SPECIAL SOFT TISSUE INJURIES
The “Goesinto” principle becomes markedly magnified when treating the soft tissue of the face. This area of the body houses multiple highly specialized visceral afferent and efferent sensory end organs with their accompanying neurovascular and anatomic support systems. Because these structures have specialized needs for repair, returning the patient to normal form and function often presents a quandary to the clinician. The following discussion will be presented in a segregated fashion for given special anatomic structures to provide the oral and maxillofacial surgeon some contemporary update on treatment and care for this unique area of the human called the face.
NASAL SOFT TISSUE INJURIES
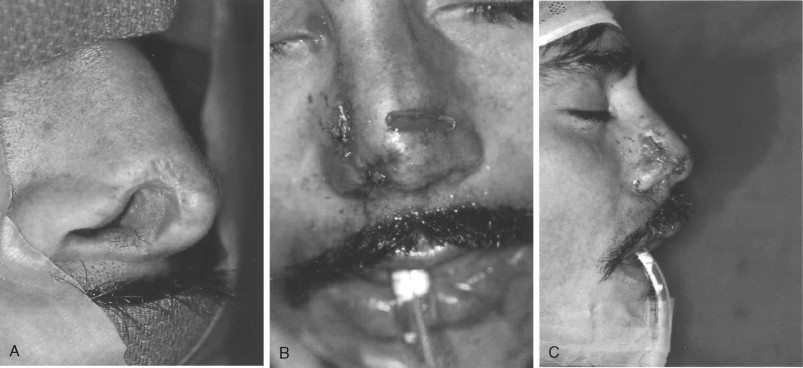
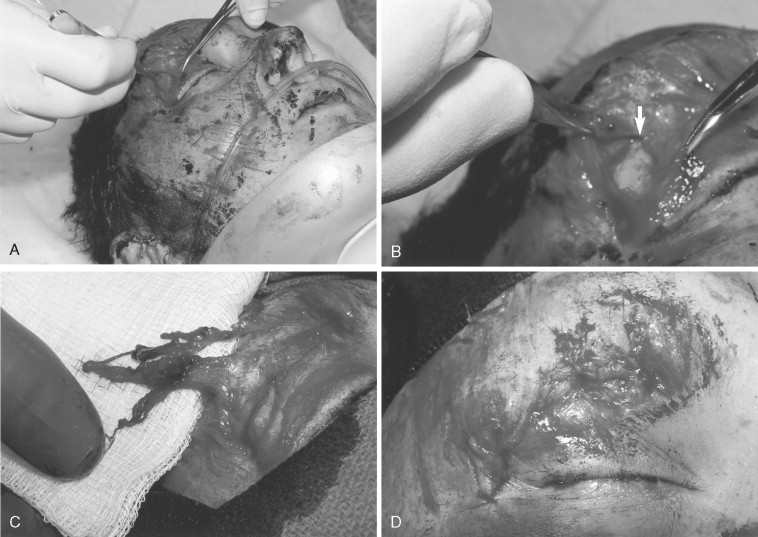
The most prominent feature on the face is the nose, therefore making it more prone to injury of both its hard and its soft tissue. A great deal of information has been written on nasal injury and repair with some emphasis on accomplishing definitive repair at the time of injury presentation to minimize later complications and deformities. The most important aspects of nasal injury repair include the control of epistaxis because patients can hemorrhage to death from nasal injury. This control can be in the form of intranasal packing coupled with low-pressure balloon catheters while using oxymetazoline as a vasoconstrictive agent rather than cocaine or phenylephrine; both cocaine and phenylephrine systemically raise the blood pressure and have had lethal side effects ( Figure 18-1 ). Airway maintenance is a priority with consideration given to utilizing airway adjuncts or intubation with packing ( Figure 18-2 ). The clinician must be suspicious for concomitant head and neck injuries, especially in children, and must also be aware of potential co-morbidities or ongoing pharmacologic therapies that may complicate or exacerbate the treatment process, such as anticoagulants (e.g., warfarin [Coumadin]) or antiplatelets (e.g., aspirin and clopidogrel [Plavix]).
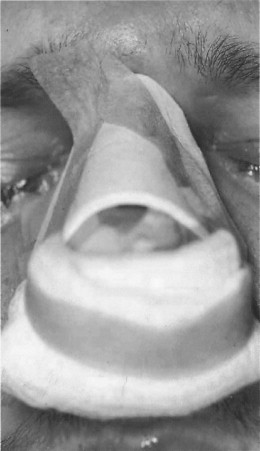

Most nasal injuries can often be treated in the emergency department with external splinting and internal nasal packing if necessary to support the mucosa, septum, and dorsum, such as seen in Figure 18-1 . However, if bone and cartilage are grossly disrupted they should be evaluated, reduced, and stabilized directly while the patient is sedated with a general anesthetic. Cartilage may be sutured directly to aid with reduction ( Figure 18-3 ). Every effort should be made to minimize long-term intranasal packing to reduce septic risk and to enhance patient airway comfort.
The nasal aperture and nasal tip soft tissue laceration will be most revealing in terms of scarring secondary to the thick, underlying dermis. The most important physiologic anatomy of the nose is the nasal aperture, which, with alterations in its size, can cause decreased nasal air flow and increased airway resistance, creating problems with breathing. Therefore repairs that return the nasal aperture to its original size and symmetry are paramount if at all possible ( Figure 18-4 ).
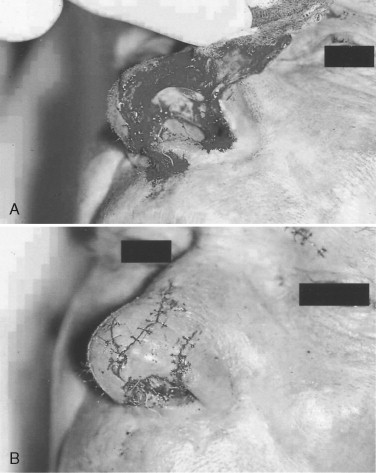
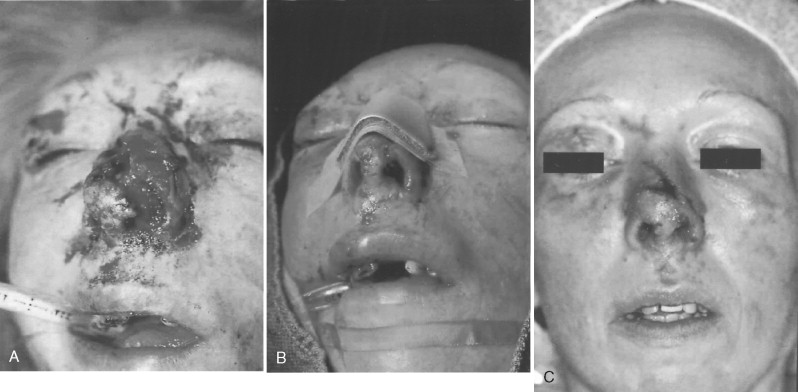
Avulsion type hard and soft tissue injuries need evaluation and treatment while the patient is sedated with a general anesthetic. Secondary reconstructive touch-up procedures should be anticipated ( Figure 18-5 ).

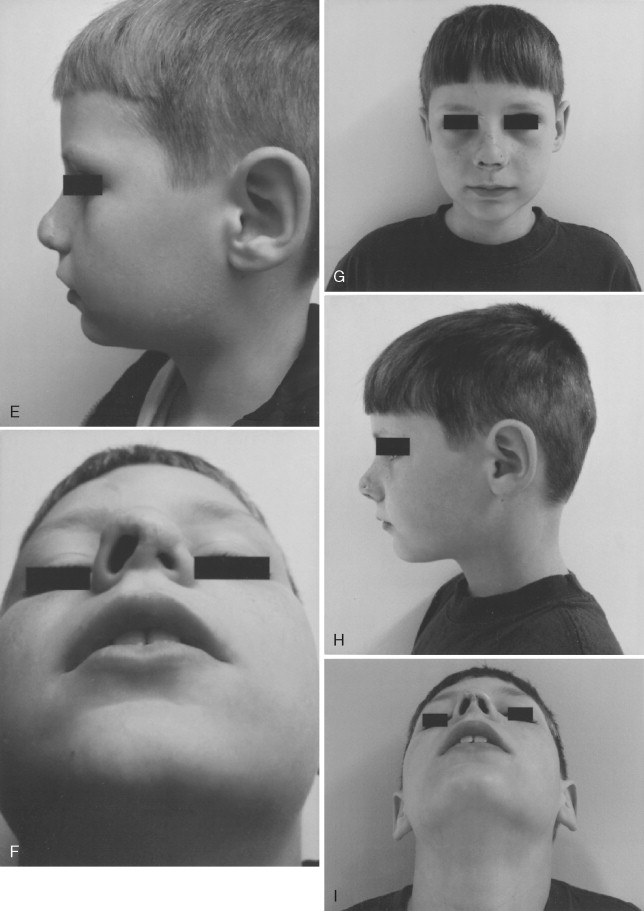
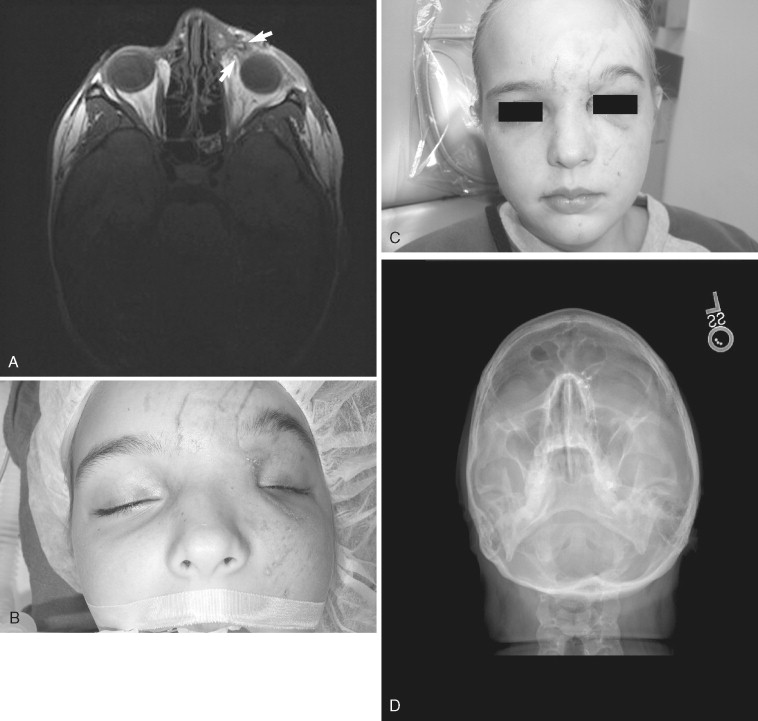
Because of bony remodeling and soft tissue scarring, clinicians should expect to reconstruct a small percentage of nasal injuries secondarily if the patient desires. The most common causes of this need for revision are patient noncompliance (such as sleep posture), the general cantilever-like instability of the nasal prominence itself, or the type and nature of the injury ( Figure 18-6 ). The clinician should remember to evaluate contiguous structure involvement such as medial canthal attachment, lacrimal sacs, outflow tracks, and sinus involvement, all of which are housed within the nasal compartment ( Figure 18-7 ). Turbinates, if necessary, can be partially or completely sacrificed.
Remember that the dorsum follows the septum and the nose is one-third bone to two-thirds soft tissue, especially in children. The septum, including both the quadrate cartilage anteriorly and the vomerine process more posteriorly, needs to be reduced or “snapped back” on top of the palatal crest. If buckling occurs, especially of the quadrate cartilage, then synechial adhesions may form between the septum and turbinates, decreasing nasal air flow and cross-sectional vault volume while increasing turbulence. If axial or random blood supply is greatly compromised, consider the use of adjunctive therapies early, such as hyperbaric oxygen therapy.
PERIORBITAL SOFT TISSUE INJURIES
Any periorbital soft tissue injury should raise the clinician’s awareness of possible occult injury to the globe or orbital content. Clinical and radiographic evaluation of this area is a priority. Pertinent points in evaluating and treating soft tissue injuries in the periorbital area include establishing visual acuity (not necessarily using the Rosenbaum pocket screener but discerning light and objects) and checking cardinal gazes if possible. In the obtunded patient it is important to identify an intact red reflex via funduscopic exam and to note any intraocular bleeding such as a hyphema. Hysterical blindness or those “professing blindness” versus true blindness can be ruled out by the following method: nonblind patients will reflexively follow their own likeness in a hand-held mirror.
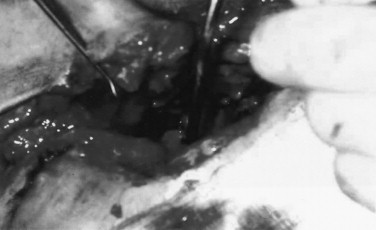
Corneal abrasions and foreign bodies are excruciatingly painful and patients will complain about them bitterly. Obtunded patients must be examined closely for these injuries unless lid edema or chemosis prevents examination. Shining an ophthalmologic light at 90 degrees to the corneal surface while viewing the cornea with another scope can often identify abrasions without using fluorescein dye ( Figure 18-8 ). Current therapies for corneal abrasions consist of treatment with nonsteroidals such as ketorolac ophthalmic solution (Acular) while patching and taping the eye closed for 24 hours. Biosalt solution (BSS) is a standard nontoxic, nonirritating irrigant for washing blood and foreign bodies from the fornices of the lids and corneoconjunctival surfaces.
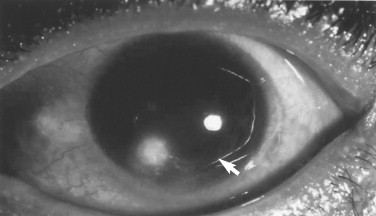
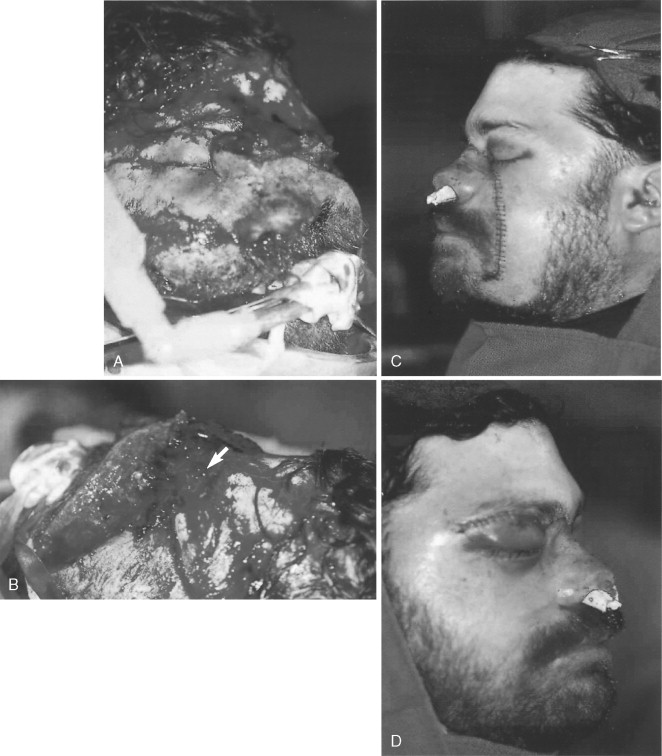
Lack of visual acuity, detached retinas (no red reflex), dislocated lenses, intraocular bleeds, and decompressed globes all need emergent ophthalmologic evaluation. If there is gross disruption of the globe and appropriate consultation indicates no hope of salvage, then enucleation is inevitable ( Figure 18-9 ). There is no rush to enucleate, however, as sympathetic ophthalmia is not as much a dreaded concern as once thought historically. A 10- to 14-day time frame is allowable to reach a decision on treatment. Steroid use is reasonable for stabilizing or treating occult injuries such as traumatic optic neuropathy (which occurs in a latent fashion from 3 to 5 days post injury) and for sympathetic ophthalmia. Traumatic optic neuropathy or retrobulbar hematoma may actually be emergently addressed by disrupting the lid margin; a lateral canthotomy or a margination of the bony orbital rim may be performed to salvage the site.
Treatment of eyelid lacerations begins by assessing what is present or absent, such as seen in Figure 18-9 . Through-and-through lacerations should be closed just like the mouth and lips—inside-out with care not to create an irritation source for the cornea with embedded sutures. Lacerated tarsal plates can be repaired directly. Avulsed levator attachment, as evidenced by lagophthalmia, may need reattachment to the superior tarsal rim in the upper eyelid, although tarsal trimming and superficial plication are common aesthetic procedures so this is not a great concern as once believed. Müller muscle function in elevating the superior tarsal plate can be evidenced by the phenylephrine test, which is not used extensively today. Superior lid contraction with corneal and scleral show is a much more serious problem than a ptotic lid, possibly creating ulceration of the cornea with potential loss of sight. When in doubt do not make heroic attempts to repair a levator sling because it is much more acceptable to repair secondarily any exaggerated ptosis ( Figure 18-10 ).
Some secondary reconstruction procedures, such as the Mustarde’s procedure or palpebral-based conjunctival transpositional flaps with or without partial tarsal plate transposition, are used in cases in which there is significant avulsion of the lid soft tissue and tarsal plates. One must be sure to completely release Müller’s muscle attachment on the posterior side of the tarsal plate transpositional flap before inserting it in the opposing lid defect to avoid retraction during graft healing. Mustarde’s procedure uses nasal septal cartilage with overlying mucosa similar to free buccal mucosal grafts for fornices reconstruction, combined with a lateral-based opposing lid skin flap or a non–hair-bearing postauricular full-thickness flap ( Figure 18-11 ).

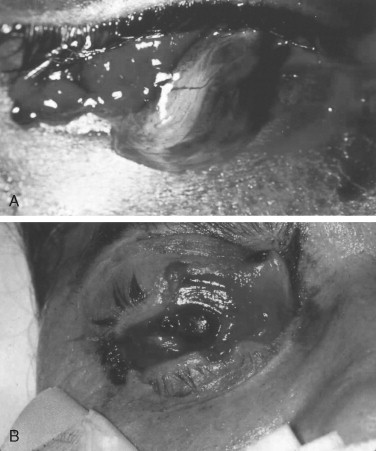
Through-and-through lid lacerations of the medial third of the lid margin often involve the canaliculus of the lacrimal apparatus or canthal attachments. Where identified, the canaliculi can be repaired by dilating the puncta and threading a polyethylene monocanalicular tube through the lumen, which then literally snaps into the punctal sphincter for retention ( Figure 18-12 ). These monocanalicular stents have outdated Crawford tubes in terms of ease of placement and retention. The clinician does not necessarily have to canulate all the way through the lacrimal sac and out the lacrimal duct unless the entire system has been disrupted. Only 2 to 3 cm of tubing is necessary to canulate the distal and proximal ends of the disrupted canaliculus into the lacrimal sac. There is often great difficulty in locating proximal and distal ends of the canaliculus in the laceration. Air can be introduced through the puncta while allowing water to pool in the laceration, so air bubbles can be seen coming out of the disturbance. This tube can be left in place 10 to 14 days to re-epithelialize and then removed under local anesthesia if necessary. Care should be taken not to take an inordinate length of time in locating canalicular ducts; in addition, absolutely do not sacrifice or delay repair of the lid for the sake of the canaliculus. Although the inferior canaliculus carries 80% of the lacrimal runoff, the superior canaliculus will accommodate in times of injury. Equally important is the knowledge that older individuals have decreased lacrimation and so repair of the inferior duct is even less important in these patients. Epiphora should be expected and will usually spontaneously resolve, but chronic epiphora may need a dacryocystorhinostomy to resolve it.

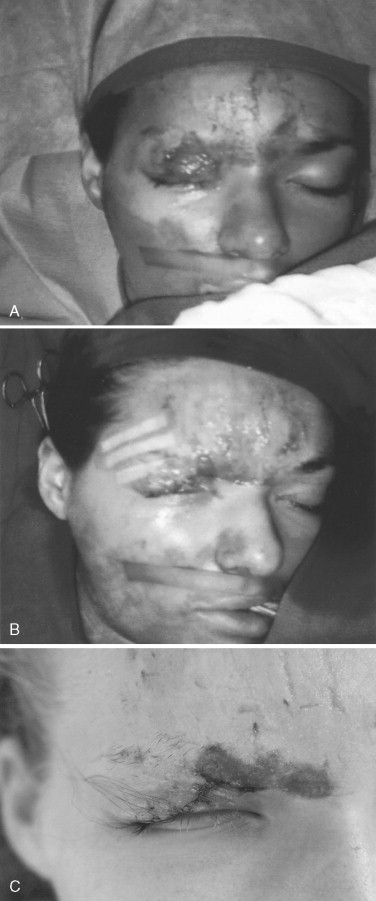
Repair of canthal tendon lacerations usually involves the superior or inferior limbs. Deep bites with a small ½-turn needle into the subcutaneous tissue at the lid margin using a colorless nonresorbing suture will usually suffice in repair without extreme measures such as exploratory incisions or laceration extensions. Delayed repair of canthal attachments is more appropriate than destroying other anatomic structures in distorted traumatic lacerations, such as seen in Figures 18-13 and 18-14 .
Avulsion or loss of one third of the tissue of a lid can be reconstructed by wide undermining of this loose tissue system, keeping in mind the amount of tissue often removed during cosmetic procedures such as canthopexy and blepharoplasty. Too much tension over the cornea following closure can cause irritation as well ( Figure 18-15 ). Lateral-based finger flaps, swung from one lid to the other, or full-thickness grafts from the postauricular non–hair-bearing area, or lateral preauricular advancement flaps (which are at high risk for cranial nerve VII injury) can be utilized. Procedures such as the lateral advancement preauricular flap are rarely used and are usually not that necessary in concert with long-term resolution and wound maturation. Herniating fat is often a blessing in preventing adhesions between the dermis and the orbital septal tissues, so it is best left alone with only skin closure over the fat. Loss of eyelashes and eyebrows is often treated with tattooing rather than complex small flaps or grafts with poor hair follicle orientation ( Figure 18-16 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


