The term temporomandibular joint disorder (TMD) describes a condition that involves temporomandibular joint (TMJ) pain and dysfunction. TMD may arise from a muscular disorder or may involve the joint itself or any of its associated structures. Effective management of TMD becomes more critical, and potentially complex, when a patient presents with both myofascial pain and articular disease. deBont et al created a detailed classification system for the articular disorders of the TMJ ( Box 50-1 ).
Articular Disorders
-
Noninflammatory arthropathies
-
Osteoarthrosis
Primary
-
Chondromalacia
Secondary
-
Internal derangements
-
Condyle-eminence mobility disturbances
-
Trauma
-
Avascular necrosis
Bone and Cartilage Disorders with Articular Manifestations
-
Inflammatory arthropathies
Primary
-
Rheumatoid arthritis
-
Juvenile rheumatoid arthritis
-
Psoriatic arthritis
-
Ankylosing spondylitis
-
Seronegative polyarthritis
Secondary
-
Synovitis
-
Traumatic arthritis
-
Osteoarthritis
-
Crystal-induced arthropathy
Growth Disorders
-
Neoplasms
-
Developmental or acquired
-
Diffuse connective tissue disorders
-
Miscellaneous articular disorders
The earliest recognized and reported dysfunction of the TMJ involved joint ankylosis or dislocation. Another articular condition, internal derangement (ID), was first described by Hey and Davies in 1814. ID involves an abnormality of the disk-fossa relationship resulting in a mechanical disorder that creates irregular joint noises and prohibits normal, smooth condylar movements. A staging system for ID that describes the clinical and radiographic characteristics of this disorder was created by Wilkes ( Box 50-2 ).
Stage I Early
-
Clinical—Painless clicking
-
No limitation of opening
-
-
Radiographic—Mild disk displacement with early reduction; normal disk morphology
Stage II Early/Intermediate
-
Clinical—Occasional painful clicking
-
Intermittent locking
-
-
Radiographic—Mild to moderate disk displacement with late reduction
-
Mild disk deformity
-
Stage III Intermediate
-
Clinical—Joint tenderness
-
Limited opening
-
Frequent pain
-
-
Radiographic—Displaced, nonreducing disk
-
Disk deformity
-
Stage IV Intermediate/Late
-
Clinical—Chronic pain
-
Limited opening
-
-
Radiographic—Severe displacement, without reduction
-
Deformity of disk
-
Degenerative osseous changes
-
Stage V Late
-
Clinical—Variable joint pain
-
Joint crepitus
-
-
Radiographic—Nonreduction of disk with perforation of disk attachment or disk
-
Degenerative osseous changes
-
Stage I is clinically consistent with painless clicking but no limitation of jaw opening. In stage II the patient experiences occasional painful clicking and intermittent joint locking. As the patient progresses to stage III, more significant joint pain on function occurs along with restricted jaw opening. Stage IV is marked clinically by chronic pain and limited mouth opening. In stage V, the patient’s exam is positive for crepitus, episodic and variable joint pain, and restriction of opening.
The presence of parafunctional oral habits, concomitant medical and/or psychological conditions, and other past and present treatment needs to be carefully identified and considered before pursuing surgery. Proper patient selection is also a fundamental and essential aspect of TMJ surgery. Although non-surgical, conservative therapies should be undertaken, and often exhausted, before pursuing surgery, certain pathologic disorders of an articular origin are best treated by surgery, specifically TMJ dislocation, ankylosis, certain condylar fractures, neoplasms, and degenerative joint disease.
The evolution of surgery for ID is well documented in the literature. In 1887 Annandale reported the first intracapsular procedure for ID, while in 1909 Lanz reported the first use of a diskectomy for painful joint dysfunction. An array of procedures ranging from minimally invasive techniques to arthrotomy have been used to treat ID, and the benefits of each have been clearly documented. The use of TMJ arthrography was instrumental in establishing disk pathology as a factor in TMD, and studies by Dolwick elaborated on the role of various disk surgeries, such as repositioning and repair, in the treatment of ID. Yet the exact role of surgery for the management of ID still remains controversial. Detractors of surgery for ID are quick to point out that among progressive anatomic degenerative changes, TMJ pain and dysfunction can still decrease in the absence of any treatment.
This chapter discusses key elements in a patient’s history and physical exam that assist the surgeon in selecting the proper surgical candidate. The chapter also lists the goals of surgery for ID and the role of diagnostic imaging in treatment planning. Only open arthrotomy techniques are reviewed, as other minimally invasive procedures used to treat ID and TMD are covered in other chapters. Lastly, complications of surgery and the importance of postoperative physical therapy will be discussed.
HISTORY AND PHYSICAL EXAMINATION
The diagnosis of ID is achieved through a thorough history and detailed clinical examination, and an accurate diagnosis is paramount in determining either the most appropriate surgical technique or the need for surgery altogether. However, establishing the patient’s diagnosis can be an obstacle for the surgeon because each patient’s symptoms are highly individualized. Additionally, the patient may not always accurately report or describe his or her symptoms. Focused questionnaires regarding TMJ pain and dysfunction can be completed by the patient to help the surgeon rule out certain subtypes of TMDs that may not be amenable to surgery. If the patient reports a history of painful joint noises and pain on mandibular function, a diagnosis of ID is likely and surgery may be indicated. One scenario that should cause concern for the surgeon is a recent resolution of a patient’s history of joint noises in lieu of continued joint pain. This clinical picture may indicate acute disk perforation. The following are physical exam findings consistent with ID:
- 1.
Pain on palpation directly over the TMJ, particularly during joint loading
- 2.
Limitation in joint range of motion
- 3.
Deviation on opening, if unilateral
- 4.
Joint noises consistently associated with pain
- 5.
Joint crepitus
If concomitant myofascial pain or dysfunction exists, they must be specifically addressed in the comprehensive treatment of the patient. Myofascial pain may develop secondarily in patients with ID, and ID may develop secondarily in patients with myofascial pain. In cases of disk dislocation with reduction, a patient may experience significant pain while trying to move past the obstructing portion of the disk. When a patient has a unilaterally dislocated disk, the mandible will deviate to the affected side during rotation and then correct its path toward the midline once the condyle has moved past the obstruction and has reduced itself into the disk. In bilateral disk dislocation with reduction, the mandible may deviate to one side and then click. The mandible may deviate to the contralateral side and then click again.
PATHOGENESIS
Recent studies have related the molecular biology of the joint to the pathogenesis of ID. An imbalance favoring catabolic over anabolic processes has been implicated in the development of degenerative disease. Milan proposed that mechanical stresses in the joint make the TMJ susceptible to formation of free radicals, which are thought to contribute to the production of other metabolites and enzymes that promote degenerative changes. One specific free radical, nitric oxide, has been formed in increased levels in arthritic joints. Nitric oxide also promotes the formation of enzymes and prostaglandins that lead to inflammation and tissue breakdown within the joint. Nitzan hypothesized that free radical formation leads to oxidative stress, which subsequently may impair the lubrication system of the joint. The ultimate disruption of joint lubrication leads to increased friction within the joint space. Nitzan and Etsion suggested that this increased friction, attributable to a lack of disk lubrication, is what causes disk dislocation as the disk is repetitively pressed against the articular surfaces.
Synovial fluid analysis of the TMJ has shed light on the role of cytokines, proteinases, and other substances in the development of ID. Interleukins are specific cytokines that mediate inflammation and have been detected in both ID and osteoarthritis (OA) of the TMJ. Cytokines appear to contribute to tissue damage by inducing the release of proteinases and collagenases. Gruber et al reported on the possible role of one such marker, matrix metalloproteins (MMPs) produced by synoviocytes and articular chondrocytes, as mediators of cartilage degradation. Kubota et al compared the TMJ synovial fluid between asymptomatic patients and those with established ID or OA for differences in interleukin-1 beta (IL-1β) and IL-6 levels to determine whether the IL levels would reflect the pathogenesis of ID. Results indicated higher levels of IL-1β in the synovial fluid of joints with ID or OA compared to the normal, asymptomatic group. IL-β and IL-6 levels were also significantly higher in the OA group than in the ID group. This study concluded that elevated levels of cytokines can be potential markers for cartilage degradation in the TMJ. The findings from the above-mentioned studies lend support to the role of arthrocentesis or arthroscopy as the initial surgical intervention for ID such as closed lock, as lavage of inflammatory mediators and lysis of adhesions can be accomplished by either technique. Other past and more recent studies continue in their attempts to establish the role of molecular biology of the TMJ with ID.
PATHOGENESIS
Recent studies have related the molecular biology of the joint to the pathogenesis of ID. An imbalance favoring catabolic over anabolic processes has been implicated in the development of degenerative disease. Milan proposed that mechanical stresses in the joint make the TMJ susceptible to formation of free radicals, which are thought to contribute to the production of other metabolites and enzymes that promote degenerative changes. One specific free radical, nitric oxide, has been formed in increased levels in arthritic joints. Nitric oxide also promotes the formation of enzymes and prostaglandins that lead to inflammation and tissue breakdown within the joint. Nitzan hypothesized that free radical formation leads to oxidative stress, which subsequently may impair the lubrication system of the joint. The ultimate disruption of joint lubrication leads to increased friction within the joint space. Nitzan and Etsion suggested that this increased friction, attributable to a lack of disk lubrication, is what causes disk dislocation as the disk is repetitively pressed against the articular surfaces.
Synovial fluid analysis of the TMJ has shed light on the role of cytokines, proteinases, and other substances in the development of ID. Interleukins are specific cytokines that mediate inflammation and have been detected in both ID and osteoarthritis (OA) of the TMJ. Cytokines appear to contribute to tissue damage by inducing the release of proteinases and collagenases. Gruber et al reported on the possible role of one such marker, matrix metalloproteins (MMPs) produced by synoviocytes and articular chondrocytes, as mediators of cartilage degradation. Kubota et al compared the TMJ synovial fluid between asymptomatic patients and those with established ID or OA for differences in interleukin-1 beta (IL-1β) and IL-6 levels to determine whether the IL levels would reflect the pathogenesis of ID. Results indicated higher levels of IL-1β in the synovial fluid of joints with ID or OA compared to the normal, asymptomatic group. IL-β and IL-6 levels were also significantly higher in the OA group than in the ID group. This study concluded that elevated levels of cytokines can be potential markers for cartilage degradation in the TMJ. The findings from the above-mentioned studies lend support to the role of arthrocentesis or arthroscopy as the initial surgical intervention for ID such as closed lock, as lavage of inflammatory mediators and lysis of adhesions can be accomplished by either technique. Other past and more recent studies continue in their attempts to establish the role of molecular biology of the TMJ with ID.
GOALS AND CRITERIA FOR SURGERY
Surgery is reserved for patients whose TMJ pain and dysfunction are refractory to non-surgical modalities and when symptoms result in significant impairment. The goal of surgery is to preserve the articular tissues while returning the patient to a more regular diet and reestablishing a normal range of motion to the jaw. Individualized goals of surgery are discussed with each patient before undertaking any form of surgery. The American Association of Oral & Maxillofacial Surgeons (AAOMS) published the first guidelines for disk surgery in 1984 based on a literature review and the general consensus of surgeons. This document was succeeded by another in 1990 that stated the standards and criteria for TMJ surgery. TMJ arthrotomy is performed for TMJ ankylosis, trauma, previous surgery, severe degenerative disease, growth disturbances, and neoplasms. As recently as 2005, a study by Hall et al compared the outcomes of four commonly used techniques in treating ID.
Two reports by Holmlund at The Second International Consensus Meeting in 1992 have stated criteria for successful TMJ disk surgery. These criteria include the following:
- 1.
Mild, brief, or infrequent pain of no concern to the patient
- 2.
A vertical range of motion greater than 35 mm and a lateral range of motion greater than 6 mm
- 3.
Ability of the patient to eat a regular diet, at worst avoiding tough or hard foods
- 4.
Stabilization of possible degenerative imaging changes
- 5.
Absence of symptoms for at least 2 years
- 6.
Absence of significant complications
A common form of ID is closed lock. This condition is associated with either an acute or a chronic anterior disk dislocation without reduction. When TMJ arthroscopy is undertaken for this condition, adhesions are often noted in the superior joint space. These adhesions can subsequently be removed by arthroscopic techniques. Adhesions can be noted in the superior joint space particularly during diagnostic arthroscopy and then subsequently removed by arthroscopic surgery. Arthrotomy is performed for closed lock if arthroscopic techniques fail to correct the mechanical disturbance.
DIAGNOSTIC IMAGING
Hard tissue abnormalities of the TMJ are most readily identifiable by plain films and computed tomography (CT) scans. Panorex radiographs best serve as a screening tool to identify any gross bony abnormalities, while CT scans are superior to plain tomography in evaluating hard tissues. CT scans provide only limited evaluation of the soft tissues surrounding the TMJ, particularly the disk. Soft tissue disorders of the joint can also be determined by arthrography, but this is rarely performed with the advent of magnetic resonance imaging (MRI). MRI is the study of choice to evaluate ID. MRI studies differentiate the variable proton density within a given tissue volume and then use variable pulse sequences to configure images. The TMJ disk has a low signal pattern and appears black because of its low proton density. Tissues that are higher in either water or proteins appear white on an MRI, which may be indicative of tissue edema. No direct correlation has been definitively reported linking higher signal intensities of TMJ disks with perforations or other surface damage.
Studies of disk displacement or degenerative changes of the condyle have been clearly demonstrated in asymptomatic patients. Thus one must avoid overemphasizing radiographic findings so as to prevent unnecessary or overly aggressive treatment. Figure 50-1 (parts A and B ) illustrates an MRI that displays anterior disk displacement without reduction.
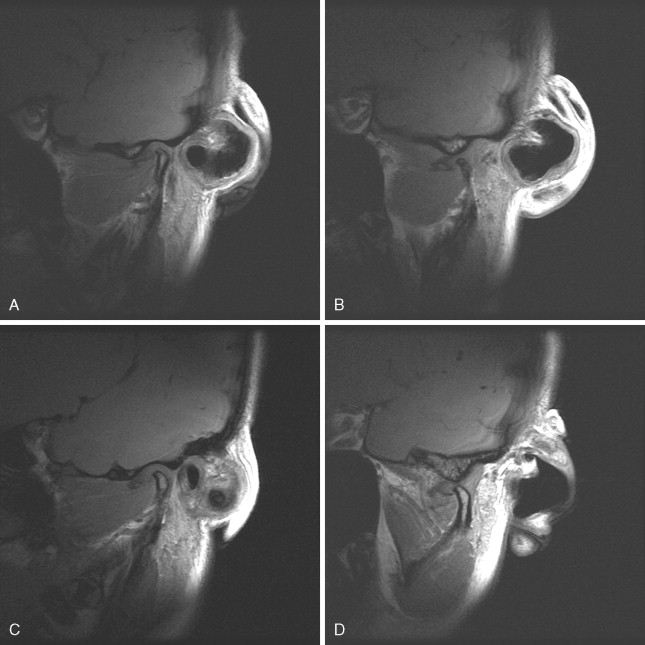
This patient was involved in a motor vehicle accident and sustained a whiplash-type injury and developed a unilateral TMD. Parts C and D of Figure 50-1 illustrate how the same patient can manifest the identical anatomic abnormality on the contralateral side. However, this patient reported no symptoms from the contralateral side.
When ordering an MRI for ID, the surgeon should request both sagittal and coronal views to accurately depict the three-dimensional aspect of ID. Sagittal views alone may not depict medial or lateral disk displacement. Liedberg and Katzberg have reported the diagnostic value of coronal MRI views in verifying disk displacement. An MRI should also be ordered in both T 1 – and T 2 -weighted images. T 1 -weighted images best depict the anatomy of the TMJ, while T 2 -weighted images allow for visualization of joint effusions. No studies have been able to consistently or accurately determine disk perforations.
PREOPERATIVE THERAPIES
Non-surgical, conservative therapies used in the treatment of TMD are covered in greater detail in other chapters of this text. Nonsteroidal anti-inflammatory drugs, a soft diet, physical therapy, splint therapy, and, when indicated, behavioral therapy are among the various non-surgical, conservative therapies that are typically implemented, and sometimes exhausted, before surgery is considered in the treatment of ID. When myofascial pain exists concurrently with ID, splint therapy may relieve one pain but aggravate another. If an anterior repositioning splint is implemented because of the presence of the ID, the patient’s myofascial pain may be aggravated. If the more common maxillary stabilization splint is fabricated, the myofascial pain may be improved, but joint pain may still exist, especially if the patient is functioning on the posterior attachment of the disk.
SURGERY
A variety of open surgical techniques exist for the treatment of ID. These include the following:
- 1.
Disk repositioning
- 2.
Disk repair
- 3.
Diskectomy alone
- 4.
Diskectomy with autologous graft replacement
- 5.
Condylotomy
The above-mentioned procedures are all performed through either a preauricular, an endaural, or a postauricular skin incision. Regarding grafting procedures, this chapter will discuss only those techniques that use autologous tissue sources, as numerous studies have concluded that the use of currently available alloplastic graft materials in TMJ surgery is unsupported. The specific arthrotomy technique chosen is usually dependent on the surgeon’s skills and experiences. The procedure should also result in the fewest complications, such as facial nerve injury, permanent occlusal changes, and relapse of joint pain and dysfunction. Another consideration is if a second surgical site is required for procurement of an autologous graft.
PREAURICULAR INCISION
The preauricular incision is commonly used and a modification of an incision designed by Blair. The incision provides maximal lateral and anterior access to the joint space. The preauricular incision is approximately 3 cm long and has a superior and inferior component, which meet at a point level with the superior aspect of the tragus. The incision is placed within a preauricular skin crease that lies posterior to the superficial temporal vessels and the auriculotemporal nerve. The vessels can be avoided by following the preauricular cartilage during the dissection. Sufficient surgical access in the inferior portion of the incision can be easily achieved by carrying the incision to a point just below the tragus, but the incision can be extended inferiorly to the level of the lobule.
The skin and subcutaneous tissues are sharply incised with a 15 blade. The superior portion of the incision is progressively dissected with mosquito hemostats down to the intensely white temporalis fascia. The inferior portion of the incision is dissected down to the lateral TMJ ligament. Since the external auditory canal is angled nearly 45 degrees anteromedially to the skin surface, the inferior portion of the dissection follows the pretragal pocket to avoid perforating into the external auditory canal. Small retractors are placed into the superior and inferior pockets. A sharp, curved Metzenbaum scissors is placed on top of the temporalis fascia and used to connect the superior and inferior pockets, and the overlying tissues are sharply incised. A flap is reflected anteriorly and superiorly, clearly exposing the temporalis fascia. This flap is then retracted anteriorly away from the tragus. A 15 blade is used to make a vertical incision through the temporalis fascia; then the dissection proceeds down to the root of the zygomatic arch. A full-thickness flap is then elevated anteriorly off of the arch until the articular eminence is visualized.
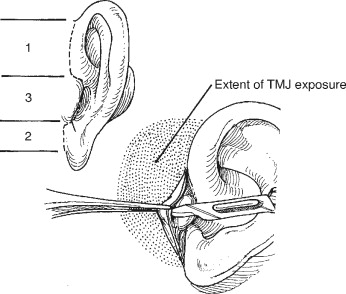
The mandible can be manipulated through a sterile drape, allowing the surgeon to become oriented and possible identify the lateral pole of the condyle. The overlying tissues are bluntly dissected with Metzenbaum scissors until the lateral capsule is identified ( Figure 50-2 ).

Small Obwegesser right angle retractors can be used inferiorly and anteriorly to expose the articular eminence and the lateral capsule. A superior extension of the preauricular incision allows access to the temporalis muscle if a temporalis muscle flap must be harvested for reconstructive purposes. The primary disadvantage of the preauricular incision is the risk of injury to the superficial temporal vessels.
ENDAURAL INCISION
The endaural incision described by Rongetti is a modification of an endaural approach first reported by Lempert for treatment of otosclerosis. The endaural incision is more aesthetic because the incision is made in the external auditory canal ( Figure 50-3 ).
However, this incision does carry the disadvantage of possible perichondritis. The superior portion of this incision begins at the junction of the face and pinna and extends to the top of the tragus. The incision is made at a 90-degree angle to the skin surface just anterior to the pinna, following the cartilage of the pinna. The inferior portion of the incision begins at the base of the tragus and extends to the junction of the lobe and the face. The tragus is retracted anteriorly and an incision is made 2 to 3 mm inside the crest of the tragus, connecting the superior and inferior incisions ( Figure 50-4 ).
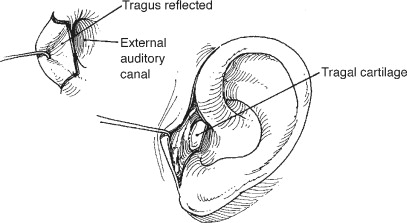
The skin is dissected off of the tragal cartilage without creating a perforation of the skin while it is being reflected over the cartilage. Metzenbaum scissors are used at the superior extent of the incision to bluntly dissect down to the temporalis fascia. The superficial temporal vessels can be avoided by closely following the cartilage of the pinna. The dissection anterior to the tragus follows a supraperichondrial plane, over the cartilage that forms the anterior wall of the external auditory canal. An important landmark during this dissection is the bony postglenoid tubercle, which is located anterior to the cartilage of the external auditory canal. The dissection along the anterior portion of the cartilaginous canal must stop at the postglenoid tubercle because the tympanic membrane is attached to the cartilaginous canal near the junction of the cartilaginous and bony canal. If the bony canal is perforated, the tympanic membrane can be injured. The plane of dissection follows that of the cartilage of the canal rather than the skin surface, or the parotid gland may be violated. Inferiorly, the dissection proceeds down to the skin just beneath the lobe. Sutures can be placed through the tragal cartilage and the superior flap to assist in retraction.
OTHER INCISIONS
Alexander described the postauricular approach for TMJ surgery. More recently Politi described a deep subfascial approach to the TMJ or zygomatic arch. The incision is a modification of the preauricular incision that follows a deep subfascial dissection, passing deep to both layers of the temporalis fascia. No injuries to the facial nerve were reported with this incision and it was not necessary to ligate any superficial temporal vessels except an occasional posterior branch of the superficial temporal artery. The deep subfascial approach was recommended in second procedures of the TMJ or in delayed surgery. The specific incision used is ultimately determined by the surgeon’s experience, as no studies have indicated that the incision affects the intended goals of the surgery.
CAPSULAR INCISIONS
Once the lateral capsule is identified, the mandible can be distracted through a sterile drape, enabling the lateral pole of the condyle to be palpated through the capsule. The capsule can be incised through any number of different incision designs to gain access to the superior joint space. The most commonly used incisions involve making an incision either over the lateral rim or just below the lateral rim of the glenoid fossa ( Figure 50-5 ).

The superior joint space is insufflated with 2 to 3 mL of epinephrine-impregnated local anesthetic through the lateral capsule. The local anesthetic will rapidly escape once the capsule is either dissected off of the rim with a periosteal elevator or incised with a scalpel. In the case of the latter design, the incision is extended anteriorly and posteriorly with a pair of sharp scissors. The surgeon should excise any adhesions within the superior joint space, but should not be overly aggressive with removing tissue from the undersurface of the fossa, as the synovial lining may be inadvertently removed.
Care must be taken not to damage the posterior attachment of the disk while dissecting the capsule. If the surgeon must access the inferior joint space, the capsule can be incised off of the disk and the periosteal elevator can reflect a flap to expose the condyle. Vertical reduction of the articular eminence can be performed to maximize the surgeon’s view of the superior joint space. Reduction typically involves removal of 4 to 5 mm of bone on the most lateral aspect of the eminence along the lateral tubercle. If necessary, an additional 1 to 3 mm of bone can be removed from the medial aspect of the eminence to optimize movement of the condyle within the fossa during the arthroplasty.
WOUND CLOSURE
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


