Introduction
Compared to the conventional approach to orthognathic surgery, “surgery first” protocols could be advantageous in terms of shortened treatment times and immediate esthetic improvement. However, consensus regarding patient selection, technical protocol, and stability is still lacking.
Methods
A systematic review of the scientific literature on surgery-first treatment (January 2000 to January 2015) was performed. The PubMED and Cochrane Library databases were accessed. Patient selection criteria, specific surgical-orthodontic protocol, treatment duration, patient and orthodontist satisfaction, and stability of results were compared with a similar population treated conventionally.
Results
The search yielded 179 publications. The application of strict selection criteria gave the final group of 11 articles. In total, 295 patients were managed with a surgery-first approach. A Class III malocclusion was the most prevalent underlying malocclusion (84.7%). Total treatment duration was shorter in surgery-first patients than in those treated conventionally. There was substantial heterogeneity among articles and high reporting bias regarding the inclusion and exclusion criteria, the orthodontic and surgical protocols, and the stability of results. A meta-analysis of combined data was not possible.
Conclusions
The surgery-first approach is a new treatment paradigm for the management of dentomaxillofacial deformity. Studies have reported satisfactory outcomes and high acceptance. However, the results should be interpreted with caution because of the wide varieties of study designs and outcome variables, reporting biases, and lack of prospective long-term follow-ups.
Highlights
- •
Surgery first represents a new treatment concept for the management of dentomaxillofacial deformity.
- •
Key reported advantages are total treatment reduction and immediate improvement of the deformity.
- •
Compared to conventional protocols, an increased instability has not been found.
- •
Consensus regarding orthodontic-surgical protocols and inclusion-exclusion criteria are lacking.
- •
The heterogeneity and low evidence level of current studies precludes a meta-analysis.
Until recently, the conventional approach to orthognathic surgery involving preoperative orthodontics, followed by surgery and postoperative orthodontics, was the sole recognized approach to orthognathic surgery. The first orthognathic surgeons realized that the amount of mandibular setback was limited by the magnitude of overjet between the maxillary and mandibular incisors. Consequently, the “orthodontics-first” concept became a widely acknowledged dogma. It emphasized that optimal surgical repositioning of the jaw was possible only after the removal of all dental compensations before surgery. Over the years, acceptable levels of stability and satisfaction with posttreatment outcomes have validated this approach.
In 1959, Skaggs raised the issue of surgical timing in relation to orthodontic treatment and suggested that surgery should precede orthodontic treatment if a satisfactory interarch relationship can be reached surgically. This is, to our knowledge, the first documented reference to what is currently known as “surgery first.” Behrman and Behrman hypothesized that when the jaw position is corrected, the normalized surrounding soft tissues—lips, cheeks, and tongue—facilitate postoperative tooth movement and reduce the length of orthodontic treatment. They illustrated this concept metaphorically with their suggestion to “build the house and then move the furniture.” Brachvogel et al defined further potential advantages of this surgery-first approach, suggesting that dental arch alignment after surgery is similar to orthodontic treatment in any Class I case, and that possible postsurgical relapse can be easily addressed with postoperative orthodontics. Whereas the case report by Nagasaka et al in 2009 is often cited as the first clinical application of this approach, an article by Dingman in 1944 reported an “improved” method for correcting mandibular prognathism based on performing surgery before orthodontics.
Subsequent research has demonstrated that compared with the traditional scheme, surgery-first protocols seem to reduce total treatment time and obtain immediate improvement of the facial profile or upper airway constriction. These factors may lead to high patient satisfaction rates from the early stages of treatment and improved cooperation during postoperative orthodontics. The observed reduction in total treatment time is related to more efficient postoperative orthodontics. It has been suggested that surgery-first patients typically require shorter orthodontic treatment times. This observation may be related to partial resolution of dentoalveolar compensation after surgery, leading to less complex orthodontic treatment. After the correction of the skeletal base discrepancy, the direction of postsurgical treatment coincides with the natural direction of spontaneous dental compensation and muscular force, thereby decreasing the time to full compensation. Moreover, orthodontic tooth movement may be facilitated by the surgically induced regional acceleratory phenomenon. This metabolic process is a complex physiologic phenomenon involving accelerated bone turnover and decreased regional mineral density.
The proposed benefits of surgery first have led to a growing acceptance in surgical and orthodontic communities toward these protocols. Nevertheless, there is currently no consensus regarding surgical protocols, specific complications or limitations of this treatment sequence, and stability of the results. Consequently, the aims of this systematic review were to analyze current protocols and results of patients treated with surgery first and to compare the outcomes with those obtained from a conventional approach.
Material and methods
The PICOS (participants, intervention, comparisons, outcomes, and study design) criteria focused on nongrowing, nonsyndromic patients with a skeletal maxillofacial deformity treated with a surgery-first approach and a similar population treated with the conventional orthognathic approach. Outcomes assessed included treatment duration, patient satisfaction, orthodontist satisfaction, and stability. Regarding the study design, a level of evidence of at least IV was required. In the level III group, case series with a sample size less than 10 were excluded.
An electronic search of PubMed and Cochrane Library databases was performed from January 2000 to January 2015. The search strategy was designed to include 2 aspects: terms related to the surgical procedure of interest (orthognathic surgery) and terms related to the specific approach of interest (surgery first). The following term sequence was used in PubMed: (“surgery first”) AND (“orthognathic surgery”) OR (“surgery first”) AND (“orthodontics” [MeSH]). No preliminary exclusion of articles based on language of publication was applied. The electronic search was augmented with manual searches of the reference lists of the selected publications.
This search strategy was undertaken independently by 2 investigators (M.A.P-G., R.G-M.). All titles obtained by the electronic searches were screened. When the title did not contain enough information for exclusion, the article was selected for abstract evaluation. Subsequently, the abstracts of all potentially relevant articles were reviewed based on the inclusion criteria. Those that apparently fulfilled these criteria and articles whose title and abstract did not contain enough relevant information were obtained in full. The Cohen kappa coefficient was used to measure interrater agreement for title and abstract selection. Full-text articles were analyzed for final inclusion with reasons for rejection noted. In case of a discrepancy between investigators, a consensus decision was made.
The methodologic quality of studies was assessed for a risk of bias independently by the same 2 investigators. Depending on the type of study—randomized or nonrandomized—the use of the Cochrane Collaboration Tool or the Newcastle-Ottawa scale for quality and risk of bias assessment was planned. In case of a discrepancy between the investigators, a consensus decision was made.
Results
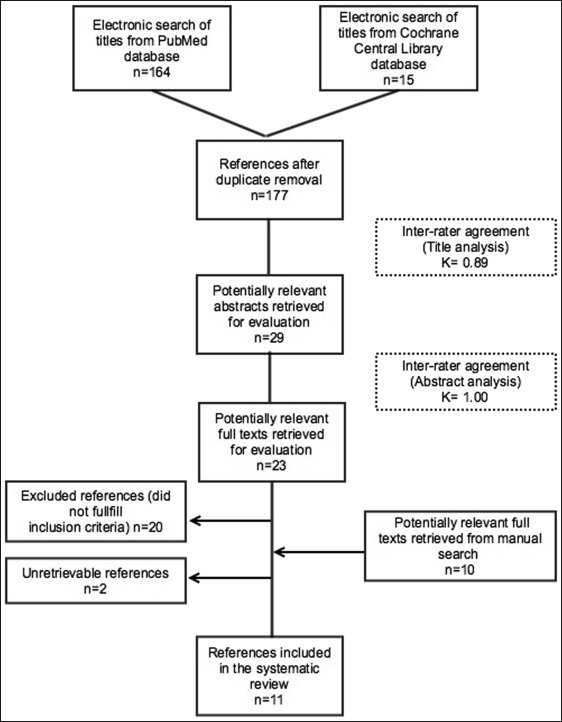
The electronic search produced 164 publications in PubMed and 15 in the Cochrane Library (total, 179). After removal of duplicates, 177 potentially relevant titles were assessed. Of these, 29 were selected for further abstract analysis (interrater agreement, κ = 0.89). Subsequently, 23 articles were retrieved for full-text evaluations. Manual search led to the inclusion of 10 additional articles ( Tables I and II ).
| Authors and year of publication | Origin | Study type | Sample size and distribution | Mean age at time of surgery (y) | Aim of study | Type of malocclusion | Type of intervention | Total treatment time (mo) | Stability or relapse |
|---|---|---|---|---|---|---|---|---|---|
| Baek et al, 2010 | South Korea | Prospective, case series | n = 11 (5 male, 6 female) | 22.95 | To evaluate surgical movement and postoperative orthodontic treatment of the SFA for the correction of skeletal Class III malocclusion. | Skeletal Class III | Bimaxillary surgery: LeFort I osteotomy (with posterior impaction of the maxilla) and BSSO for mandibular setback | 12.18 ± 3.57 | NR |
| Wang et al, 2010 | Taiwan | Retrospective, case control | n = 36 (18 CA, 18 SFA) | CA 22.3 ± 3.8 SFA 23.3 ± 4.2 |
To investigate transverse dimensional changes of the dental arches in skeletal Class III malocclusion treated with the SFA vs CA. | Skeletal Class III | Bimaxillary surgery: LeFort I osteotomy and/or BSSO | NR | NR |
| Liao et al, 2010 | Taiwan | Retrospective, case control | n = 33 (13 CA, 20 SFA) | CA 21 ± 4 SFA 23 ± 4 |
To compare the SFA vs CA in terms of treatment outcome (facial esthetics, occlusion, stability, and efficiency). | Skeletal Class III and open bite | Bimaxillary surgery: LeFort I osteotomy (with posterior impaction, with or without segmentation) and BSSO | CA 17.1 ± 3.4 SFA 11.4 ± 4.2 |
At debonding, maxillary stability was good in both the horizontal and vertical directions. In the horizontal direction, mild rmandibular relapse was found in both groups. Although the vertical mandibular stability was worse in the SFA group than in the CA group, the direction of instability was favorable for open-bite correction. |
| Ko et al, 2011 | Taiwan | Retrospective, case control | n = 53 (27 male, 26 female) 35 CA: 19 male, 16 female; 18 SFA: 8 male, 10 female |
CA 22 ± 4.1 (range, 18-34) SFA 24.6 ± 4.9 (range, 18-33) |
To compare the SFA vs CA in terms of (1) progressive dental and skeletal changes, (2) postsurgical stability, (3) treatment efficacy of skeletal Class III correction. | Skeletal Class III (ANB <0°) | Bimaxillary surgery: BSSO and 1 of these 3 options: (1) presurgical nonextraction therapy + maxillary segmentation + tooth extraction during surgery; (2) presurgical nonextraction therapy + LeFort I osteotomy with clockwise rotation; or (3) presurgical extraction therapy + LeFort I osteotomy | SFA 17.8 ± 5 CA 15.76 ± 2.7 |
NR |
| Liou et al, 2011 | Taiwan | Prospective, cohort | n = 22 | NR | To study postoperative changes in bone physiology and metabolism and the corresponding responses in the dentoalveolus. | NR | Bimaxillary surgery: LeFort 1 osteotomy and BSSO | NR | NR |
| Ko et al, 2013 | Taiwan | Retrospective, cohort | n = 45 (19 male, 26 female) | 23.2 | To identify parameters related to skeletal stability after OGS in skeletal Class III with SFA; to compare dental and skeletal variables between patients with better and worse surgical stability; and to evaluate correlations between variables and mandibular stability. | Skeletal Class III (ANB <0°) | Bimaxillary surgery: LeFort I osteotomy, BSSO, and genioplasty (the latter only in 22 subjects) | 13.9 | At debonding, 12.46% relapse. Mean B-point relapse, 1.44 mm. |
| Choi et al, 2015 | South Korea | Prospective, case control | n = 56 (16 male, 40 female) 24 CA, 32 SFA |
22.4 | To clarify the hypothesis: “OGS without presurgical orthodontics (SFA) may be as effective as the CA in correcting dentofacial deformities.” | Skeletal Class III | Bimaxillary surgery: LeFort I osteotomy with posterior impaction of the maxilla and BSSO or mandibular setback | SFA 19.4 CA 22.3 |
At 12 to 36 months follow-up, relapse rate was not statistically significant different between groups except for the lower anterior facial height ratio. |
| Hernandez-Alfaro et al, 2014 | Spain | Prospective, case series | n = 45 (18 male, 27 female) | 23.5 (range, 17-36) | To describe a specific orthodontic and surgical protocol for SFA, discuss its benefits and limitations, and update its indications. | Skeletal Class II (n = 19), skeletal Class III (n = 22), asymmetry (n = 4) | Bimaxillary surgery (n = 30): 1. LeFort I osteotomy + BSSO (n = 29) 2. LeFort I osteotomy + mandibular front-block (n = 1) Maxillary surgery (n = 11): LeFort I osteotomy Mandibular surgery (n = 4): BSSO |
10.2 | NR |
| Kim et al, 2014 | South Korea | Retrospective, cohort | n = 61 (28 male, 33 female) 38 CA, 23 SFA |
CA 21.6 ± 3.5 SFA 23 ± 6.3 |
To compare the SFA vs CA in terms of stability after mandibular setback in skeletal Class III subjects. | Skeletal Class III | Mandibular surgery: BSSO | SFA 15.4 CA 22.5 |
At debonding, mandible moved anteroinferiorly. Average amounts of anterior relapse, 1.6 mm in the CA group and 2.4 mm in the SFA group. Vertical relapse pattern was similar. Relapse >3 mm comprised 39.1% of the SFA group vs 15.8% of the CA group. Relapse <1.5 mm more dominant in CA. Significant association between degree of relapse and group difference. |
| Park et al, 2014 | South Korea | Retrospective, case control | n = 60 (24 male, 36 female) 36 CA, 24 SFA |
CA 22.4 ± 4.4 SFA 22.4 ± 4.6 |
To compare the SFA vs CA in terms of differences in the amount and pattern of maxillary incisor inclination change in skeletal Class III treated with extraction of the maxillary 1pm and bimaxillary surgery. | Skeletal Class III | Bimaxillary surgery: LeFort I osteotomy + BSSO. Maxillary 1pms were extracted during surgery in the SFA group | NR | NR |
| Kim et al, 2014 | South Korea | Retrospective, case series | n = 37 (20 male, 17 female) | 23 ± 4 | To evaluate postoperative stability of the treatment of mandibular prognathism treated with the SFA (with IVRO instead of BSSO for the mandible). | Skeletal Class III | Bimaxillary surgery: LeFort I osteotomy + IVRO | 14 ± 6 | At debonding, postoperative changes in skeletal variables were measured for 1 year postoperatively and showed no remarkable changes of the maxillary position in either plane. The mandible had no significant relapse horizontally, but vertical relapse was significant at all time intervals, particularly during the first 6 months postoperatively. Both anterior and posterior facial heights were decreased 1 year postoperatively, and most changes occurred during the first 6 months postoperatively. |
| Authors and year of publication | Preoperative orthodontic preparation | Preoperative orthodontic appliance used for SFA | Postoperative orthodontic protocol | Mean postoperative orthodontic treatment time | Postoperative splint use/intermaxillary fixation |
|---|---|---|---|---|---|
| Baek et al, 2010 | NR | Passive surgical wires bonded directly to tooth surface or ligated to brackets. | NR | 8.91 ± 3.14 months | 4 weeks |
| Wang et al, 2010 | 1-2 weeks | 0.022 × 0.028-in preadjusted appliance and sliding mechanics bonded without forces. | NR | NR | NR |
| Liao et al, 2010 | 1 month | 0.022 × 0.028-in brackets are bonded, and 1-3 days before surgery, a 0.016 × 0.022 NiTi wire was placed. | Orthodontic treatment was initiated immediately after surgery because the active archwire was left in place. For segmental surgery patients, sectional archwires were replaced with continuous archwires. If there was a shift to an undesirable bite, occlusal adjustment or light elastics were used to stabilize jaw position. Incomplete arch coordination can be assisted by light transpalatal elastics, an active palatal arch, or an active lingual arch. Once alignment, leveling, and coordination were achieved, 0.016 × 0.022 SS was used. Incomplete incisor decompensation can be assisted by Class II elastics. |
NR | NR |
| Ko et al, 2011 | SFA 21 ± 4.5 days CA 154 ± 59.3 days |
Full bonding and passive 0.016-in SS archwire. | NR | NR | NR |
| Liou et al, 2011 | NR | NR | NR | NR | NR |
| Ko et al, 2013 | NR | NR | NR | 12.2 months | NR |
| Choi et al, 2015 | NR | Application of 1 bracket for intermaxillary fixation | NR | NR | NR |
| Hernandez-Alfaro et al, 2014 | 1 week | Full bonding 1 week preoperatively and placement of a soft arch the day before surgery | Initiation of orthodontic treatment 2 weeks postsurgery; archwire change every 2-3 weeks. | 9.5 months (range, 6-13) | Fixation of end splint to maxilla (2 weeks) only in the case of maxillary segmental surgery. |
| Kim et al, 2014 | CA 12.9 months SFA 1 month |
Full bonding without archwire | Both groups received the same postoperative management. Use of intermaxillary elastics. |
SFA 14.3 months CA 9.6 months (but 12.9 months of preoperative orthodontics) |
Use of intermaxillary elastics and an interocclusal splint for 4-6 weeks. |
| Park et al, 2014 | NR | NR | NR | NR | NR |
| Kim et al, 2014 | 2-3 weeks | Full bonding (archwires placed preoperatively for surgical anchorage) | Postoperative active physiotherapy with Class II elastics (2 weeks) followed by orthodontic treatment. | 12 ± 6 months | Intermaxillary fixation for 2 weeks followed by active physiotherapy using Class II elastics until the patient could open the mouth at least 30 mm, with confirmation of a stable occlusion with a surgical wafer. |
Application of the inclusion criteria caused the exclusion of 21 articles. One publication was not retrievable. Eleven articles fulfilled the inclusion criteria and were selected for systematic analysis. The PRISMA flow diagram ( Fig 1 ) gives an overview of the selection process. Table I summarizes the sample’s demographic characteristics, aims, clinical characteristics, types of intervention, total treatment times, and stability for each study. Table II summarizes the orthodontic protocols and splint use.
This systematic review included 5 case-control studies, 3 cohort studies, and 3 case series. Seven studies were retrospective, and 4 were prospective. The majority of the studies were undertaken in Asia (91%).
Since no clinical trials were retrieved, methodologic quality could not be assessed with the Cochrane Collaboration tool. For case-control and cohort studies, the Newcastle-Ottawa scale was applied ( Table III ).
| Authors and year of publication | Study type | Sample size and distribution | Newcastle-Ottawa scale outcome (range, 0-9) |
|---|---|---|---|
| Baek et al, 2010 | Prospective, case series | 11 | NA |
| Wang et al, 2010 | Retrospective, case control | 36 (18 CA, 18 SFA) | 6 |
| Liao et al, 2010 | Retrospective, case control | 33 (13 CA, 20 SFA) | 6 |
| Ko et al, 2011 | Retrospective, case control | 53 (35 CA, 19 SFA) | 5 |
| Liou et al, 2011 | Prospective, cohort | 22 | 7 |
| Ko et al, 2013 | Retrospective, cohort | 45 | 7 |
| Choi et al, 2015 | Prospective, case control | 56 (24 CA, 32 SFA) | 6 |
| Hernández-Alfaro et al, 2014 | Prospective, case series | 45 | NA |
| Kim et al, 2014 | Retrospective, cohort | 61 (38 CA, 23 SFA) | 7 |
| Park et al, 2014 | Retrospective, case control | 60 (36 CA, 24 SFA) | 4 |
| Kim et al, 2014 | Retrospective, case series | 37 | NA |
Information concerning total treatment duration was absent in 3 articles. Patient and orthodontist satisfaction was assessed in only 1 publication. Only 3 articles provided complete and detailed information about orthodontic measures. Only 1 study reported stability outcomes at follow-ups of 1 and 3 years ; the rest evaluated the results at appliance removal only.
The included studies focused on (1) assessment of postoperative consequences in terms of skeletal changes, dental changes, esthetic changes, or physiologic changes ; (2) assessment of stability ; (3) assessment of satisfaction ; and (4) report of a specific protocol.
Overall, in the 11 selected articles, a total of 295 patients with a mean age of 23.13 years at the time of surgery were treated with a surgery-first approach. The sample sizes ranged from 11 to 45 subjects, with ages from 16 to 36 years, although 1 study failed to report information concerning age.
Regarding the type of malocclusion, Class III was the most prevalent (84.7%; Table I ). Only 1 article reported on different types of malocclusion: 19 skeletal Class II patients (6.4% of the total sample), 4 with skeletal asymmetry (1.4%), and the remaining 22 patients were skeletal Class III. Liou et al did not specify the types of malocclusions included in their research.
A total of 239 patients (84.7%) underwent bimaxillary surgery ( Tables I and II ). A LeFort I osteotomy (segmented or not) and a bilateral sagittal split osteotomy were performed in 201 patients (68.1%). One study group reported intraoral vertical ramus osteotomy without segment fixation in 37 patients (12.5%). One patient (0.3%) was managed with a LeFort I osteotomy plus a mandibular front-block osteotomy. Eleven patients (3.7%) received an isolated LeFort I osteotomy, and 45 (15.2%) underwent isolated bilateral sagittal split osteotomy.
Postoperatively, the final splint was left in place as a means of occlusal stabilization for 4 to 6 weeks in 2 studies. Hernandez-Alfaro et al restricted final splint fixation to maxillary segmental cases. Kim et al maintained maxillomandibular fixation without a splint for 2 weeks, followed by active use of intermaxillary elastics.
In the surgery-first approach, fixed orthodontic appliances were typically placed 1 to 6 weeks preoperatively ( Table II ). One study group bonded a single bracket for surgical fixation, and another bonded the arch directly to the teeth in some patients.
Most articles reported the use of a manufactured passive wire. The arch was installed 2 to 3 weeks preoperatively in 1 study and at an average of 21 ± 4.5 days before surgery in another study. Two study groups did not place an arch preoperatively. Placement of a soft arch 1 day before surgery, or between 1 and 3 days before surgery, was mentioned. In 3 publications, details about orthodontic preparation were lacking.
Only 3 articles provided information about postoperative orthodontic treatment. According to the protocol followed by Hernandez-Alfaro et al, orthodontic movements started 2 weeks after surgery, and archwire changes took place every 2 to 3 weeks. Kim et al maintained maxillomandibular fixation plus active physiotherapy with Class II elastics until mouth opening reached 30 mm with confirmation of a stable occlusion using a surgical wafer, followed by postoperative orthodontic treatment. Liao et al began postsurgical orthodontics immediately after surgery because the active archwire was left in place. For patients receiving segmental surgery, sectional archwires were replaced with continuous archwires at the first postsurgical orthodontic appointment or at the time of surgery. The authors specified that if there was a shift to a convenience bite, occlusal adjustment or light elastics were used to guide and stabilize the jaw position. Incomplete arch coordination was managed with light transpalatal elastics, an active palatal arch, or an active lingual arch. Once alignment, leveling, and coordination were achieved, a 0.016 × 0.022-in stainless steel wire was placed. Incomplete incisor decompensation was addressed with Class II elastics.
Three articles reported the use of miniscrews to facilitate postoperative orthodontic treatment. Four to 8 miniscrews were placed, depending on whether the maxillary osteotomy was undertaken segmentally.
The mean total duration of treatment after the surgery-first approach was 14.2 months (range, 10.2-19.4 months). Based on comparative studies in which surgery first was compared with the conventional approach, total treatment time was longer in the conventional group (mean, 20.16 months; range, 15.7-22.5 months).
The reported advantages and disadvantages of the surgery-first approach are given in Table IV .
| Advantages | Disadvantages |
|---|---|
|
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


