Transposition of the maxillary canine and the lateral incisor is a complex dental anomaly to treat. The difficulty increases if the treatment aims to correct the transposition. These case reports describe 2 patients with transposition of the maxillary lateral incisor and canine. The first case involves bilateral incomplete transpositions, and the second is a complete transposition. The radiographic appearance of the canine was similar in the 2 patients. However, the treatments were distinct because of the 3-dimensional positions of the teeth. The first case involved palatally placed lateral incisor roots. To prevent resorption of the lateral incisors, the canines were moved into position buccally. In the second case, the lateral incisor root had a buccal position, and the canine crown was tractioned palatally. The position of the lateral incisor root was critical when electing the correct treatment and mechanics for each patient.
Highlights
- •
This report compares 2 patients with lateral incisor-canine transpositions.
- •
The incisor root was positioned palatally in 1 patient and buccally in the other.
- •
Both patients needed surgical exposure.
- •
The canine was tractioned buccally in 1 patient and palatally in the other.
- •
Full correction was achieved in both patients.
Tooth transposition is the positional interchange of 2 adjacent teeth or the development or eruption of a tooth in a position occupied normally by a nonadjacent tooth. Although evidence has been found of transpositions in prehistoric skulls, the cause of a transposition is still unknown. Genetic inheritance, previous trauma, alteration in the position of the dental lamina, or retention of the deciduous canine are current etiologic theories. The incidence of transpositions in the population is low (0.2%-0.38%). Most transpositions occur in the maxilla (76%), of which 88% are unilateral. The canine is involved in 90% of transpositions, most commonly with the first premolar (71%) or the maxillary lateral incisor (20%). Transpositions are classified as complete when both teeth have been entirely transposed or incomplete when only the crowns or the roots have interchanged positions.
Current diagnosis relies on clinical and radiographic observations. Two-dimensional radiography allows predictions about the position and amount of resorption; however, cone-beam computer tomography (CBCT) improves visualization of the transposition, resorption, and associated risks.
Because of low prevalence rates, robust trials regarding the most effective treatment and timing of treatment are not available. The following treatment options remain: (1) no treatment, (2) interception involving extraction of the deciduous canines, (3) extraction of 1 transposed tooth if extraction is required for correction of the malocclusion, (4) alignment of the teeth in the transposed position and subsequent restorative treatment for camouflage, and (5) orthodontic correction of the transposed teeth.
The 2 cases presented involve canine and lateral incisor transpositions in the maxilla: one was bilateral and incomplete, and the second was a complete transposition as classified in the literature. The differing tooth anatomies of the canine and the lateral incisor make this type of transposition more complex because of esthetic and functional considerations. The treatment option chosen for both patients was orthodontic correction. Although these cases involved the same teeth and both patients opted for the same treatment, the sequences of mechanics were different because of the position of the lateral incisor root in relation to the canine crown. The patients were informed of the associated risks and treatment alternatives.
Patient 1
Diagnosis and etiology
A 12-year-old boy came for an initial orthodontic assessment. It was noted on palpation that the maxillary left and right canines were buccally positioned between the respective central incisor and lateral incisor. A complete set of orthodontic records was taken. There was no relevant medical history.
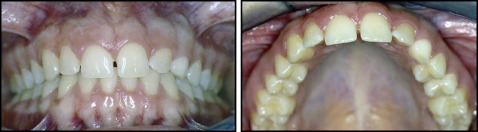
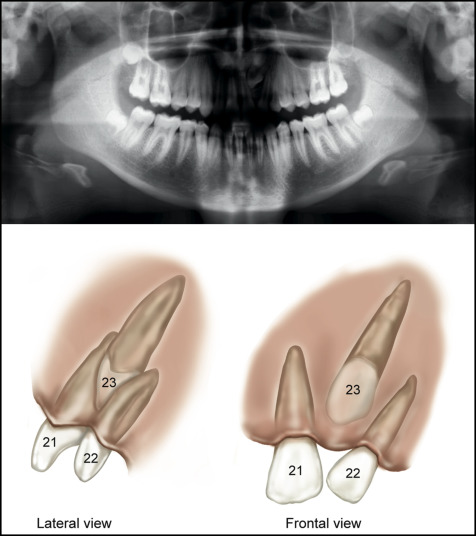
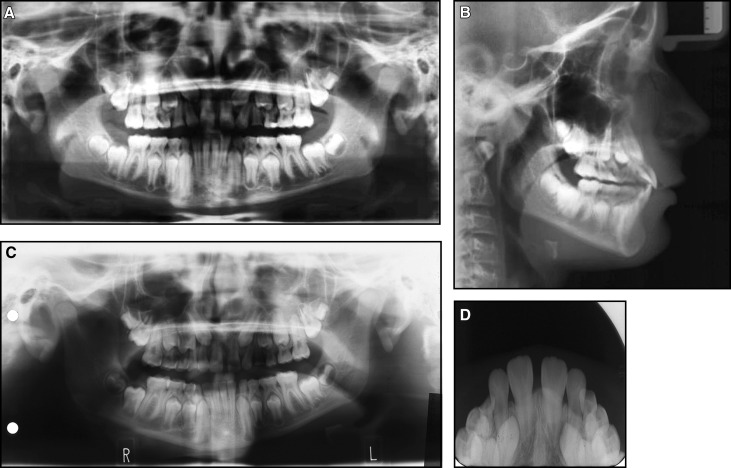
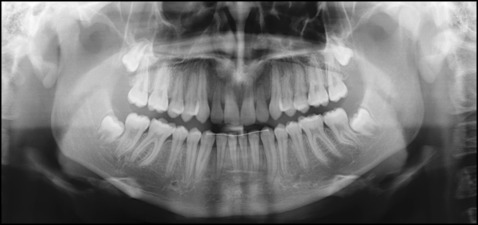
Intraoral photos showed a Class I mixed dentition, with delayed exfoliation of posterior deciduous teeth including the maxillary canines. The maxillary arch was spaced with a midline diastema associated with a low frenal attachment and proclination of the maxillary incisors. The photographs were taken in centric relation, but in occlusion there was a unilateral crossbite caused by a functional shift ( Fig 1 ). The panoramic radiograph confirmed the presence of all teeth but demonstrated generalized delayed eruption of the permanent dentition. The crowns of the canines were transposed with the roots of the lateral incisors. The right side was an incomplete transposition, and the left side was nearing a complete transposition but with favorable distal angulations and apex positions for correction. The lateral incisor roots had evidence of resorption. The lateral cephalometric radiograph also confirmed that the canine crowns were positioned buccal to the lateral incisor roots ( Fig 2 , A and B ). Radiographs forwarded from the previous clinic ( Fig 2 , C and D ) confirmed the buccal position of the canines with the parallax technique. Comparison of the panoramic radiographs confirmed that the bilateral transposition was progressing toward a complete transposition, and resorption on the roots of the lateral incisors was active.

Treatment objectives
The patient was treated in 2 phases. The objective of the first phase of treatment was to correct the bilateral transpositions with closed exposure of the canines and fixed orthodontics in the maxillary arch only. The objectives of the second phase of treatment were to (1) correct the crossbite, (2) level and align the arches while maintaining correct overjet and overbite, (3) correct the center line, and (4) achieve Class I molar and canine relationships. The overall objective was to provide the patient with improved esthetics and a functioning occlusion.
Treatment alternatives
Other alternatives were also considered, including extraction of 1 transposed tooth. This was deemed not ideal because the malocclusion did not require extraction. Extracting a transposed tooth and later replacing it with an implant was not an option because of the esthetics, function, and financial cost to the patient. Another alternative was alignment of the teeth in the transposed position and subsequent camouflage. This was also rejected because correction gives better final esthetic and functional results with less long-term maintenance. No treatment was also considered. The risk of damage to the roots of the lateral incisors or the central incisors meant that interception was required. The need for treatment was increased because the transpositions were bilateral.
Treatment progress
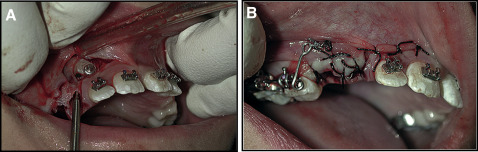
In the first phase, fixed appliances (Roth 0.022 × 0.028-in slot) were placed in the maxillary arch with a quad-helix for crossbite correction. The surgical procedure was bilateral closed exposure under local anesthesia, performed by an author (P.L.). The maxillary right deciduous canine was extracted at the start of the procedure. The buccal mucoperiostial flap was designed to cause minimal damage to the papillae. Three incisions were made to raise the flap. The first incision was along the alveolar ridge, the second was mesial to the deciduous second molar perpendicular to the alveolar ridge and approximately 12 mm in height, and the third incision was distal to the lateral incisor perpendicular to the alveolar ridge and 5 mm in height. The flap was raised to uncover the canine crown. Bone removal allowed exposure of the canine’s buccal surface to facilitate bonding of a button ( Fig 3 , A ). A metallic ligature wire (0.012-in stainless steel) with eyelets to facilitate traction was attached to the button. The mucoperiosteal flap was sutured into position. A buccal arm (0.019 × 0.025-in rectangular stainless steel wire) extended from the accessory buccal tube with an L-shaped spring ( Fig 3 , B ). Activation took place every 2 to 3 weeks with elastic thread. To minimize further resorption of the lateral incisor roots, the canine crowns were tractioned from the buccal aspect with a distoapical vector, allowing the canine crown to move past the root of the incisor to the widest part of the dentoalveolar process in a controlled manner. Once the correct sequence of the teeth in the first quadrant had been achieved, a second buccal arm tractioned the canine vertical to its correct position in the arch ( Fig 4 , A ). In the second quadrant, swapping the positions of the teeth was facilitated by moving the lateral incisor palatally to allow distal movement of the canine with an L-shaped buccal spring arm ( Fig 4 , B ). Once the canines were uprighted and clear of the lateral incisor roots, the lateral incisors were fully incorporated into the archwire ( Fig 4 , C ). Toward the end of treatment, increased labial-palatal torque was placed on the lateral incisors using a Warren anterior torquing spring followed by final settling.

Treatment results
After 25 months of active treatment, the patient was debonded. The treatment was extremely complex but gave him excellent esthetic and functional results with a good long-term prognosis. Intraoral posttreatment records show that the canines were successfully aligned and the transposition corrected. The gingival levels of both canines were anatomically correct with no recession, buccally or palatally. The final torque and color of the canines were clinically pleasing. Class I molar and canine relationships were achieved bilaterally with ideal overjet and overbite ( Fig 5 ). The radiographic assessment shows successful correction of the transpositions with good parallelism of the roots. The lateral incisors’ root lengths were similar when compared with the pretreatment radiographs, and minimal resorption occurred during the treatment ( Fig 6 ).

Patient 2
Diagnosis and etiology
A 15-year-old girl was referred for evaluation of an unerupted permanent canine in the maxillary left quadrant. When the dentoalveolar process was palpated buccally, a transposition was suspected. There was nothing of note in the medical or social history.
Full orthodontic records were taken. In the intraoral photographs, a molar Class I relationship was evident bilaterally. Spacing was present in the maxillary arch with a median diastema. The buccal position of the lateral incisor root was confirmed from clinical palpation and the inclination of its crown ( Fig 7 ). The panoramic radiograph showed that all teeth were present except the maxillary left third molar. The transposition was evident in the second quadrant. The position of the maxillary lateral incisor root was buccal and distally angulated. The transposed canine was palpable buccally, although because of the lack of a bulge, it was almost in the line of the arch, as shown in Figure 8 .