Space Management in the Transitional Dentition
Development of the dentition is a long process that occurs in an orderly fashion under the control of genetic and environmental factors, from the primary dentition through the transitional stage to the permanent dentition, resulting in a functional, esthetic, and stable occlusion. During this long process, many local or systemic factors can influence development of the occlusal system, and any disturbances can prevent the progression to normal occlusion. General practitioners, pediatric dentists, and orthodontists have the highest responsibility to monitor this process carefully during developmental stages and to detect and manage disruptions of normal occlusal guidance.
Every tooth is maintained in its socket over the basal bone in a certain relationship to the dental arch, with adjacent and opposing teeth under a continuous balanced force resulting from the action of different environmental forces. If one of these forces is altered or removed, the relationships with adjacent teeth will change, causing drifting of teeth and initiating space problems. Early loss of primary teeth is one of the most common problems during the transitional stage of dentition, resulting in loss of space.
Fundamentals of Space Management
Before treatment planning and designing any appliance for space management, practitioners must understand the nature of the problem and the fundamental bases governing the biology and mechanism of occlusal development. The following are important processes to consider in this regard:
• Etiology of early primary tooth loss
• Effects of primary molar extraction on succedaneous teeth
• Incidence and nature of space closure
• Prediction of tooth emergence
• Factors influencing time of eruption
• Factors influencing mesial or distal drift
Etiology of early primary tooth loss
Local or systemic factors can cause early loss or early exfoliation of primary teeth:
• Extraction due to extensive caries
• Traumatic injury
• Early exfoliation due to abnormal root resorption (eg, ectopic eruption)
• Systemic disorders or hereditary syndromes, such as hypophosphatasia, rickets, acrodynia, leukemia, juvenile periodontitis, and Papillon-Lefèvre syndrome (see chapter 10)
Effects of primary molar extraction on succedaneous teeth
Fanning1 studied the lateral jaw radiographs of four boys and four girls who had undergone early and unilateral extraction of primary molars at different ages. The longitudinal study evaluated the tooth development and eruption of the antimere teeth, which were used as controls, and the rate of formation and the speed and time of eruption of the succedaneous teeth. No change was observed in the rate of root formation of the premolars after extraction; however, an immediate spurt occurred in the eruption of the premolar, regardless of its stage of development and the stage at which the primary molar was extracted. Premolar eruption was accelerated in the presence of longstanding necrosis of the primary tooth, especially if accompanied by loss of surrounding bone. Extraction of the primary tooth during active eruption of a developed premolar caused early clinical emergence of the premolar.
Early extraction of the primary tooth, before complete formation of the premolar crown (approximately 4 years of age), resulted in an initial surge, but then the tooth remained stationary and eruption was delayed. Therefore, the question arises whether it is possible to estimate individual eruption patterns by considering root development and skeletal development in addition to chronologic age. The effects of primary molar extraction on formation and eruption of their successors can be summarized as follows:
• The rate of formation of premolars does not change.
• An immediate surge in eruption occurs, regardless of the dentition stage and the patient’s age.
• Eruption is delayed if extraction occurs before half of the root formation is completed.
• Eruption is accelerated if extraction occurs when half of the root is developed.
Posen2 examined the complete records of 350 children at the ages of 4 and 5 years. Of these children, 62 patients, 34 girls and 28 boys, were selected who had undergone unilateral extraction of primary molars. The accumulated records included plaster casts and annual oblique cephalometric radiographs.
Posen2 concluded that eruption of premolars was delayed in these children. After the age of 5 years, a gradual decrease in delayed eruption of premolars was noted in these patients, and, at ages 8, 9, and 10 years, eruption of premolars greatly accelerated. This study confirmed delayed eruption of premolars and acceleration at ages 8 to 10 years after early extraction of primary molars.
Incidence and nature of space closure
Premature loss of primary teeth can cause functional disturbances and, because of the possibility of drifting of adjacent teeth, can result in space loss, difficulty in eruption of their successors, and, consequently, occlusal problems. Thus, premature loss of primary teeth needs careful attention during development of the dentition.
The consequences of premature extraction of primary teeth have been the subject of discussion for many years. In 1742, French physician Pierre Fauchard spoke of the inevitability and undesirability of removing primary teeth before their natural shedding.
The consequence of premature loss of primary teeth has been evaluated in several longitudinal and cross-sectional studies. In a review of previous studies, Owen3 revealed a large controversy in opinions on space management in the past. Some authors, such as Lundström,4 Linder-Aronson,5 and Seipel,6 believe that space maintainers are usually a waste of time and even are harmful 19% of the time. On the other hand, many researchers believe that premature loss of primary teeth usually results in space closure and causes harmful effects in the permanent dentition.3,7–10 Owen3 concluded that the following general trends are evident:
• The incidence of space closure increases with time. For all experiments, at least 96% of premature losses result in some closure within 12 months.
• The highest and earliest incidence of closure happens after premature loss of the maxillary primary second molar.
• Some mandibular extraction spaces show no closure.
• The rate of space closure is higher in the maxilla than in the mandible.
• Rates of closure in the mandible are more varied.
• The greatest amount of space closure in a given unit of time occurs at the maxillary primary second molars and then the mandibular primary second molars.
• There is complete agreement that space closure in the maxilla is predominantly caused by mesial movement of the teeth posterior to the extraction space. In the mandible, space closure is predominantly caused by distal movement of the teeth anterior to the space.
• There is evidence that the tooth mesial to the affected molar can drift distally into the space. Therefore, loss of space or arch length can occur from both directions.4
• Reports of space opening are only associated with late extraction.
The rates of the space lost after primary tooth loss differ. Northway et al10 stated that the space loss was greatest in the first 6 months and occurred in smaller amounts after that, with the least occurring 1 year after tooth loss.
Johnsen7 evaluated primary first molar loss in 10 white children during the mixed dentition stage (8 had bilateral and 2 unilateral premature primary first molar loss). At the initial visit, alginate impressions, photographs, and radiographs were taken. In all patients, the primary canine was present at the initial impression, and the primary second molars were present at the final impression. For six of the patients extraction was within 1 month of the initial casts; for one it was within 3 months; and for the remaining three it was more than 6 months after the casts were prepared.
Final measurements of the distances between the permanent first molars and permanent incisors were taken on the initial and final casts and compared. Spaces at the extraction site were measured from teeth immediately adjacent to the extraction site. Johnsen7 reported no significant mesial movement of the mandibular permanent molars after mandibular primary first molar loss but some space loss at the maxillary molars, especially if the permanent molars were erupting. Space loss in the mandible after premature loss of the primary first molar was the result of distal movement of the anterior teeth, especially in the presence of mandibular anterior crowding.
Northway et al10 digitized 107 dental casts from University of Montreal growth samples. Longitudinal data were collected annually from the age of 6 years, for an average observation period of 5.9 years. Trying to determine different aspects of early loss of primary teeth, Northway et al10 reported the following:
• Regarding dimensional loss due to caries or primary tooth loss (the first molar [D], the second molar [E], or both the first and second molars [D + E]), they found that in both sexes significantly greater amounts of space were lost in the mandible, with an average loss of 1.7 mm (ranging from 0.9 to 3.7 mm), than in the maxilla, with an average loss of 1.2 mm (ranging from 0.7 to 3.0 mm).
• The maxillary D loss group experienced a later increase in the amount of maxillary D + E loss.
• In both arches, the greatest loss of space occurred as a result of mesial molar movement; maxillary canine migration was significant only when the maxillary primary molars were lost as early as 9 years of age.
• In the mandible, maximum canine migration occurred after mandibular primary first molar loss.
• More space was lost in the first year following an extraction than in the successive years.
• In the maxilla, the rate of loss was age related (more space loss in younger children); in the mandible, the rate of loss was not age related.
• There was no significant difference in age for space opening during the emergence of the succedaneous teeth in the mandible; the opening occurred during second premolar eruption.
• Permanent molar mesial drift occurred in the maxilla after both E and D + E loss.
• Mesial movement of the mandibular permanent molar occurred only after E loss.
• Maxillary D loss affected maxillary canine relationships, while mandibular D + E loss affected mandibular canine relationships.
Prediction of tooth emergence
The timing of tooth eruption in orthodontic treatment is sometimes a decisive factor, whether in space management or extraction strategy. Unfortunately, individual variation in the age of eruption, especially in teeth emerging through the gingiva, is very high.
Grøn11 assessed tooth formation and emergence in 874 children (347 boys and 440 girls) by taking radiographs of the emerging tooth and its antimere as well as a left hand-wrist radiograph. Tooth formation was estimated by intraoral radiographs and rated in four stages of root length: one-quarter, one-half, three-quarters, and full root length (with open apex). Findings indicated that tooth emergence is more closely associated with the stage of root formation than chronologic age or skeletal age. The majority of teeth studied had three-quarters of the root complete at the time of clinical emergence; the mandibular central incisors and first molars had less root development, while the mandibular canines and second molars had just past three-quarters’ root development at emergence.
Hägg and Taranger12 studied tooth emergence in 212 randomly selected urban Swedish children who were followed from birth to 18 years of age. The study found that emergence of the primary teeth in boys is less than 1 month ahead of girls until the eruption of the primary second molars. Girls are consistently ahead of boys from eruption of the primary second molars to eruption of the permanent second molars (difference from 3 to 11 months).
Demirjian,13 studying a genetically homogenous French Canadian group of children 2.5 to 19 years of age, evaluated 5,437 panoramic radiographs and found no difference in the timing of dental development between boys and girls from 5 to 6 years of age. In contrast, among the older children girls were always more developed than boys.
Smith and Buschang14 examined growth of the mandibular canine and premolar roots in a mixed longitudinal sample of orthodontic patients (77 females and 74 males). They found that as a percentage of tooth length, roots grow with decreasing velocity between 7 and 14 years of age. More complex patterns appear for absolute growth in root length; for example, girls show an earlier maximum growth rate for the canine than for the premolars. Substitution of dental age for chronologic age reduces between-subject variation (assessed at age 11 years), especially for boys. A better understanding of dental maturation, including root length growth, should allow improved prediction models.
Factors influencing time of eruption
To summarize the literature, the following are some guidelines for predicting tooth emergence:
• Tooth emergence appears to be more closely associated with stage of root formation than chronologic age or skeletal age.
• There are variations between individuals.
• There is a much larger variation in the stage of root development at the time of clinical emergence than there is at the time of alveolar emergence.
• Sex differences in the timing of eruption are smallest for mandibular first molars and greatest for mandibular canines.
• The majority of teeth had attained three-quarters of their root length at clinical emergence and one-half at alveolar emergence.
• In normal tooth emergence, the root apices are always open and the root length is never less than one-quarter of normal size.
• Mandibular first molars and central incisors had one-half of their root developed at the time of emergence.
• Mandibular canines and second molars had more than three-quarters’ development of their roots.
• Emergence of the primary teeth in boys is around 1 month ahead of that in girls.
• In emergence of the permanent dentition, girls are ahead.
• There is a tendency for earlier tooth eruptions in the mandible.
• Usually there is no significant difference in age of eruption between the right and left sides of the mouth. (The right and left side difference in development is never more than one-quarter of the root). A variation in the emergence between the left and right sides can be considered normal if it persists for less than 6 months. Any asymmetric pattern of eruption that lasts for more than 6 months must be evaluated carefully.
• Most asymmetric eruption occurs in the premolar area.
Factors influencing mesial or distal drift
Principal factors that have the greatest influence on the rate and extent of mesial and distal drift of teeth are the degree of crowding in the dental arch, the type of primary tooth that is extracted, the type of occlusion, the age of the patient, the presence of abnormal oral musculature, the existence of abnormal oral habits, and the stage of dentition.
Degree of crowding
Degree of crowding in the dental arch is an important factor in space loss following premature loss of primary teeth.
Mandibular incisor crowding and extraction of the mandibular primary canine or primary first molar may cause a quick movement of adjacent teeth, such as midline shift or retraction of the incisors; increase overjet; and cause overeruption of mandibular incisors and impinging bite. On the contrary, in an uncrowded arch, there may be little or no movement of teeth following extraction. The author has observed no space loss in patients with a large mandible (mandibular prognathism). Much less space loss occurs in a primary dentition with interdental spacing (Baume class I) than in a primary dentition with no spacing (Baume class II).
Type of extracted tooth
Space loss and drift of adjacent teeth also depend on the type of primary tooth. For example, premature loss of the primary second molar, whether in the maxilla or mandible, causes mesial shift of the permanent first molar. Early loss of primary first molars can cause mesial drift of the posterior teeth and distal drift of the anterior teeth (in the mandible mostly distal and in the maxilla mostly mesial). Extraction of a primary canine allows permanent incisors to drift distally, but mesial drift of teeth is minimal.
Type of occlusion
Patients with deep bite have a greater tendency for space loss, especially in mandibular dentition, than do patients with open bite. Class II division 1 malocclusion usually becomes more severe after loss of mandibular primary teeth.
Permanent first molar occlusion has some influence on the rate of space loss. For example, maxillary and mandibular permanent first molars with good intercuspation have less tendency for mesial shift than do those with an end-to-end relationship.
Age of the patient
The age of the patient, or the dental age of the patient, plays a strong role in space loss following primary tooth extraction. The earlier a primary tooth is extracted, the greater the amount of drift. Research has shown that the highest rate of space loss happens in the first year after extraction, especially the first 6 months.15
If a primary molar is extracted before eruption of the permanent first molar, then the severity of mesial drift and space loss is much greater, even in arches that are not crowded.
Abnormal oral musculature
A strong mentalis muscle and high tongue position can damage occlusion after the loss of a mandibular primary molar or primary canine. In these conditions, collapse of the mandibular dental arch and distal drifting of the anterior segment will result.
Abnormal oral habits
Thumb or finger habits that exert abnormal forces on the dental arch, if accompanied by early loss of primary teeth, can aggravate arch collapse.
Stage of dentition
The stage of dentition and occlusal development can influence the rate and amount of space loss. In general, if the teeth near the space left by the premature loss of primary teeth are in an active stage of eruption, more space loss is likely to occur.
Planning for Space Management
Besides all of the aforementioned treatment planning considerations, such as the incidence and nature of space loss, prediction of tooth emergence, mesial and distal drift of adjacent teeth, and local and systemic factors, including type of occlusion, age of the patient, location of tooth loss, and time elapsed after extraction, the following specific points must be considered in order to determine the appropriate treatment plan, type of management, and type of device to be applied:
• Space availability (determined via space analysis)
• Amount of space loss
• Severity of the problem
• Nature of the problem
• Crowding or spacing in other areas of the arch
• Chronologic and dental ages of the patient
• Stage of occlusal development
• Presence or absence of a permanent successor
• Condition of the permanent successor and eruption potential (delayed or retarded eruption)
• Patient’s profile and any skeletal disharmony
• Relation of adjacent and opposing teeth
• Dental and periodontal conditions
• Time elapsed since loss of the primary tooth
• Status of permanent first molar eruption
• State of emergence and type of occlusion of the permanent first molar
• Position of the teeth and stage of eruption in the opposing arch
• Amount of overlying bone
• Sequence of eruption of the permanent teeth
• Presence of any abnormal muscle dysfunction
• Presence of any oral habits
• Patient’s occlusion and existing malocclusion
• Prognosis of the proposed management
Planning for any type of space management, like any other orthodontic treatment or tooth movement, requires a series of diagnostic procedures.
Diagnostic procedures
Diagnostic aids such as clinical evaluation, cast analysis, and radiograph and cephalometric evaluation enable the practitioner to reach proper decisions about space management that are linked to individual conditions and variations. After careful evaluation, the decision then will be made whether to maintain, regain, create, or eliminate space for each patient according to his or her dentoskeletal structural composite.
Diagnostic procedures, like any other treatments, require tools for data collection, analysis, and measurements. After the necessary diagnostic aids are collected, the first step in space management is recognition of the available space relative to the space needed for the permanent successor and occlusion.
Space evaluation and size prediction
The space available in the arch can be determined with space analysis. Space analysis is the evaluation of spacing or crowding within the dental arches, achieved through a comparison of the amount of space available and the amount of space required to align the teeth properly. In other words, the purpose of this type of analysis is a comparison of arch length to tooth material. Several types of analysis are available:
• Nance analysis16
• Moyers analysis9
• Tanaka and Johnston analysis17
• Staley and Kerber analysis18
• Merrifield analysis19
• Bolton analysis20
Nance analysis. In a comprehensive study, Nance16 concluded that the length of the dental arch from the mesial surface of one mandibular permanent first molar to the mesial surface of the opposite side is always shortened during the transition from the mixed to the permanent dentition.
Nance16 also reported an average leeway of 1.7 mm between the combined mesiodistal widths of the mandibular primary canine and the primary first and second molars and the mesiodistal widths of the corresponding permanent teeth in each side of the arch, with the primary teeth being larger. In the maxillary arch, the difference between the primary and corresponding permanent teeth is 0.9 mm per side.
Nance’s method16 compares a direct measurement from the periapical radiograph of unerupted teeth to available space. Available space is calculated by measuring arch length with a soft brass wire from the mesial surface of one permanent first molar to the mesial surface of the first molar on the other side. A sharp divider or a piece of 0.010-inch brass wire is used to measure the mesiodistal width of unerupted teeth on complete-mouth periapical radiographs (the tube is aimed directly toward the contact points). For accuracy and to assess for distortion in the film, the width measured on the radiograph is compared with the actual cast width.
Besides leeway space, two other dimensions are measured: the outside measurement, which is the perimeter of the arch from the mesiobuccal surface of one mandibular permanent first molar around to the mesiobuccal surface of the first molar of the opposite side, taken with a brass wire, and the inside measurement, which is taken with a divider from the mesiolingual surface of the mandibular permanent first molar on one side, at the point where the lingual tissues touch the crown of the tooth, to the gingival tissues between the mandibular central incisors on their lingual aspect. Nance16 indicated that the outside measurements do not increase from the time of the mixed dentition to the time when all permanent teeth are present but decrease during the transition; likewise, the inside measurement also decreases.
Moyers mixed dentition analysis. The mixed dentition analysis advocated by Moyers9 is a measurement taken from the four mandibular incisors to find the estimated size of maxillary and mandibular canines and premolars from probability tables that he calculated for girls and boys. The mandibular incisors were used because they would provide greater accuracy than maxillary lateral incisors, which have more variation in size.
The purpose of this analysis is to evaluate the amount of space available in the arch for succeeding permanent teeth and necessary occlusal adjustment. This method has some advantages: The analysis can be applied directly in the mouth as well as on casts on both arches; it is not time-consuming; and it requires no special equipment or radiographic projection.
Tanaka and Johnston analysis. The Tanaka and Johnston17 analysis is a variation of Moyers’s method9 except that the probability chart is not needed. In this technique, the total width of the four mandibular permanent incisors is measured and then divided by 2. The result plus 10.5 mm gives the estimated width of the mandibular permanent canine and premolars and the result plus 11.0 gives the estimated width of the maxillary canine and premolars. According to Dean et al,8 the estimated width, in millimeters, of unerupted canines and premolars measured with the Tanaka and Johnston method17 corresponded to the 75% level of probability in Moyers’s prediction table.9
For example, if the width of the mandibular incisors is 23.0 mm, one would divide by 2 and add 10.5 mm for the mandibular arch. The result is 22.0 mm, compared with 22.2 mm obtained from Moyers’s table. The corresponding values for the maxillary arch are 22.5 mm for the Johnston and Tanaka analysis and 22.6 from Moyers’s table. The Tanaka and Johnston analysis provides significant clinical acceptability with a minimal amount of time and effort.
Staley and Kerber analysis. Staley and Kerber18 introduced a combination method of space analysis in which the size of permanent incisors is measured directly on the dental casts and the size of unerupted premolars is measured on radiographs to predict the mesiodistal width of unerupted canines, which cannot be accurately measured on a radiograph.
Merrifield analysis. Merrifield’s “total space analysis” is based on craniofacial analysis and Tweed’s triangle together with total dentition analysis.19 In this analysis, the dentition is divided into three areas: anterior, midarch, and posterior. This division is made for two reasons: (1) simplicity in identifying the area of deficient or surplus space and (2) the possibility of arriving at a more accurate diagnosis, according to the mandibular incisor position and inclination and the patient’s skeletal pattern.
Bolton analysis. The Bolton20 analysis is another kind of cast analysis used for a comparative evaluation of the mesiodistal widths of the maxillary and mandibular dentition. The greatest mesiodistal dimension of all teeth (except second and third molars) is measured on each cast. The ratio of the 12 mandibular measurements to the 12 maxillary measurements (sum of mandibular 12 divided by sum of maxillary 12, multiplied by 100) is considered the overall ratio. The ratio of the 6 mandibular anterior measurements to the 6 maxillary anterior measurements (sum of mandibular 6 divided by sum of maxillary 6, multiplied by 100) is the anterior ratio. Bolton20 reported that the mean overall ratio is 91.3 (± 1.91). The mean anterior ratio is 77.2 (± 1.65).
This analysis addresses discrepancies in tooth mass between the maxillary and mandibular arches. Proportional sizes of the dentition are a prerequisite for good occlusion; for example, if teeth are large in one arch and normal or small in the opposing arch, some irregularity in occlusion will occur, and there is no way to achieve an ideal occlusion.
Another example of disproportion is when large maxillary incisors combined with normal mandibular incisors result in increased overjet. Large mandibular incisors and normal maxillary incisors cause mandibular incisor crowding (Fig 4-1). Thus, these discrepancies deserve attention before treatment planning.
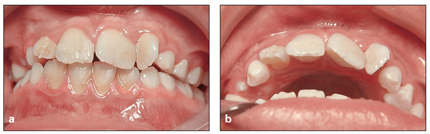
Fig 4-1 (a and b) Bolton discrepancy (oversized maxillary incisors).
Other considerations determining space adequacy
Space management is a general strategy of different procedures applied during the primary or mixed dentition to prevent or intercept problems of occlusal development. The purpose of all mixed dentition analysis is to estimate as accurately as possible the amount of space required for permanent canines and premolars before eruption. Careful evaluation is an important step in achieving proper space management during the primary or mixed dentition.
Regardless of the method used in arch length analysis, which is a linear comparison of arch length and tooth size, the following factors also must be considered:
• Inclination of the mandibular incisors
• Patient’s profile
• Patient’s growth pattern
• Incisor shape and degree of crowding
• Curve of Spee
• Interdental spacing
• General eruption patterns and problems of eruption
• Amount of leeway space
Inclination of mandibular incisors. The anteroposterior position of incisors can affect decisions about space management. If incisors are crowded and already proclined, the space requirement would be greater than the analysis measurement indicates. If the mandibular incisors are retruded because of muscular dysfunction or habits, there is a possibility of bringing the incisors to a more normal inclination and gaining some space. This also must be considered in space calculation.
Nance16 asserted that overprotruding incisors to gain space is a big mistake; he claimed that “it is a suicide” because it is not stable, it damages alveolar bone support, and it disturbs the patient’s profile. Treatment planning for any type of space creation must be based on the position and inclination of incisors and the patient’s profile.
Patient’s profile. The patient’s profile and lip position are another important consideration in space analysis. A lip that is procumbent relative to the chin and nose may require incisor retraction, which needs more space. Likewise, correction of incisor crowding while the profile is convex and the lips are procumbent requires more space than the analysis indicates, and the possibility of extraction would change the results of space measurement.
Patient’s growth pattern. The patient’s growth pattern is another important factor to be considered. As Björk and Skieller21 stated, in a child with a well-proportioned face there is little or no tendency for the dentition to be displaced during growth, while in a child with jaw discrepancy the teeth often shift anteriorly or posteriorly. Space analysis would be less accurate in children with problems such as Class II or III malocclusion, long face, or short face).
In addition, the growth pattern informs whether distalization of posterior segments is possible for space regaining or space creation. Distalization can be very critical in vertical growth and advantageous in deep bite conditions.
Incisor shape and degree of crowding. During evaluation of anterior crowding and measurement of the amount of crowding, the amount of incisor overlap must be carefully determined. Generally every overlapped contact will require 1 mm or more of space for correction. Incisors with wide edges have a higher tendency for overlap and more need for stripping and the result is more stable.
Curve of Spee. According to Andrews,22 the ideal occlusion will have a nearly flat curve; correcting the curve of Spee and bringing the curve to a flat or nearly flat level requires some space, which must also be considered in space analysis.
Study casts are a useful tool in the measurement of the curve of Spee, which can be measured, in millimeters, from the deepest part of the curve to the occlusal plane, which is a straight horizontal plane resting from the tip of the most distobuccal cusp of the last molar to the tip of mandibular canine of the mandibular arch. Correcting the curve of Spee also requires some extra space that must be considered in space analysis.
It has been generally believed that, for each 1 mm of curve, 1 mm of space is required for correction on each side of the arch.
Interdental spacing. The presence of any interdental spacing in the arch must be carefully measured and considered to ensure accuracy of the overall space analysis.
General eruption pattern and problems of eruption. The presence of any obstacle disturbing the eruption process must be considered in management planning. This includes hypodontia and hyperdontia, abnormal sequence of eruption, retarded eruption, abnormal root development, resorption, infection, ankylosis, or any pathologic lesions.
All of these problems can change final decisions about space management, and careful radiographic evaluation of eruption patterns is essential.
Amount of leeway space. Many investigators, including Nance,16 Moorrees and Chadha,23 and Ricketts,24–26 have shown that leeway space and arch circumferences decrease during the transitional dentition as the molars shift mesially. Arch length also decreases through the proximal wear of molars and premolars; Moorrees and Chadha23 reported that the average arch length of an individual is smaller at 18 years of age than at 3 years of age.
Considering these events, the presence of good leeway space is another important point to be considered in space analysis. Moderate space deficiency of the incisors during the mixed dentition can be solved in some situations in the presence of a good amount of leeway space (see space supervision in the following section).
The best tools for accurate evaluation of all the aforementioned points and completion of accurate space analysis are the clinical evaluation, study casts, radiographic examination, and cephalometric analysis.
Treatment Options for Space Management
After careful space analysis and evaluation of the important points mentioned, and depending on the specific conditions of the patient’s problem, the following five options may be considered for space management:
1. Space maintenance
2. Space regaining
3. Space creation
4. Space closure
5. Space supervision
Space Maintenance
Space maintenance is a procedure performed in the primary and mixed dentitions to preserve the available space before any closures occur in the arch length. The use of a space maintainer appliance or restoration of a proximal caries lesion in the primary dentition at the right time can obviate the consequences of loss of arch length and the need for complex orthodontic treatment at a later stage.
Appropriate space maintenance usually is a process to maintain a space when adequate space is available and all unerupted teeth are present and at the proper stage of development. There are also other situations when maintaining the space is indicated even without the presence of a successor.
Indications
• When the available space is sufficient for the permanent successor and there is more than 6 months’ time before the permanent successor erupts, space maintenance is recommended.
• When the permanent successor is missing but the patient has a perfect occlusion, space must be maintained to prevent occlusal disturbances and allow for a future implant or fixed partial denture.
• When hypodontia in one arch causes constriction and arch length deficiency and there is crossbite, space must be maintained to preserve arch length for a better arch relationship; an example is when there is a missing maxillary lateral incisor and maxillary deficiency.
• If the space has already decreased some and is not sufficient for the succedaneous tooth but overall arch evaluation indicates adequate arch length, there is no need for space regaining; space maintenance is sufficient.
Prevention of space loss during the primary or mixed dentition is not limited to premature loss of primary teeth; there are other situations that need early intervention, such as the presence of proximal caries and primary molar ankylosis. Early maintenance is necessary to preserve space for the interproximal contact until proper restoration. Ankylosis of primary teeth, especially when they are below the level of occlusion, can result in tipping of adjacent teeth and space loss as well as overeruption of the opposing tooth. These problems are more destructive when the ankylosed tooth is submerged.
Contraindications
There are situations when space maintenance is not the proper management and other options such as space regaining, space creation, space closure, or other choices must be applied. Examples of these situations include the following:
• When the space is not sufficient for the permanent successor
• When the space is sufficient but the space analysis indicates an overall arch length deficiency and comprehensive orthodontic treatment and extraction is required
• When no permanent successor is present but overall space analysis in the arch indicates a need for space closure
• When the primary dentition is widely spaced
• When space loss is not predicted
• When the succeeding tooth is expected to erupt in less than 6 months
• When the opposing molars are locked into a desirable and stable relationship
Failure to maintain space
Early loss of primary teeth can cause many different problems for the dentition. Two cases can best explain this principle (Figs 4-2 and 4-3). Both patients were at almost the same stage of dentition and similar occlusion, and each had lost one of the maxillary primary lateral incisors. The child shown in Fig 4-2 had lost the maxillary right primary lateral incisor, and the child shown in Fig 4-3
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


