dierks in 2000 reported the use of a vascularized metatarsophalangeal joint to reconstruct the temporomandibular joint.

TMJ reconstruction has also been performed using vascularized rib and iliac crest. Other autogenous tissues—such as fibula and iliac bone free grafts, clavicle, and sternoclavicular joint—have been used. However, none of these reports provided long-term follow-up information.
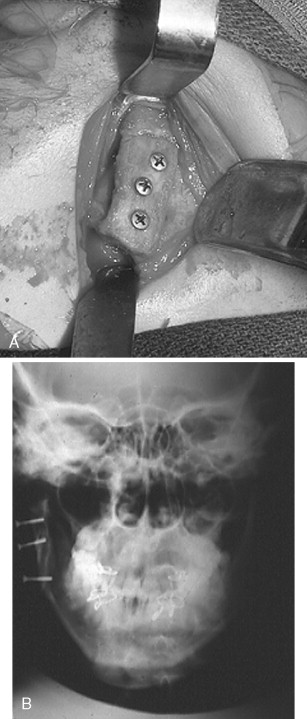
The nonvascularized costochondral free graft has been the most frequently recommended autogenous bone for the reconstruction of the TMJ because of its ease of adaptation to the recipient site, its gross anatomic similarity to the mandibular condyle, its low morbidity at the donor site, and its demonstrated growth potential in juveniles ( Figure 51-3 ).
Tissue
Vascularized and Nonvascularized Tissue.
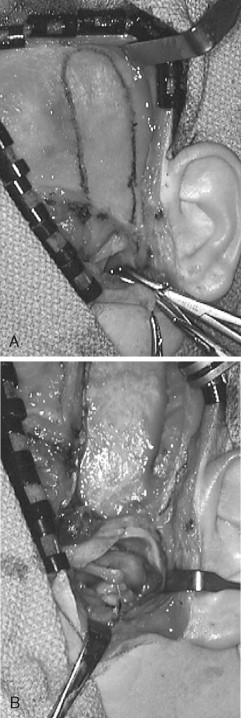
A number of different autogenous tissues—temporalis fascia, masseter, temporalis muscle flaps, dermal grafts, and fascia lata —have been advocated as a replacement for the TMJ articular disk. However, the vascularized local temporalis muscle flap appears to remain the most popular.
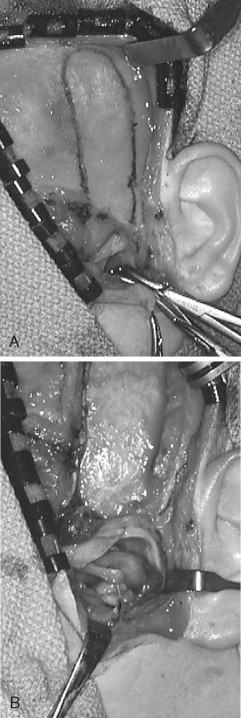
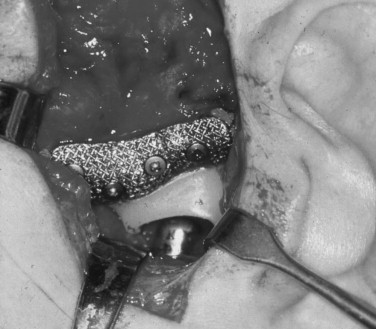
The advantages of the temporalis muscle flap are its reliable blood supply and its proximity to the TMJ. Feinberg and Larsen stated that one of the most important roles of the temporalis muscle flap is the maintenance of functional movements. Since the flap is attached to the coronoid process, when the mandible translates, the movement of the mandible pulls the muscle flap in an anterior direction, simulating the natural functional movements of the disk ( Figure 51-4 ). Investigators who performed follow-up studies on patients with temporalis muscle replacement demonstrated the presence of viable muscle tissue within the joint.
Tong and Tideman reported the re-formation of a disklike interpositional structure, after 18 months, with use of the pedicled temporalis muscle flap in four diskectomized Rhesus monkeys with osteoarthritis. They also reported a milder degree of osteoarthritis was observed histologically in the joints in which the graft survived (three of the four monkeys).
However, Henry and Wolford presented the following contraindications for the use of the temporalis muscle/fascia graft: failed Proplast-Teflon (Vitek, Houston, TX) or Silastic (Dow Corning, Arlington, TX) with continuing foreign body giant cell reaction; rheumatoid arthritis or other high-inflammatory connective tissue diseases; progressive osteoarthritis; and two or more prior surgeries.
Auricular Cartilage.
Ioannides and Maltha reported the use of autogenous auricular cartilage led to the use of this technique in autogenous disk replacement. However, Takatsuka et al investigated histologically auricular cartilage after diskectomy in the rabbit TMJ and found fibrous adhesion of the grafted auricular cartilage to the condyle and the presence of a fibrous layer containing fragmented cartilage on the articular surface. They concluded that auricular cartilage did not appear to be an ideal material for disk replacement. Other investigators reported similar results.
In the past, autogenous tissue has been called the “gold standard” for management of primary, uncompromised TMJ reconstruction. However, because of the potential morbidity associated with harvest of autogenous tissues, the inability of these tissues to survive either the transplantation process or the functional demands of the forces applied to them, and the reasons that will be discussed below, there arose the need for the development and use of alloplastic materials to reconstruct the TMJ. This is a similar course followed by orthopedic surgery in reconstruction of other body joints.
ALLOPLASTIC TMJ RECONSTRUCTION
John Murray Carnochan, a New York surgeon, was credited with the idea of interposing alloplastic material between the surfaces of diseased, excised joints in an attempt to prevent ankylosis and promote movement and function. In 1840 he reported an attempt to mobilize a patient’s ankylosed TMJ by placing a small block of wood between the raw bony surfaces of the residual mandible after gap arthroplasty.
As one traces the use of alloplastic materials in the management of severe anatomic TMJ disease, mandibular dysfunction associated with ankylosis was the primary problem that led patients to seek treatment. Every new material that was developed was used in an attempt to manage joint ankylosis, including ankylosis of the TMJ.
In 1960 Sir John Charnley reported on the use of a total alloplastic prosthetic hip reconstruction system using a titanium-backed ultra–high-molecular-weight polyethylene acetabular cup articulating with a chromium-cobalt femoral head attached to a titanium femoral shaft component that was cemented into place with polymethylmethacrylate. Modifications of this device with the same materials, now minus the cement, have become the “gold standard” not only for hip reconstruction but also for knee and shoulder total joint replacement devices in orthopedic surgery.
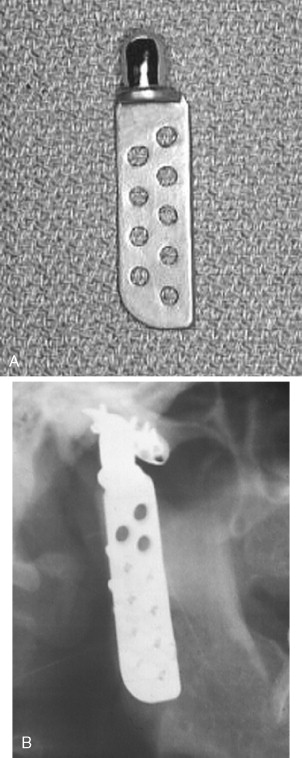
In 1963, 1964, and 1970, Christensen reported the use of a thin cast vitallium fossa-eminence prosthesis in the management of TMJ ankylosis ( Figure 51-5 ). He later added a cast vitallium ramus-condyle with a polymethylmethacrylate head to create a total joint prosthetic device ( Figure 51-6 ).

Between 1974 and 1985, there were a number of reports of partial and total alloplastic TMJ reconstructions. These were typically case reports with small numbers of patients for whom the problem was ankylosis or reconstruction after ablative malignant disease surgery. Of these, the two most significant reports were those by Kiehn and Kummoona.
In 1985 and again in 1990 S. Sonnenburg and M. Sonnenburg reported the use of a total TMJ device that consisted of a chromium-cobalt-molybdenum ramus-condyle component that articulated against an ultra–high-molecular-weight polyethylene fossa (UHMWPE). This mimicked the materials and geometry used in the design of alloplastic joint prostheses by orthopedic surgeons.
Hinds, Homsy, and Kent in 1974 reported the use of a Proplast-Teflon-coated vitallium ramus-condyle component for hemiarticulation reconstruction of the TMJ. Kent, in 1983, reported the use of a Dacron/Proplast-Teflon (VK-I) and later still a Dacron/Proplast-Teflon/ultra–high-molecular-weight polyethylene (UHMWPE) (VK-II) fossa. The ramus-condyle and fossa components were then used as a total alloplastic TMJ reconstruction prosthetic device. In 1993 Kent et al reported a long-term follow-up study of these devices ( Figure 51-7 ).
From 1990 to 1995, others reported on the development and use of alloplastic partial and total temporomandibular joint reconstruction prostheses. The indications for their use ranged from ankylosis to reconstruction after ablative surgery for disease and/or trauma to the multiply operated failed TMJ patient.
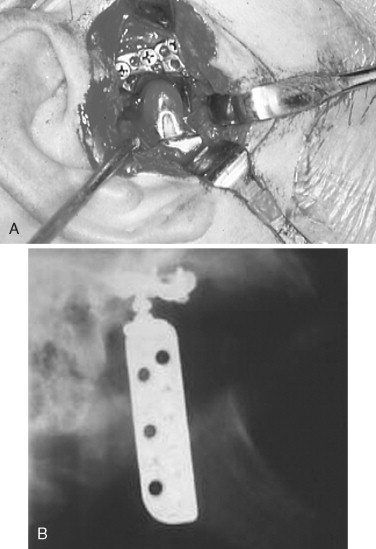
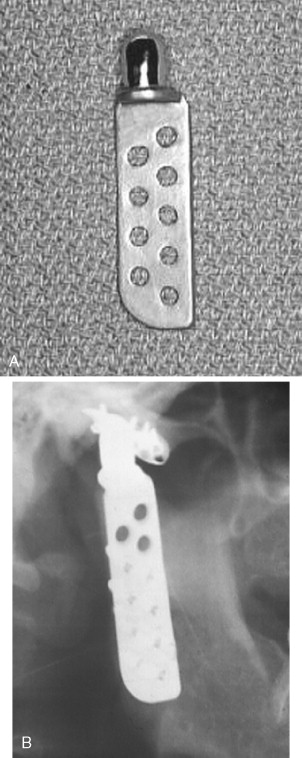
In 1993 Henry and Wolford reported prospective results with the use of the Techmedica (Camarillo, CA; now TMJ Concepts) computer assisted designed/computer aided manufactured (CAD/CAM) total alloplastic TMJ prosthesis in the management of 26 patients followed for a mean of 46 months with anatomically mutilated, functionless TMJs after Proplast-Teflon failure. Wolford, Cottrell, and Henry then reported in 1994 the use of the same device in 56 multiply operated TMJ patients followed for a mean of 30 months. Mercuri et al in 1995 reported the preliminary results in a prospective multicenter clinical study with the Techmedica prosthesis on 215 patients followed for a mean of 4 years. In 2004 Mercuri et al presented a 10-year follow-up study; and in 2006 Edibam et al reported a 14-year follow-up study of these patients ( Figure 51-8 ).
In 1995 Chase et al reported retrospective results with the use of the Christensen (TMJ Inc., Golden, CO) total TMJ alloplastic prosthesis in 21 patients followed for a mean of 2.4 years. Garrett et al reported the use of a custom modification of the standard Christensen total alloplastic TMJ prosthesis for use in 20 multiply operated patients followed for a mean of 7.5 months. In 2000 Gerard and Hudson reported on the use of the metal-to-metal modified Christensen device implanted in 23 patients followed for a mean of 26 months ( Figure 51-9 ).
Wolford et al presented the first comparison of pre- and postoperative subjective and objective domains from similar groups of patients implanted with two different total TMJ alloplastic prostheses: Techmedica (now, TMJ Concepts, Ventura, CA) and Christensen (TMJ, Inc.). These authors found statistically significant better outcomes in both domains in patients implanted with the Techmedica prostheses than the Christensen.
All implanted alloplastic devices (dental implants, orthopedic and TMJ prostheses) depend on the principle of osseointegration of the components for their ultimate stability and longevity. Osseointegration implies the direct incorporation of the implant by the bone without the preliminary phase of fibrous tissue in-growth. The requirements for osseointegration are essentially the same as for primary fracture healing—the transmission of forces from the implant to the bone and vice versa must occur without relative motion or without intermittent loading. Therefore, just as with a dental implant, the most important principle in total joint alloplastic reconstruction is primary stability of the device components from the moment of their implantation.
In orthopedic surgery, total joint alloplastic devices can be initially stabilized by press-fitting or cementation into the cancellous shaft of the host long bone. Unfortunately, in the case of the TMJ, the anatomy of both the mandible and the temporal glenoid fossa does not provide these options. Therefore screw fixation of both the fossa and the ramus/condyle components of all TMJ alloplastic devices must be utilized for initial fixation and stabilization.
Compounding the stability problems in the TMJ area is the fact that most patients presenting with indications for total TMJ alloplastic reconstruction have distorted anatomy caused either by numerous failed prior surgical interventions/materials or by primary or secondary joint pathology. This makes it extremely difficult to reconstruct such cases with a stock or “off-the-shelf” or so-called “stock” device.
Either all stock devices must be bent to fit or shimmed with bone or alloplastic cement, or precious host bone must be removed to develop some reasonable host bone contact with the components of those devices. Both of these maneuvers can lead to component material fatigue or overload, promoting early failure under functional loading and, more concerning, allow micromotion of such altered components that will interfere with osseointegration. Micromotion leads to the formation of a fibrous connective tissue interface between the altered component and the host bone, resulting in early loosening of that component and potential early catastrophic or certain later premature device failure ( Figure 51-10 ).

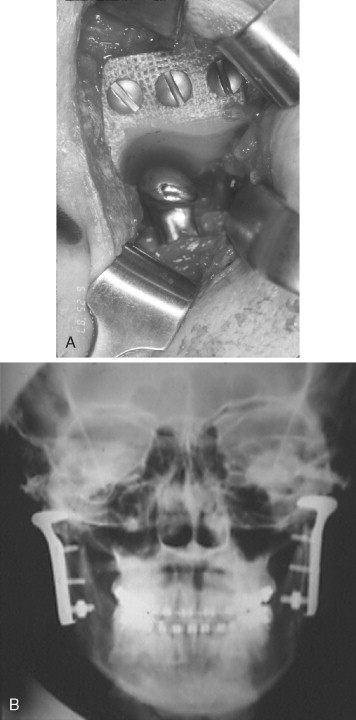
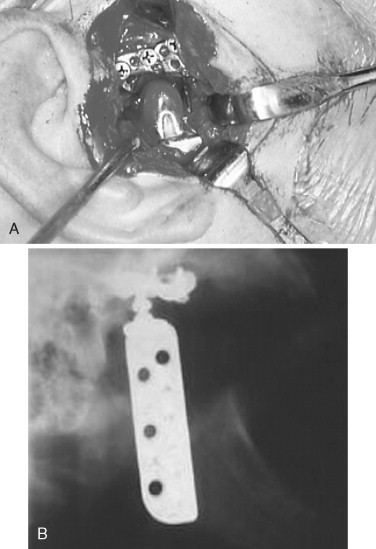
Therefore a patient-fitted or custom-made TMJ device appears to be most appropriate for such complex cases. Patient-fitted/custom-made devices, because they are designed and manufactured for each specific anatomic situation, conform to any unique anatomic situations and require no alteration or supplementation to achieve initial implantation stability. Since the components interface correctly with the host bone, the screw fixation secures the components to the host bone, mitigating any micromotion and maximizing the opportunity for osseointegration of the components and fixation screws ( Figure 51-11 ).

When calculating the cost of a procedure or device, it is important not only that the cost of the device is considered but also that all factors associated with its placement are deliberated. The major advantage of alloplastic over autogenous TMJ reconstruction is that there is no need for a second surgical site so the potential increasing morbidity and the expensive intraoperative and postoperative hospital time are greatly decreased. Therefore despite the fact that these devices are expensive, all things considered, the relative cost involved with alloplastic TMJ reconstruction overall is either equal to or ultimately less than that for autogenous TMJ reconstruction.
HISTORIC PERSPECTIVE OF TMJ RECONSTRUCTION
AUTOGENOUS TMJ RECONSTRUCTION
Bone—Vascularized and Nonvascularized
Early attempts at TMJ reconstruction involved the use of autogenous tissues. In 1909 Bardenheuer performed a mandibular condyle replacement with the fourth metatarsal. This technique was also reported in 1920 by Gillies. The use of an autogenous metatarsal head to reconstruct the mandibular condyle was also reported by Dingman in 1964, Glahn in 1967, and Spiessl in 1972. Use of a nonvascularized metatarsophalangeal joint to correct a facial deformity was reported by Entin in 1958 ( Figure 51-2 ). Datillo in 1986 and Dierks in 2000 reported the use of a vascularized metatarsophalangeal joint to reconstruct the temporomandibular joint.

TMJ reconstruction has also been performed using vascularized rib and iliac crest. Other autogenous tissues—such as fibula and iliac bone free grafts, clavicle, and sternoclavicular joint—have been used. However, none of these reports provided long-term follow-up information.
The nonvascularized costochondral free graft has been the most frequently recommended autogenous bone for the reconstruction of the TMJ because of its ease of adaptation to the recipient site, its gross anatomic similarity to the mandibular condyle, its low morbidity at the donor site, and its demonstrated growth potential in juveniles ( Figure 51-3 ).

Tissue
Vascularized and Nonvascularized Tissue.
A number of different autogenous tissues—temporalis fascia, masseter, temporalis muscle flaps, dermal grafts, and fascia lata —have been advocated as a replacement for the TMJ articular disk. However, the vascularized local temporalis muscle flap appears to remain the most popular.
The advantages of the temporalis muscle flap are its reliable blood supply and its proximity to the TMJ. Feinberg and Larsen stated that one of the most important roles of the temporalis muscle flap is the maintenance of functional movements. Since the flap is attached to the coronoid process, when the mandible translates, the movement of the mandible pulls the muscle flap in an anterior direction, simulating the natural functional movements of the disk ( Figure 51-4 ). Investigators who performed follow-up studies on patients with temporalis muscle replacement demonstrated the presence of viable muscle tissue within the joint.
Tong and Tideman reported the re-formation of a disklike interpositional structure, after 18 months, with use of the pedicled temporalis muscle flap in four diskectomized Rhesus monkeys with osteoarthritis. They also reported a milder degree of osteoarthritis was observed histologically in the joints in which the graft survived (three of the four monkeys).
However, Henry and Wolford presented the following contraindications for the use of the temporalis muscle/fascia graft: failed Proplast-Teflon (Vitek, Houston, TX) or Silastic (Dow Corning, Arlington, TX) with continuing foreign body giant cell reaction; rheumatoid arthritis or other high-inflammatory connective tissue diseases; progressive osteoarthritis; and two or more prior surgeries.
Auricular Cartilage.
Ioannides and Maltha reported the use of autogenous auricular cartilage led to the use of this technique in autogenous disk replacement. However, Takatsuka et al investigated histologically auricular cartilage after diskectomy in the rabbit TMJ and found fibrous adhesion of the grafted auricular cartilage to the condyle and the presence of a fibrous layer containing fragmented cartilage on the articular surface. They concluded that auricular cartilage did not appear to be an ideal material for disk replacement. Other investigators reported similar results.
In the past, autogenous tissue has been called the “gold standard” for management of primary, uncompromised TMJ reconstruction. However, because of the potential morbidity associated with harvest of autogenous tissues, the inability of these tissues to survive either the transplantation process or the functional demands of the forces applied to them, and the reasons that will be discussed below, there arose the need for the development and use of alloplastic materials to reconstruct the TMJ. This is a similar course followed by orthopedic surgery in reconstruction of other body joints.
ALLOPLASTIC TMJ RECONSTRUCTION
John Murray Carnochan, a New York surgeon, was credited with the idea of interposing alloplastic material between the surfaces of diseased, excised joints in an attempt to prevent ankylosis and promote movement and function. In 1840 he reported an attempt to mobilize a patient’s ankylosed TMJ by placing a small block of wood between the raw bony surfaces of the residual mandible after gap arthroplasty.
As one traces the use of alloplastic materials in the management of severe anatomic TMJ disease, mandibular dysfunction associated with ankylosis was the primary problem that led patients to seek treatment. Every new material that was developed was used in an attempt to manage joint ankylosis, including ankylosis of the TMJ.
In 1960 Sir John Charnley reported on the use of a total alloplastic prosthetic hip reconstruction system using a titanium-backed ultra–high-molecular-weight polyethylene acetabular cup articulating with a chromium-cobalt femoral head attached to a titanium femoral shaft component that was cemented into place with polymethylmethacrylate. Modifications of this device with the same materials, now minus the cement, have become the “gold standard” not only for hip reconstruction but also for knee and shoulder total joint replacement devices in orthopedic surgery.
In 1963, 1964, and 1970, Christensen reported the use of a thin cast vitallium fossa-eminence prosthesis in the management of TMJ ankylosis ( Figure 51-5 ). He later added a cast vitallium ramus-condyle with a polymethylmethacrylate head to create a total joint prosthetic device ( Figure 51-6 ).

Between 1974 and 1985, there were a number of reports of partial and total alloplastic TMJ reconstructions. These were typically case reports with small numbers of patients for whom the problem was ankylosis or reconstruction after ablative malignant disease surgery. Of these, the two most significant reports were those by Kiehn and Kummoona.
In 1985 and again in 1990 S. Sonnenburg and M. Sonnenburg reported the use of a total TMJ device that consisted of a chromium-cobalt-molybdenum ramus-condyle component that articulated against an ultra–high-molecular-weight polyethylene fossa (UHMWPE). This mimicked the materials and geometry used in the design of alloplastic joint prostheses by orthopedic surgeons.
Hinds, Homsy, and Kent in 1974 reported the use of a Proplast-Teflon-coated vitallium ramus-condyle component for hemiarticulation reconstruction of the TMJ. Kent, in 1983, reported the use of a Dacron/Proplast-Teflon (VK-I) and later still a Dacron/Proplast-Teflon/ultra–high-molecular-weight polyethylene (UHMWPE) (VK-II) fossa. The ramus-condyle and fossa components were then used as a total alloplastic TMJ reconstruction prosthetic device. In 1993 Kent et al reported a long-term follow-up study of these devices ( Figure 51-7 ).

From 1990 to 1995, others reported on the development and use of alloplastic partial and total temporomandibular joint reconstruction prostheses. The indications for their use ranged from ankylosis to reconstruction after ablative surgery for disease and/or trauma to the multiply operated failed TMJ patient.
In 1993 Henry and Wolford reported prospective results with the use of the Techmedica (Camarillo, CA; now TMJ Concepts) computer assisted designed/computer aided manufactured (CAD/CAM) total alloplastic TMJ prosthesis in the management of 26 patients followed for a mean of 46 months with anatomically mutilated, functionless TMJs after Proplast-Teflon failure. Wolford, Cottrell, and Henry then reported in 1994 the use of the same device in 56 multiply operated TMJ patients followed for a mean of 30 months. Mercuri et al in 1995 reported the preliminary results in a prospective multicenter clinical study with the Techmedica prosthesis on 215 patients followed for a mean of 4 years. In 2004 Mercuri et al presented a 10-year follow-up study; and in 2006 Edibam et al reported a 14-year follow-up study of these patients ( Figure 51-8 ).
In 1995 Chase et al reported retrospective results with the use of the Christensen (TMJ Inc., Golden, CO) total TMJ alloplastic prosthesis in 21 patients followed for a mean of 2.4 years. Garrett et al reported the use of a custom modification of the standard Christensen total alloplastic TMJ prosthesis for use in 20 multiply operated patients followed for a mean of 7.5 months. In 2000 Gerard and Hudson reported on the use of the metal-to-metal modified Christensen device implanted in 23 patients followed for a mean of 26 months ( Figure 51-9 ).
Wolford et al presented the first comparison of pre- and postoperative subjective and objective domains from similar groups of patients implanted with two different total TMJ alloplastic prostheses: Techmedica (now, TMJ Concepts, Ventura, CA) and Christensen (TMJ, Inc.). These authors found statistically significant better outcomes in both domains in patients implanted with the Techmedica prostheses than the Christensen.
All implanted alloplastic devices (dental implants, orthopedic and TMJ prostheses) depend on the principle of osseointegration of the components for their ultimate stability and longevity. Osseointegration implies the direct incorporation of the implant by the bone without the preliminary phase of fibrous tissue in-growth. The requirements for osseointegration are essentially the same as for primary fracture healing—the transmission of forces from the implant to the bone and vice versa must occur without relative motion or without intermittent loading. Therefore, just as with a dental implant, the most important principle in total joint alloplastic reconstruction is primary stability of the device components from the moment of their implantation.
In orthopedic surgery, total joint alloplastic devices can be initially stabilized by press-fitting or cementation into the cancellous shaft of the host long bone. Unfortunately, in the case of the TMJ, the anatomy of both the mandible and the temporal glenoid fossa does not provide these options. Therefore screw fixation of both the fossa and the ramus/condyle components of all TMJ alloplastic devices must be utilized for initial fixation and stabilization.
Compounding the stability problems in the TMJ area is the fact that most patients presenting with indications for total TMJ alloplastic reconstruction have distorted anatomy caused either by numerous failed prior surgical interventions/materials or by primary or secondary joint pathology. This makes it extremely difficult to reconstruct such cases with a stock or “off-the-shelf” or so-called “stock” device.
Either all stock devices must be bent to fit or shimmed with bone or alloplastic cement, or precious host bone must be removed to develop some reasonable host bone contact with the components of those devices. Both of these maneuvers can lead to component material fatigue or overload, promoting early failure under functional loading and, more concerning, allow micromotion of such altered components that will interfere with osseointegration. Micromotion leads to the formation of a fibrous connective tissue interface between the altered component and the host bone, resulting in early loosening of that component and potential early catastrophic or certain later premature device failure ( Figure 51-10 ).

Therefore a patient-fitted or custom-made TMJ device appears to be most appropriate for such complex cases. Patient-fitted/custom-made devices, because they are designed and manufactured for each specific anatomic situation, conform to any unique anatomic situations and require no alteration or supplementation to achieve initial implantation stability. Since the components interface correctly with the host bone, the screw fixation secures the components to the host bone, mitigating any micromotion and maximizing the opportunity for osseointegration of the components and fixation screws ( Figure 51-11 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


