Examination, Early Detection, and Treatment Planning
In the past, orthodontics was focused mainly on juvenile and adult treatment. Some types of early intervention procedures, such as orthopedic treatment, were not as well known and accessible as they are today. The major focus was limited to aligning irregularities after complete development of malocclusions.
Regardless of whether therapy involves the early-age or the traditional orthodontic approach, sometimes more emphasis is placed on the mechanisms of treatment than on the important element of diagnosis. Every day, new orthodontic products come to the market, and orthodontic residents and new orthodontists are influenced by the manufacturer’s advertising.With so much emphasis on knowledge of bands, brackets, archwire configurations, and “systems,” practitioners sometimes get the mistaken impression that orthodontic care is primarily a mechanical procedure.
Early orthodontic treatment is now more generally accepted as a means of gaining the greatest possible control over form and function and changes that happen with time. The main objectives of early orthodontic treatment are to detect problems at early stages of development, to eliminate or control the disturbing effects of these factors, and to intervene at the proper time. To achieve these objectives as well as efficient treatment and excellent results, a thorough diagnosis and sophisticated treatment plan are required.
Treatment planning is strategy, the treatment itself is the tactic, and all of these processes must be organized on a sequential basis. In other words, the clinician must follow this systematic procedure:
1. Examine the patient
2. Diagnose the problem
3. Classify the problems
4. Plan the treatment
5. Treat the patient
Diagnosis is the most critical part of orthodontic treatment. The goal of the diagnostic process is to prepare a comprehensive list of the patient’s problems in order to synthesize the various treatment options into a rational treatment plan for the best outcome.
A comprehensive orthodontic diagnosis does not merely focus on the relationships of the maxillary and mandibular dentition. It requires a thorough evaluation of the patient’s general health and occlusal situation and a consideration of the relationship of the dentition to the basal bone, other skeletal components, and the neuromuscular and soft tissue environments.
All treatment planning must be based on the elimination or control of etiologic factors and use of the patient’s growth potential to guide occlusion toward normality, especially in early orthodontic treatment.
Diagnostic procedures must follow a series of organized and sequential steps (Fig 3-1). The first step toward a thorough and accurate diagnosis in orthodontic treatment is the creation of an accurate and adequate diagnostic database. This is necessary for assessment and recognition of dentoskeletal anomalies. The second step is the design of a treatment plan, based on accurate findings, that both addresses the present situation and allows for future changes in dentition and jaw growth that will take place during the early treatment.
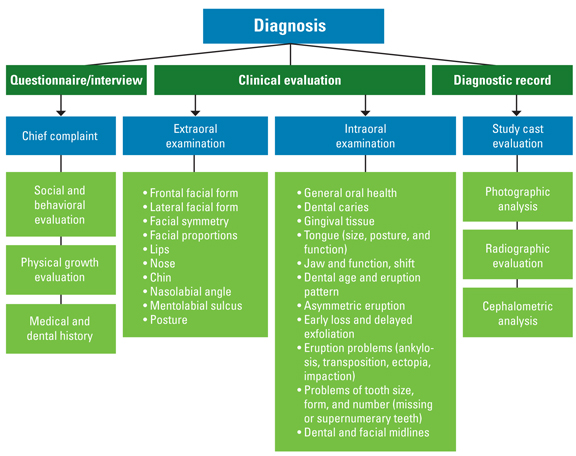
Fig 3-1 Elements of a complete diagnostic database.
Orthodontic problems almost always result from improper developmental processes that take place during development of the occlusal system; they are not the result of a pathologic process. It is often difficult to be certain of etiologic factors, but it is important to establish and rule out the causes of malocclusion. The etiology of malocclusion and the relative contributions of genes and environment have been a matter of controversy over the past century (see chapter 1). Studies in more recent decades indicate that during embryonic life, genetic mechanisms have more influence on the morphogenesis of craniofacial structure. The development of occlusion, in contrast, seems to be influenced strongly by the environment, especially during the early postnatal period.1
For orthodontic purposes, all diagnostic databases, whether clinical or paraclinical, are derived from three major sources: (1) the questionnaire and interview, (2) the clinical evaluation, and (3) the paraclinical evaluation (diagnostic record).
Questionnaire and Interview
The interview is an important appointment for the patient and the provider. The main purpose is to evaluate the patient’s and parents’ desires and their social and behavioral statuses. Many orthodontic practices use questionnaires, which can be completed by nurses or orthodontists.
This type of form can be filled out by patients or parents in advance to determine the patient’s wishes, expectations, and goals for orthodontic treatment.
The questionnaire can be broken down into four sections: (1) patient’s chief complaint, (2) social and behavioral evaluation, (3) physical growth evaluation, and (4) medical and dental history.
Patient’s chief complaint
The first step of the interview is to find out the patient’s chief compliant and expectations from treatment. The best way to ascertain this information is for the orthodontist to directly question the parent or patient, especially if facial esthetics is a concern. Some example questions include:
• What brought you here?
• What changes are you expecting to achieve?
• What is your chief complaint?
The provider may or may not agree with the patient’s wishes; this judgment must be explained after the record is completed, when the clinician explains the problem and offers the best treatment options. The main purpose at this stage is to determine the patient’s exact goal, whether it is entirely esthetic or a health concern. Confirming this information makes the practitioner aware of the patient’s or parents’ knowledge and understanding of the situation. In addition, it makes it easier for the provider to explain the problem, the treatment options, treatment limitations, and the dependability of the results. The results of some early-age treatments are dependent on the patient’s cooperation and the parents’ care. Reasons for early intervention and the possibility of a second phase of treatment must be clearly explained.
Social and behavioral evaluation
The social and behavioral histories are another important part of the first interview. Although these factors are important for treatment success, some parents may be reluctant to speak of their child’s emotional or behavioral problems. In these situations, the practitioner must cautiously explain that treatment success depends on patient compliance.
For this reason, questioning about school progress or the patient’s attitude with friends or siblings could be helpful. Recognition of the patient’s emotional or learning disabilities will help to modify the treatment approach according to the patient’s ability. Treatment can be designed in such a way to reduce the responsibility and cooperation needed from the patient in the use of some orthodontic devices such as headgear or removable appliances.
Pretreatment evaluation of the social and behavioral statuses of the patient is also important for understanding the patient’s expectations, particularly for adult patients. Sometimes, after minor interceptive treatment, the patient or parents may expect a great change in facial appearance before full eruption of the permanent dentition. It is the practitioner’s responsibility to explain the limitations and the possible final results of treatment.
Physical growth evaluation
The general physical growth of the child is another important element to assess in the general evaluation for any type of early orthodontic treatment. The growth status of a child is an important part of treatment planning; this includes the amount of growth that can occur during treatment and the potential for growth that remains after treatment. The best growth modification strategy is achieved during the growth spurt of children.
The growth status of children can be explored by asking questions such as:
• How rapidly has the child grown recently?
• Has there been a change of clothing size?
• Are there signs of sexual maturation?
While these questions can be helpful in estimating the child’s current growth status, other more accurate techniques are available for evaluation of the growth potential, including evaluation of hand-wrist radiographs, neck vertebrae, and cephalometric radiographs.
Medical and dental history
The main purpose of seeking the medical and dental history of the orthodontic patients is to establish the causes of malocclusion, if possible. Although it is sometimes difficult to be certain of etiologic processes, it is still important to conduct a thorough examination and prepare good records. This will clarify problems and allow the best treatment planning. The orthodontist must base the design of the treatment strategy on the nature of the problem and the findings obtained from recorded data.
The patient’s medical history consists of two parts, the family’s history and the patient’s history.
Family’s medical history
The most important points in the evaluation of family medical history are:
• Genetic background
• General health of the parents and siblings
• Facial and dental resemblances between the parents and the patient
• History of orthodontic treatment for the parents or siblings
• Dental health of the parents
• Condition of the mother during pregnancy (diseases, medications, accidents) as well as length of term and type of delivery
The family and genetic history can be evaluated by finding resemblances between the facial characteristics and dental occlusions of the parents and the patient. Previous orthodontic treatment of family members and the nature of these issues should also be considered.
The parents’ general and dental health is a good indicator of the patient’s susceptibility to periodontal disease and caries. The mother’s general health during pregnancy can have a direct effect on the patient’s health and dental occlusion. Some medications or diseases (eg, viral infections and endocrine disease) and accidents during pregnancy are examples of history items that should be assessed. Reports indicate that length of term and premature birth can also affect development of occlusion by disturbing normal jaw growth or dental structures.2,3 The use of forceps in difficult deliveries can affect the temporomandibular joint (TMJ), and long-term effects could detrimentally influence growth and development of the jaws.4
Patient’s medical history
As discussed in chapter 2, the exact contribution of genetic and environmental factors associated with specific types of malocclusion is not always easy to verify. Therefore, the orthodontist or assistant must ask several important questions to aid assessment.
When the patient’s health is evaluated prior to treatment, it is important to note whether the patient has previously taken or is currently taking any long-term medication and for what purpose. This information can help to determine if the patient has any systemic or metabolic disease that may contraindicate orthodontic treatment or postpone the time of treatment. For example, orthodontic treatment for children with diabetes, even under medical control, requires special and careful monitoring, because these individuals are susceptible to periodontal breakdown following application of orthodontic forces. In children with mitral valve prolapse or heart problems caused by rheumatic fever, premedication and antibiotic prophylaxis might be required prior to invasive procedures such as banding.
Another area to assess when gathering the patient’s history is any previous occurrences of accidents or trauma to the dentition, jaws, and joints. Early fractures of the condylar neck should not be overlooked, because they can cause significant developmental defects at older ages. For example, childhood condylar jaw fracture is the most likely cause of asymmetric mandibular deficiency in children.5,6
Other destructive processes in the TMJ that can cause mandibular problems include rheumatoid arthritis and congenital absence of tissue, as is seen in patients with hemifacial microsomia.
Considering the phenomenon of “form related to function” and the possibility that one might affect the other, any imbalance in muscle function and any disturbed physiologic functions such as respiration, deglutition, mastication, and speech must be carefully evaluated. Assessment of a previous or present history of mouth breathing in growing children is important. This condition can have profound effects, including enlarged tonsils or adenoids, oronasal obstruction, and allergies.
Eliciting information regarding allergies is also important because many patients are allergic to clinical and orthodontic materials such as latex or have sensitivity to nickel, which can be a component of wires and brackets.
Any history of blood transfusions must be considered because of the risk of immunodeficiency after exposure to viruses such as hepatitis and human immunodeficiency virus (HIV).
The important areas to ask about prior to orthodontic treatment can be summarized as follows:
• History of long-term medication use
• Last visit to a physician and dentist
• Hospitalizations: when and why
• Allergies, especially latex or nickel sensitivity
• History of blood transfusion (to assess the chance of hepatitis or HIV infection)
• Heart problems, such as mitral valve prolapse or problems associated with rheumatic fever (to assess need for antibiotic prophylaxis)
• Accidents or any traumatic injuries to the teeth or jaws (the effects of previous trauma to teeth and apical involvement without any clinical signs may be intensified by orthodontic force and tooth movement)
Clinical Examinations
The orthodontic clinical examination is a thorough evaluation of orofacial structure, both in stasis and in function. The health of oral and perioral hard and soft tissue structures must be carefully assessed before any orthodontic treatment. Pathologic problems such as dental caries, periodontal disease, inadequate attached gingiva, and apical involvement must be treated first. After the problem is under control, bonding and tooth movement can be started.
Clinical examinations involve a series of tests that can be performed by visual observation, digital inspection, and functional analysis of all of the extraoral and intraoral structures. It is important not to concentrate so closely on one aspect of the patient’s overall condition that other significant problems are overlooked.
Extraoral Examination
The extraoral clinical examination includes evaluation of facial esthetics and morphology, including structures, proportion, typing, and symmetry. The facial form, in both the frontal and lateral views, is now a major determinant of orthodontic diagnosis and treatment planning. Facial and dental appearances are of major concern to almost all patients seeking orthodontic treatment. Evaluation of esthetics is an important part of the clinical examination. Graber and Vanarsdall7 pointed out that malocclusion is a disability with a potential to affect physical and mental health, not a disease, and that appropriate treatment can improve the well-being of the patient.
Assessment of dentoskeletal hard tissue relationships alone without a thorough knowledge of the condition and changes of soft tissue that take place during growth and orthodontic treatment is entirely inadequate. Facial esthetics is an extremely complex issue that must be carefully assessed in the extraoral examination.
Gugino and Dus8 stated that the human face as a whole is anatomically and functionally one of the most complex regions of the human body. A sound understanding of embryology and physiology of the occlusal system and the stomatognathic system is required to understand and recognize the problem of malocclusion in order to provide the best orthodontic treatment for each patient’s occlusion.
Many factors, including eyes, hair, skin, lips, teeth, nose, chin, and jaws, play an important role in the composition of an esthetic face. These components impact our perception of the face and must be carefully evaluated during diagnosis and treatment planning for orthodontic treatment.
Esthetic evaluation of the patient’s frontal and lateral appearances and detection of any deformity before treatment, prediction of future growth changes in early orthodontic treatment, and design of a treatment plan that takes these elements into consideration are majors goal of the extraoral examination.
Esthetic evaluation of the patient’s frontal and lateral appearances deserves special attention, especially in early-age orthodontic treatment. This evaluation is important at the time of examination, and all potential growth changes during and after treatment must be considered.
The extraoral examination should include assessment of the following important features (see Fig 3-1):
• Vertical and transverse frontal facial morphology (dolichocephalic, mesocephalic, or brachycephalic)
• Facial profile (straight, convex, or concave), to identify any adverse sagittal (anteroposterior) growth patterns and occlusal disharmonies
• Facial proportions, that is, the upper and lower facial dimensions, to identify any adverse vertical growth patterns
• Upper lip–lower lip height ratio
• Facial symmetry, to identify any adverse transverse growth patterns including asymmetries of maxillary and mandibular bones
• Development, tonicity, and form of facial muscles and soft tissue
• Nose size and proportion and symmetry to the rest of the facial structures
• Chin size, shape, symmetry, and position related to other facial structures
• Lip size, tonicity, and position related to profile and incisors, at rest and in function
• Nasolabial angle
• Mentolabial sulcus
• Patient’s posture
Frontal facial evaluation
At the beginning of a systematic facial examination, the child should be seated in an upright position with the practitioner at a distance looking straight at the child’s face. Evaluation of the patient’s frontal view allows the examiner to identify the patient’s facial form, facial symmetry, and proportion between different parts of the face.
Other factors must be considered in treatment planning besides cephalometric measurements. Lines, angles, and numbers cannot be the only diagnostic tools used. The things an observer’s eyes reveal about the patient’s facial characteristics in three dimensions, both in stasis and in function, are also very important to consider. These elements include facial typing, facial symmetry, and facial proportion.
Facial typing
When the face is viewed from the front, the facial form can be identified as long, wide, or medium. According to En-low’s classification,9 these three types of facial pattern are termed dolichocephalic (long face), brachycephalic (broad face), and mesocephalic (medium face), respectively. According to Enlow,4 the facial complex attaches to the cranial base, which dictates the dimension, angle, and topographic characteristics of the face.
The dolichocephalic head shape yields a narrow, long, and protrusive face and a mostly convex profile. Patients with Class II malocclusions with a tendency toward a vertical pattern show this type of facial pattern. The brachycephalic head shape yields a broad, less protrusive, straight profile, a short face, and a tendency toward a horizontal growth pattern. Class II division 2 malocclusions are usually associated with this type of facial pattern. The mesocephalic head shape is an intermediate head form with intermediate facial features. Usually patients with normal or Class I occlusions show this type of configuration. Different head forms are more prominent in different geographic regions. The type of facial morphology, especially in growing patients, can have some impact on growth prediction, and these considerations may impact treatment tactics such as expansion.
Facial symmetry
Facial symmetry in the frontal and lateral views is another important aspect to evaluate because this will reveal asymmetric growth patterns of the maxilla and mandible and/or lateral deviations of the mandible. All faces show a minor degree of asymmetry, but marked asymmetry is not normal and needs careful evaluation, especially in young children.
Facial symmetry can be assessed by viewing the face from the frontal view or while the patient is reclined in the dental chair and the practitioner is seated behind the chair. A piece of dental floss can be stretched from the middle of the bridge of the nose, down the nose and lower face, to the midpoint of the chin to establish the facial midline. Next, facial symmetry can be judged by comparing the left and right sides of the face from the facial midline plane (Fig 3-2).

Fig 3-2 Evaluation of facial symmetry. A—facial midline; B—bipu-pillary line; C—lip line.
This evaluation must be performed with the patient both at rest and at maximal intercuspation or centric occlusion to clarify if the asymmetry is due to mandibular shift and chin deviation or to structural asymmetry (Fig 3-3). Facial asymmetry can be the result of many morphologic abnormalities of different parts of the dentoskeletal structures in congenital misconfiguration.

Fig 3-3 Asymmetric growth of the mandible (right condylar hyperplasia) in a 16-year-old girl.
As Subtelny indicated,10 except in cases of congenital deformity, the maxillary bone is a fixed, stable bone, and the midpalatal suture (raphe) is the true midline indicator of the maxilla. The maxillary midline, except in cases where the maxillary dental midline has shifted because of local factors, coincides with the facial midline and can be a good point of reference in evaluation of facial symmetry.
The causes and the morphologic configurations of facial asymmetry can be determined through the use of diagnostic aids such as posteroanterior cephalometric and lateral jaw radiographs, examination of the dental occlusion on the left and right sides, and observation of occlusal level (curve of Wilson). Patients with significant skeletal asymmetry (those patients with asymmetry not resulting from only a functional shift of the mandible) always fall into the severe problem category.
Early detection of any asymmetry, especially in young children, could be very important for early intervention. The timing of intervention and the treatment plan depend on the cause of the problem, the type of asymmetric mandibular growth, and whether the asymmetry is caused by deficient or excessive growth of the condyle.
Analysis of facial symmetry is discussed further in the section on frontal photography.
Facial proportion
Evaluation of facial proportion is another important aspect of the clinical and paraclinical evaluation. When the anterior facial proportion is evaluated in the vertical dimension, three segments of the face can be assessed: (1) from forehead hair line to glabella, (2) from glabella to subnasale, and (3) from subnasale to soft tissue menton. In a normal, balanced ratio, these three segments are equal (Fig 3-4).

Fig 3-4 Frontal evaluation of facial proportions. In a balanced ratio, the segments from forehead hairline to glabella (A), from glabella to subna-sale (B), and from subnasale to soft tissue menton (C) are equal.
The upper lip–lower lip height ratio is another frontal evaluation of facial proportion. The area from subnasale to stomion should be approximately one third of the total lower third of the face (subnasale to menton)11 (Fig 3-5).

Fig 3-5 Upper lip–lower lip height ratio. The area from subnasale to stomi-on should be approximately one-third of the total lower third of the face.
Another frontal evaluation that can be considered is the sagittal facial proportion, proposed by Sarver,12 also called the rule of fifths. This method is discussed in more detail in the section on facial photography.
There are other important points to be evaluated in both the facial frontal and lateral views, including facial form, symmetry, nose, and chin and lip relationship in three spatial planes: the sagittal, vertical, and transverse dimensions.
Lateral (sagittal) facial evaluation
During the systematic lateral facial examination, the child should be seated in an upright position with the practitioner looking from a distance at three points: (1) the bridge of the nose, (2) the base of the upper lip, and (3) the chin. This examination gives the observer an idea of the patient’s profile.
A straight profile is indicated when all three points are at the same level and form a straight line. If the midpoint is anterior, the patient has a convex profile; if the midpoint is posterior, the patient’s profile is concave (Fig 3-6). Each of these three profiles can be caused by abnormalities of one, two, or three point combinations. For example, a convex profile can result from maxillary protrusion, mandibular retrusion, or a combination of both.
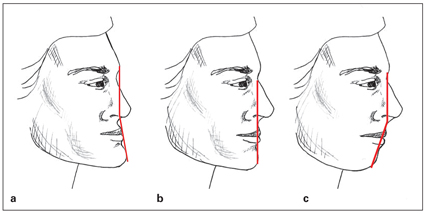
Fig 3-6 Profile types: (a) concave; (b) straight; (c) convex.
Slight retrusion of the mandible before puberty can be considered normal. This dimension will catch up to the maxilla with normal growth of the mandible. Slight convexity of the profile at this age can also be considered normal.
A well-balanced profile usually indicates the presence of a normal or Class I occlusion. An underlying normal skeletal relationship that has no skeletal discrepancy in the anteroposterior relationship, molars and canines with a normal relationship, and primary second molars with a terminal plane that is flush or has a mesial step can be considered normal.
Some children may have normal basal bone relationships but disturbed profiles. These situations may be due to abnormal inclination of the incisors such as that resulting from abnormal, nonnutritive oral habits. Correction of incisor protrusion will improve the profile.
Children with a severely convex profile usually have a Class II malocclusion, and those with a straight or concave profile can have a Class III malocclusion. The clinical and paraclinical examinations can clarify the exact type of malocclusion, whether it is the result of dental or skeletal factors (or a combination of both) or the result of maxillomandibular or dental discrepancies.
The morphology of the patient’s profile is also another important area that can change the treatment plan. For example, tooth extraction can be considered in children with a convex profile if other analyses confirm extraction, while extraction should be avoided in children with a straight or concave profile.
Divergence of the face is a termed used by Hellman.13 Divergence indicates if a profile slopes either anteriorly (anterior divergence) or posteriorly (posterior divergence). Divergence is influenced by the patient’s racial and ethnic background. For example, while people of American Indian and Asian descent tend to have an anteriorly divergent face, white people of northern European descent are likely to show posterior divergence.14
The upper-lower facial proportion, nose, chin, and lips as well as the interrelationships of these components must also be examined during the evaluation.
Intraoral Examination
Intraoral examinations for orthodontic patients, as for any other type of patient, require a thorough evaluation of the health of all oral hard and soft tissue structures. Any problem, disease, or pathologic condition, including medical problems, dental caries, and pulpal or periodontal involvement, must be treated and under control before orthodontic treatment begins.
The orofacial structure and occlusal system consist of three basic tissues:
1. Dental tissues, consisting of enamel, dentin, cementum, pulp, and the periodontal ligament
2. Skeletal tissues, consisting of bone, cartilage, and ligaments
3. Soft tissues, consisting of neuromuscular tissue, epithelial tissue, glands, the circulatory system, mucous membranes, and connective tissue
The oral cavity and all of the tissue components have several interrelated physiologic functions that directly or indirectly play some role in the development of dental occlusion. Therefore, treatment planning must be based on a thorough examination of all of these structures, in both static and functional states.
For example, evaluating the dental arch relationship in centric occlusion and looking at the relationship of maxillary and mandibular first molars are not sufficient means to classify the type of occlusion. It is necessary to assess all types of mandibular movement, such as protrusive, retrusive, and lateral excursions, and the dental and facial midline relationships at wide open, rest, occlusion, and path of closure. Assessment of the relationships between rest position and occlusion can differentiate between a functionally true and a forced-bite malocclusion caused by a mandibular shift.
Rest position is the result of a myotatic antistretch reflex in response to gravity; it alters with the position of the head, and natural head position must also be determined for each patient.
To emphasize the important role of orthodontic diagnosis, especially in early treatment, important areas of this assessment are discussed in static and functional evaluations.
The following are important features to consider in the static evaluation of the oral cavity (see Fig 3-1):
• Oral health
• Lips (position relative to each other and to incisors)
• Caries susceptibility and restorations
• Dental age (tooth eruption and sequence)
• Tooth size, forms, and number
• Periodontal and oral mucosal conditions
• Tongue size, posture, and function
• Frenum and oral mucosa
• Adenoids and tonsils
• Type of occlusion (classification, overjet, overbite, midline, urve of Spee)
The following are important features to consider in the functional evaluation of the oral cavity (see Fig 3-1):
• Perioral musculature, including the tonicity and function during mastication, deglutition, respiration, and speech
• Lip competency, tonicity, and function during rest, swallowing, speech, and respiration
• Dental and facial midline relationships at wide open, rest, occlusion, and path of closure
• Mandibular movements and protrusive, retrusive, and lateral excursions
• Freeway space
• TMJ function and dysfunction and condylar movements
• Mode of breathing
Evaluation of the dentition
The first step of occlusal development starts when primary first molars reach occlusion. Numerous reports indicate that many malocclusions develop during primary and early mixed dentition and are recognizable and preventable.15 Evaluation and classification of the primary dentition are important steps for early detection and intervention. Inspection of a child’s dental occlusion must be performed first during the late primary dentition and then before eruption of the permanent first molars.
At this age, occlusion must be carefully examined in three dimensions (sagittal, vertical, and transverse) in both centric occlusion and centric relation. The interdental spacing (Baume classification),16–19 crowding, primate space, terminal plane, primary molar and canine relationship, overjet, overbite, and midline must be evaluated. The child’s age and tooth eruption pattern are also very important to evaluate.
The development of the childhood dentition and resulting occlusion is a dynamic process, occurs in all three planes of space, and may undergo considerable change during childhood and early adolescence. With periodic evaluations, the practitioner can intercept and favorably influence undesirable changes. After more than 40 years of orthodontic practice, especially involving young children, the author believes that many eruption problems can be prevented if the problem is detected early and intervention is started early. The best way to detect these problems is longitudinal monitoring of panoramic radiographs, which is discussed later in this chapter.
Eruption that is early or delayed by a few months is not harmful unless local or systemic problems prevent normal eruption. Any early or late eruption that is detected clinically, especially if it is asymmetric, must be evaluated radiographically to determine if a problem exists.
Asymmetric eruption between the right and left sides of the dental arch lasting more than 6 months is another problem that may require early intervention. Likewise, an abnormal sequence of eruption can be very harmful to occlusal development and deserves careful assessment during the intraoral examination. Early loss and delayed exfoliation of primary teeth are etiologic factors in some malocclusions. These must be detected at an early stage through a complete intraoral examination.
Other eruption problems, such as ankylosis, tooth transposition, ectopic eruption, and tooth impaction, must be evaluated clinically and radiographically (see chapter 10).
Problems of tooth size, form, and number (missing or supernumerary teeth) are other factors that can interfere with normal eruption and tooth displacement. The absence of a mandibular incisor or the presence of a supernumerary mandibular incisor is easily overlooked; counting the teeth during the examination can prevent these problems (see chapters 6 and 7).
The intraoral examination should include assessment of the following aspects of the dentition (see Fig 3-1):
• Primary occlusion (interdental spacing, terminal plane, and mandibular shift)
• Dental age
• Eruption pattern of the dentition
• Asymmetric eruption
• Early loss and delayed exfoliation of primary teeth
• Eruption problems such as ankylosis, tooth transposition, ectopic eruption, and impaction
• Problems of tooth size, form, and number (missing or supernumerary teeth)
• Dental and facial midlines
Evaluation of soft tissues
Another area of inspection during intraoral examination is evaluation of the soft tissues. The buccal tissues, lips, floor of the mouth, palate, and gingiva should be carefully inspected and palpated. The gingival tissue in young children might be redder and smoother than that of adults because of increased vascularity and thinner epithelium.
Early detection of periodontal involvement before treatment is important; careful probing can be very helpful. Bleeding during probing is indicative of active disease, which must be brought under control before other treatment.
Crowded mandibular incisors must be carefully assessed for tissue recession, especially when attachment to the gingiva is inadequate. Extraction and nonextraction options must be carefully evaluated.
Recent findings suggest that periodontal disease may have its origins in childhood. A noted increase in the frequency of gingival inflammation in children and progressive periodontal conditions causing primary and permanent tooth loss led the American Academy of Pediatric Dentistry to place greater emphasis on prevention, early diagnosis, and treatment of gingival and periodontal disease in children.20
Other areas of the soft tissues that can play an important role in diagnosis and treatment planning in early-age orthodontic treatment are the tongue, frenum, lips, and adenoid and tonsillar tissues. Growth and development of maxillofacial morphology and oral function are closely interrelated.
The tongue has several necessary functions for life and at the same time can play an important role in development of the occlusion. The tongue has three main functions. First, it carries on its surface the taste buds, which send information to the brain about the nature of the food being eaten. Second, the tongue plays an important part in the process of mastication and deglutition. Third, the tongue is involved in speech, assuming different positions in the mouth and altering the shape of the air passage through which sounds made by the vocal cords will pass.
Most tongue postures and movements during normal function exert some forces on the dentition that are in balance with other neuromuscular forces exerted by the perioral musculature. Any imbalanced force, especially at early stages of the dentition, can cause morphologic changes in the occlusal system. Therefore, this structure must be evaluated, in both static and functional states, for the purpose of orthodontic diagnosis and treatment planning. This assessment is based on three important conditions of the tongue: (1) tongue size, (2) tongue posture, and (3) tongue function.
Tongue size
The interaction between tongue size and volume and craniofacial skeletal growth is essential for understanding the mechanism of specific types of malocclusion and treatment planning.
Harvold et al,21,22 using rhesus monkeys, demonstrated that reducing tongue volume by partial glossectomy caused the dental arch to collapse lingually and produce crowding.
One of the factors that plays an important role in the development of the occlusion is the balance between the tongue and the perioral chain of muscle. Any imbalance between these two factors can cause irregularities in occlusion. For example, in patients with acromegaly, macroglossia causes many types of irregularities, such as interdental spacing, anterior open bite, dental protrusion, and Class III malocclusion (Fig 3-7).

Fig 3-7 (a to c) Macroglossia causing a large mandibular arch, anterior and posterior crossbites, and anterior open bite. (Courtesy of J. Daniel Subtelny.)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


