Management
of Sagittal Problems
(Class II and Class III)
A major and important objective of early treatment during the primary and mixed dentitions is enhancing the normal growth and development of dental occlusion. Recent studies indicate that genetic mechanisms have more influence on the morphogenesis of craniofacial structure during embryonic life, while environmental factors influence the developing occlusion, especially during the early postnatal period.1
The first step in development of the vertical dimension of occlusion is established when the primary first molars reach occlusal contact. When the primary second molars reach occlusion, their distal surfaces (terminal plane) play an important role in the sagittal dimension of final occlusion.
It is also known that establishment of the occlusion is under the control of genetic and environmental influences and influenced by the interaction of growth and development of basal bone and other craniofacial structures. All of these structures are also under the influence of neuromuscular and soft tissue structures and their functional matrix. Disturbance of any of these components or the occurrence of disharmony or dysfunction during the development of occlusion can result in abnormal occlusion.
Many incipient malocclusions that are under the influence of environmental factors during the primary or mixed dentition could be preventable; early recognition of these anomalies and interception can eliminate or reduce the severity of future problems. There are special orthodontic problems that require early intervention, even in very young patients during the primary or early mixed dentition; these include Class II malocclusion, anterior dental crossbite, and dentoskeletal Class III malocclusion, which will be discussed in this chapter, as well as posterior crossbite, especially if it is associated with a lateral mandibular shift (see chapter 12), open bite associated with persistent oral habits or other oral dysfunction (see chapter 13), space management (see chapter 4), severe incisor protrusion (see chapter 5), and craniofacial anomalies such as clefts or hemifacial microsomia (see chapter 7).
Understanding the mechanisms of early detection and orthodontic intervention requires a thorough understanding of the development of the dentition (see chapters 1 and 2). The major goal of early intervention is to eliminate or reduce the damage from etiologic factors that cause trauma to the occlusion or interfere with the normal growth and development of occlusion, thereby providing an environment that promotes normal jaw growth and an optimal eruption pattern during the transitional dentition.
Proper intervention at early ages both corrects the present abnormalities and eliminates or minimizes more severe problems that can occur later. Depending on the type of problem and the dental and skeletal age of the patient during treatment, some patients may need a second or third phase of treatment. However, the final phase is usually much easier and faster after early intervention. Some patients may not need any further treatment.
The timing of early treatment is controversial; some practitioners advocate for treatment during the primary dentition, and some orthodontists prefer to begin treatment during the mixed dentition. There is also controversy about whether the early, middle, or late mixed dentition is preferable. The American Association of Orthodontists2 recommends that the initial orthodontic evaluation occur at the first sign of orthodontic problems or no later than the age of 7 years.
Examination of a child’s dentition during the primary dentition does not always mean treatment; careful examination can detect and anticipate developing problems at this early age and clarify the possibility of early intervention. The orthodontic examination, especially during the primary and early mixed dentitions, is more than merely an examination of dental occlusion. The assessment should include diagnosis of facial or skeletal problems that are initiating and developing in a growing child. Problems such as upper airway obstruction (mouth breathing), temporomandibular dysfunction, and abnormal myofunctional habits can have adverse effects on dentoskeletal structures. If problems are recognized early and preventive measures are instituted, many facial and dental problems may be minimized or averted.
Gugino and Dus3 stated that the human face is anatomically and functionally one of the most complex regions of the human body. A sound understanding of the physiology of the stomatognathic system is an important requirement for clinicians who wish to provide their patients with the best orthodontic and orthopedic treatment results. Therefore, clinicians must understand the basic process of occlusal development, always be aware for cautious detection, and decide on a case-by-case basis when to provide orthodontic intervention.
Early treatments follow two major strategies:
1. Removal of etiologic factors and restoration of a normal environment to facilitate normal growth and development of the dentition
2. Guidance of tooth eruption and the growth pattern to a normal state to correct or reduce the severity of dentoskeletal malrelationships
This chapter discusses common sagittal abnormalities that initiate and develop during the primary or early mixed dentition, are not self-corrected, and in some situations worsen in later stages of the dentition:
• Class II malocclusion (Class II division 1 and Class II division 2)
• Anterior dental crossbite
• Dental and dentoskeletal Class III malocclusion
Class II Malocclusion
Two large-scale surveys carried out by the United States by the Division of Health Statistics of the US Public Health Service covered 6- to 11-year-old children and youths aged 12 to 17 years. The surveys indicated that Class II malocclusion accounts for about one-third of the total malocclusions of the US population,4 with variable combinations of dental and skeletal factors contributing to the disharmony. Class II malocclusion usually causes esthetic and functional problems of varying severity, depending on the amount of anteroposterior discrepancy and its interaction with adjacent soft tissues.5
Long-term studies from the primary to the permanent dentition have shown that Class II abnormalities are not self-correcting and in some cases may worsen with age.6,7 Not all Class II malocclusions are alike; numerous types of skeletal and dental Class II malocclusions might be observed under Class II molar relationships.
A review of older literature indicates that Class II discrepancy has mainly been perceived as a sagittal problem. The characteristics of these anomalies have been classified under four sets of anteroposterior criteria: (1) maxillary skeletal position, (2) maxillary dentoalveolar position, (3) mandibular skeletal position, and (4) mandibular dentoalveolar position. The vertical and transverse dimensions were not considered to be related to Class II discrepancy; however, later research showed that either of these dimensions may be involved.
Schudy8 showed that variations in facial height may conceal or intensify the clinical appearance of Class II malocclusion. An increased mandibular vertical dimension in association with Class II malocclusion usually rotates the mandible downward and backward, which manifests as a more retruded mandible and a more convex profile. Any mistake in treatment would worsen the situation. A decreased vertical dimension causes the mandible to rotate upward and forward, manifesting as a prominent chin point.
The transverse dimension also must not be overlooked in evaluation of Class II malocclusions. Most Class II patients with a narrow maxillary arch may show a normal relationship of buccal segments in centric occlusion. Tollaro et al9 investigated posterior transverse interarch discrepancy (PTID), which was measured as the difference between the maxillary and mandibular intermolar width, in two Class II division 1 groups: one with PTID and one without PTID. In the Class II group with PTID, mandibular retrusion was associated with a posteriorly displaced mandible of normal size (functional mandibular retrusion). In the Class II group without PTID, mandibular retrusion was caused by a micrognathic mandible (anatomical mandibular retrusion).
Sometimes an underlying transverse discrepancy of 3 to 5 mm exists in the dental arch. This maxillary constriction can be unmasked clinically by having the patient bring the mandible forward to a Class I molar relationship.
Early intervention in transverse problems and proper expansion at earlier stages will facilitate forward growth of the mandible. Although Class II malocclusion is perceived as a sagittal problem, the vertical and transverse dimensions of each patient must also be considered in treatment planning.
Morphologic characteristics
The molar or canine relationships in patients with Class II malocclusion constitute only one part of a broader and extended syndrome and cannot clearly define treatment planning. Different morphologic characteristics of Class II malocclusion can be caused by malrelationships of the basal bone, malrelationships of the dentition, dentoalveolar or dentoskeletal malrelationships, or some combination of these factors (Box 11-1). In addition, discrepancies in other bony structures, such as different growth or different angulation of the anterior and posterior cranial bases, can have destructive effects on jaw harmony and occlusion (Box 11-2). Figure 11-1 shows different variations of skeletal Class II malocclusion that can develop, depending on the morphologic characteristics of basal bone.
| Box 11-1 | Morphologic characteristics of the jaws in patients with Class II malocclusion |
| • Maxillary basal protrusion • Maxillary dentoalveolar protrusion • Maxillary counterclockwise rotation • Overdevelopment of the maxillary length relative to the mandible • Vertical overgrowth of the maxilla • Mandibular basal retrognathism |
• Mandibular dentoalveolar retrognathism • Underdevelopment of the mandibular length relative to the maxilla • Overgrowth of the ramus relative to the mandibular body • Underdevelopment of the ramus relative to the mandibular body |
| Box 11-2 | Morphologic characteristics of other bony structures in patients with Class II malocclusion |
| • Increased anterior cranial base length, causing anterior positioning of the maxilla • Increased posterior cranial base length, causing posterior positioning of the mandible |
• Increased saddle angle (nasion-sella-articulare, N-S-Ar), causing posterior positioning of the condyle • Increased articular angle (sella-articularegonion, S-Ar-Go), causing posterior positioning of the mandible |
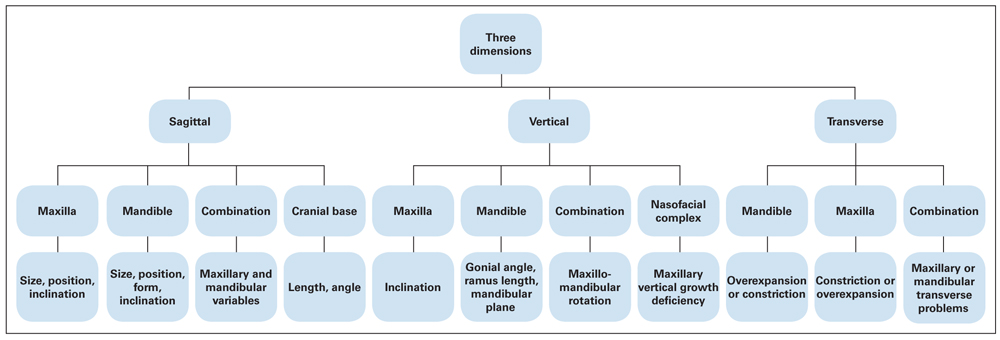
Fig 11-1 Possible variations of Class II malocclusions based on skeletal components.
Diagnostic procedures
Class II malocclusion is a multifactorial entity caused by hereditary factors or abnormally acquired environmental factors that produce aberrations in form and function during occlusal development. Therefore, thorough diagnostic evaluations are necessary for correct identification of etiologic factors and affected anatomical structures as well as proper treatment planning for correction of Class II malocclusion.
The dental occlusion and dental arch are not an isolated entity; rather, they are a part of an extensive system comprising the teeth, basal bone, and other skeletal structures of the face and cranium that interact with the neuromuscular system and surrounding soft tissues. All kinds of dentoskeletal malocclusions, including Class II types, are associated, to one degree or another, with the relationships of the following six dentoskeletal components:
1. Cranium and cranial base
2. Skeletal maxilla
3. Nasomaxillary complex
4. Maxillary teeth and alveolar process
5. Skeletal mandible
6. Mandibular teeth and alveolar process
These are independent functional units, but their interrelationships in three dimensions can produce several variations in the morphology of all dentoskeletal malocclusions, including Class II forms.
Cephalometric analysis
Proper treatment planning for dentoskeletal malocclusions cannot be established without a thorough evaluation of the interrelationships of these compartments relative to the dentition and dental occlusion. Since the introduction of the cephalometric technique by Broadbent10 in 1931, a variety of analyses has been presented by different investigators.
One of the goals of cephalometric analysis is to establish the relationships of these functional components in both the anteroposterior and vertical planes of space in order to differentiate the type of malocclusion. Research reports that have evaluated the morphology of the maxillomandibular relationship in patients with Class II malocclusion have reached differing conclusions. Some reports have indicated a high percentage of maxillary base protrusion,11 and some reports have indicated a higher percentage of mandibular base retrusion.12 Variations also exist in dentoalveolar types. Although Class II is perceived as a sagittal problem, the vertical and transverse dimensions of each patient must also be considered.
It is not the intention of this book to discuss cephalometric analysis; there are many valuable sources for this information. However, the reader should note the importance of these tools for differential diagnosis in dentoskeletal malocclusion, including Class II malocclusion, especially in early treatment approaches aiming for growth modification.
In cephalometric evaluation of dentoskeletal malocclusions and differentiation of various components of each malrelationship, it is wise not to rely on any specific angle or linear measurement; no single measurement may be reliable all the time, and other data are available. For example, because of variability in length and inclination of sella-nasion in some patients, the sella-nasion–point A (SNA) and sella-nasion–point B (SNB) angles cannot always be accurate in anteroposterior evaluation.
In all sagittal evaluations of Class II dentoskeletal malrelationships, besides the SNA and SNB measurements, the Landes angle (nasion–point A to Frankfort plane) provides a high degree of reliability for the maxilla. The Wit analysis (perpendicular lines drawn from point A and from point B to the occlusal plane) can also be used to compare the anteroposterior relationships of the maxilla and the mandible.
Growth prediction
Another important aspect of cephalometric analysis is prediction of the growth pattern, which is critical in treatment planning, especially for growing patients. Many efforts have been made to develop methods for growth prediction from cephalometric radiographs. Successful prediction is achieved when the amount and the direction of growth are predicted before early-age treatment.
Orthopedic interventions for growing children should be preceded by careful cephalometric evaluation of all components of dentoskeletal structures, such as the cranium and cranial base, the skeletal maxilla and nasomaxillary complex, the skeletal mandible, the maxillary teeth and alveolar process, the mandibular teeth and alveolar process, and especially the potential direction of jaw growth for the child. Facial divergence and convergence, Frankfort plane–mandibular incisor angle (FMA), gonial angle, y-axis, anterior and posterior facial heights, and posterior and anterior cranial base lengths and angulations are examples of measurements that can indicate children’s potential growth pattern.
Advantages of early treatment
Early orthodontic treatment for Class II malocclusion has the following benefits:
• It affords the greatest utilization of skeletal growth.
• Skeletal disharmony can be controlled in three dimensions (sagittal, vertical, and transverse).
• Observation and guidance of eruption during the transitional dentition are promoted.
• Disarticulation of the posterior segment during tooth eruption facilitates normal interdigitation.
• Leeway spaces within the dental arches are preserved.
• The need for tooth extraction is reduced.
• Better skeletal harmony is achieved.
• Results are more stable.
• Early treatment of unesthetic malocclusion can have an important impact on the psychosocial development of the patient.
• Fractures caused by trauma to protruded incisors are prevented.
• Patients exhibit better compliance at earlier ages.
The major goal of early treatment is to correct or reduce the adverse effects of dentoskeletal and muscular imbalance by improving the environment to encourage optimal occlusal development.
Class II Treatment Options
A Class II malocclusion can have various anatomical, morphologic, and functional characteristics. Treatment strategies differ depending on the special characteristics of this anomaly. Class II treatment also varies according to the skeletal age of the patient. Growth modification strategy is entirely different from treatment tactics applicable after completion of the growth spurt. Depending on the type of Class II malocclusion present and the age of the patient, four treatment options are available for Class II correction:
1. Camouflage treatment
2. Orthognathic surgery
3. Growth modification and occlusal guidance
4. A combination of the above
Camouflage treatment
Camouflage treatment is used in the permanent dentition, usually after the growth spurt, to obtain optimum results within the physiologic limits of each patient. With camouflage treatment the goal is to produce acceptable dental relationships and disguise unacceptable skeletal relationships through tooth movement, which may or may not require serial extractions. This type of treatment is indicated in adolescent and adult patients with mild to moderate skeletal problems.
Orthognathic surgery
Orthodontic treatment combined with surgical procedures is applied in adult patients to correct dental malrelation-ships and skeletal disharmonies. These types of treatments are usually implemented in individuals with severe dentoskeletal malrelationships caused by heredity, skeletal disharmony, or congenital skeletal malformation.
Growth modification and occlusal guidance
Growth modification and occlusal guidance treatments are interceptive treatments that are applied in growing children during the primary or mixed dentition to eliminate or minimize the dentoalveolar and skeletal disharmonies that can interfere with the normal growth and development of occlusion. The main objective of this type of intervention is to prepare an environment that will enhance the positive effects of growth potential for improving occlusal development.
Early versus late orthodontic treatment, especially early treatment for Class II problems, is one of the greatest controversies in orthodontics. Randomized clinical trials have been specifically designed to address these important issues in Class II treatment. Keeling et al,13 Tulloch et al,14 and Ghafari et al15 concluded that early treatment followed by later comprehensive treatment of Class II malocclusion associated with moderate to severe deformity does not produce major differences in jaw relationships or dental occlusion compared with later one-stage treatment.
On the other hand, many other experienced researchers and clinicians, including Gugino and Dus,3 Ricketts,16–18 Subtelny,19 Bench et al,20 Graber,21 and McNamara,22 insist that there are many disadvantages to waiting for eruption of the permanent dentition and second molars. In addition, many animal studies, carried out by pioneers such as Harvold et al,23 Woodside et al,24 and McNamara25 have clearly shown the histomorphologic changes induced in animal jaw growth by orthopedic forces.
Most dentoskeletal anomalies develop during the primary and mixed dentitions, and, according to Carlson,26 the midface and the mandible complete only 50% of their total growth by age 8 to 10 years; thus, a considerable amount of midface and mandibular growth occurs during the transitional dentition, which provides a good opportunity to intervene.
Long-term studies from the primary to the permanent dentition have also shown that Class II abnormalities are not self-correcting and in some cases may even worsen.6,7 Why should dental practitioners allow an unfavorable dental, skeletal, or soft tissue relationship to remain for a number of years if it can be corrected completely or at least partially at an earlier age with minimal appliance therapy and treatment effort, by taking advantage of the child’s growth potential?
Deviations in skeletal growth patterns accompanied by a disturbed functional matrix environment, such as mouth breathing, atypical swallowing, or other abnormal behaviors that can disturb jaw growth, require early intervention to eliminate or modify the condition and give orthodontists the opportunity to guide dentoalveolar development.
History of growth modification tactics
The mandible is the only freely functioning bone in the body not connected to another bone. It is tied to its contiguous structures by 13 attached muscles. The mandibular position in three planes of space (sagittal, vertical, and transverse) plays an important role in harmony of the dental occlusion. These specifications of the mandible have drawn orthodontists for many years to the possibility of influencing the mandibular position by altering the structure of the temporomandibular joint.
In 1880, Kingsley27 introduced the concept of jumping the bite for correction of mandibular retrusion. He designed a vulcanite palatal plate consisting of an anterior inclined surface to guide the mandible to a forward position. This idea influenced the development of functional jaw orthopedic treatment. Graber et al28 provided a brief history of different functional devices developed in the past century. Hotz, by modifying the Kingsley device, introduced the Vorbissplatte for treatment of severe overbite, mandibular retrusion, and retroclined incisors by muscle hyperactivity. Pierre Robin, a French physician, introduced the monobloc in 1902 as a passive positioning device for his patients to prevent glossoptosis (blocking of the airway by the tongue).
Viggo Anderson was familiar with the appliances of Kingsley and Pierre Robin and, in 1908, without thinking of “guiding growth,” applied a monobloc as a retainer for his daughter to eliminate adverse effects of abnormal function. He found that use of the appliance resulted in sagittal correction and profile improvement. Later, Anderson, in association with Haupl, named the appliance the activator because of its ability to activate the muscle forces.
In 1927, Emil Herbst introduced the fixed functional appliance (Herbst appliance). Later several modifications of the activator were introduced by different investigators, such as the Bionator by Balters in 1965, the functional regulator inducing muscle stretch by Fränkel29 in 1966, functional headgear (combined headgear and Bionator) by Stockli30 in 1973, fixed Herbst fully banded appliances by McNamara,22 the twin block (two-piece functional) appliance by Clark31 in 1977, and the magnetic activator device by Darendeliler and Joho.32
Several methods of Class II treatment that do not rely on significant patient compliance have become popular during the last decade, including several versions of the Herbst appliance and the Pendulum or Pendex molar distalization appliance. Theoretically, however, these general approaches have opposite treatment effects, one presumably enhancing mandibular growth and the other moving the maxillary teeth posteriorly. In 2007, Seifi et al33 introduced a two-piece functional appliance for Class II deep bite correction with a simple design, mandibular incisor capping, a palatal plate for maintaining the mandible in the protruded position, and without occlusal coverage so that no acrylic adjustment is necessary.
Functional appliances
Generally, functional appliances are removable devices designed to alter the neuromuscular environment of the orofacial region and to improve occlusal development and/or the craniofacial skeletal growth pattern through the following mechanisms:
• Utilization of muscle force to achieve dentoskeletal changes
• Disarticulation of the teeth to facilitate changes of inter-digitation
• Alteration in the eruptive paths of teeth
• Promotion of mandibular protraction to enhance forward mandibular growth
• Utilization of different pads to change the equilibrium of the perioral muscles
Functional therapy has several goals:
• Creation of a more favorable environment for occlusal development
• Enhancement of the normal growth of the basal and craniofacial skeletons
• Promotion of a normal growth direction of the craniofacial skeleton
• Selective inhibition or control of unfavorable growth
• Guidance of erupting teeth into more favorable positions
Extraoral traction
The use of extraoral devices to achieve growth modification in patients with Class II malocclusion goes back to the use of extraoral traction in the treatment of maxillary protrusion, first employed by Oppenheim34–36 in 1936. In 1947, Kloehn37 recommended headgear treatment in growing children to guide alveolar growth and eruption of the teeth, to reduce treatment time, and to produce a more balanced dentition and face. Since then, other investigators have reported on the effects of headgear use in early treatment of Class II malocclusions and recommended the use of headgear as one of the most reliable methods for management of maxillary protrusion.16–18,37,38
Kopecky and Fishman39 established that early orthodontic treatment and growth modification are best achieved before and during the growth spurt. Baccetti et al,40 in a cephalometric study, evaluated the role of timing in relation to skeletal maturity on the outcomes of comprehensive, nonextraction Class II therapy. They concluded that treatment of Class II malocclusion before or during the pubertal growth spurt induces significant favorable skeletal changes. They also stated that use of headgear during the prepubertal stage restricts maxillary advancement and enhances mandibular growth. The only significant changes in patients treated after the pubertal growth spurt were dentoalveolar changes.
The effects of headgear alone or headgear combined with other devices on the dentition or jaws have also been reported by many investigators. These reports reveal several changes, such as molar relationships, SNA changes and downward tipping of the palatal plane, opening or closing of the bite, maxillary molar extrusion, intrusion, downward or backward rotation of the maxilla and consequently mandibular rotation, and increases in anterior facial height.4,24,34–36,41–43
Applications of headgear in combination with removable or fixed and functional appliances have also been reported. Cephalometric evaluation in Class II division 1 patients treated with the Cetlin method—use of cervical headgear, lip bumper, and maxillary removable plate with springs to distalize the molars— showed a significant distal tipping in 70% of the treated patients and significant limitation of maxillary forward growth but no significant change in the mandibular position.42
The lip bumper is another orthodontic device that has several indications in early orthodontic treatment, especially in some Class II malocclusions. Many investigators have reported the effect of lip bumper application on transverse, sagittal, and vertical changes in occlusion.19,44,45 These reports indicated that the lip bumper has several effects: increase in arch length, uprighting of mandibular first molars, bodily dental expansion, alveolar bone remodeling, proclination of mandibular incisors by reduction of lip muscle force and abnormal dysfunction and thereby reduction of overjet, correction of the curve of Spee, opening of the bite, and maintenance of leeway space.19,44,45
The Hawley appliance also has many applications as a passive or active appliance in orthodontic treatment, including as an anterior bite plate for reducing overbite and overjet by retroclination of maxillary incisors and as a slow expander by adding a jackscrew.
Early Class II Treatment with Headgear, Lip Bumper, and Hawley Appliance (HLH) Technique
This section introduces a technique for early treatment of Class II malocclusions during the mixed dentition. In this technique, a combination of headgear, a lip bumper, and a Hawley appliance, which the author calls the HLH technique, has been designed with certain modifications.
To explain the characteristics, mechanisms, and the reasons for the modifications that have been applied in the HLH technique, it is necessary to review briefly the application and original function of each of these three devices separately.
Headgear
As an extraoral device, headgear can exert different directions of force to the basal bone and dentition and produce different treatment effects on the occlusion. Success in the application of headgear depends on three important factors: application at the proper time of growth, the patient’s cooperation, and proper mechanical management.
Proper timing
The proper age for starting early orthodontic treatment and achieving proper growth modification is just before and during the growth spurt, as has been advocated by some investigators.40 Kopecky and Fishman39 also indicated that this type of treatment has the best results when implemented before and during the growth spurt, which coincides with a value of 4 to 7 according to Fishman’s method46 of skeletal maturation assessment.
Patient’s cooperation
The patient’s cooperation is an important factor in treatment in any orthodontic treatment, especially in headgear wear, and must be considered in treatment planning. Practitioners have an important role in gaining the understanding of patients and parents and must explain the patient’s dentofacial problems as well as the necessity and advantages of orthopedic force.
Proper mechanical management
Contrary to perceptions that headgear application is an easy procedure, the mechanical management of headgear therapy is a procedure that requires precision. Headgear consists of three parts: the facebow, the anchorage pad, and a strap for traction. Depending on whether tipping, bodily, or combination movement is desired for the teeth or the maxilla, the following determinations must be made:
• Location of anchorage
• Location of the inner bow attachment
• Position of the outer bow relative to the inner bow (above, below, or at the same level)
• Type of outer bow (short, medium, or long)
The location of anchorage can be cervical, occipital, or a combination. A cervically located headgear pad with a long outer bow exerts a distal and low force on the teeth and the maxilla. This design has distalization and extrusion effects on the molars and a tipping effect on the palatal plane (counterclockwise rotation). The best indication for this configuration is Class II deep bite in a patient with a horizontal growth pattern.
High-pull headgear, in which the anchorage pad is located on the occipital area, exerts a vertical and distal force on the maxillary molars and maxillary base and causes intrusion and distal movement. Depending on the size of the outer bow (short or medium) used with high-pull headgear, different effects on the molars and the maxilla can be achieved. These include intrusion and distal tipping or intrusion and distal bodily movement.
Combination headgear has a combination of cervical and occipital pull that imparts a straight distal force to the molars for controlling extrusion and distal movement.
In all mentioned types of headgear, the size of the outer bow (short, medium, or long) and the position of the outer bow relative to inner bow (above, below, or at the same level) can change the direction of forces.
Another mechanical specification of headgear that can have different effects on the dentition and basal bone is the location of the inner bow attachment. The inner bow is commonly connected to molar tubes, but in certain situations it can be connected to the anterior segment of the maxillary archwire (like J-hook headgear), such as in patients who need incisor retraction accompanied with intrusion.
In a headgear–functional appliance combination, the inner bow can be inserted in an acrylic resin pad in the anterior, molar, or premolar area, depending on the desired direction of orthopedic force.
The following are the mechanical functions of headgear, which may vary with different configurations:
• Establishment of normal molar relationships
• Restriction of forward maxillary growth (prevention of forward movement of point A)
• Restriction of vertical maxillary growth (high-pull headgear)
• Creation of minor space by distalization of molars (tipped or bodily, depending on the type of headgear)
• Extrusion of maxillary molars to reduce overbite
• Intrusion of maxillary molars to reduce open bite or open bite tendency
• Correction of molar rotation
• Expansion of molar region
• Constriction of molar region
Modified Hawley appliance
The second component of the HLH technique for early treatment of Class II malocclusion is a modified Hawley appliance (Fig 11-2). The modified appliance has the following specifications:
• Two C-clasps: These are simple clasps made with 0.032- or 0.036-inch stainless steel wire and designed to be inserted in an acrylic resin pad that runs from the distal surface of the molars over the molar buccal tube and extends to the premolar area for easy removal.
• An inclined acrylic resin pad: The pad is placed behind the maxillary incisors for mesial movement of the mandible during closure. The position of this pad varies, depending on the severity of overjet and sagittal discrepancy of the maxilla and the mandible.
• A standard labial bow: The bow is designed to maintain anterior retention and help incisor retraction if needed.
• In some cases, 2 × 4 bonding instead of a labial bow: Another modification might be necessary in some patients with maxillary incisor crowding, rotation, or overlap that cannot be managed by a labial bow. In this situation, the Hawley appliance is designed without a labial bow; instead, 2 × 4 bonding can be used simultaneously with the inclined acrylic resin pad to achieve leveling, unraveling, and correction of crowding in the incisors.
• Addition of a jackscrew for expansion of the posterior arch segment: The jackscrew is added when patients with Class II malocclusion also have transverse problems.
• Occlusal acrylic resin coverage in the posterior regions: Occlusal coverage is a modification that might be needed in patients with Class II malocclusion, anterior open bite or open bite tendency, and a vertical growth pattern, where all of the effort must be focused on controlling the vertical dimension.
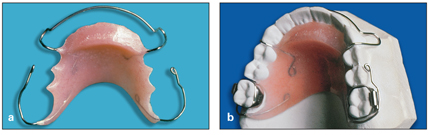
Fig 11-2 (a and b) Modified Hawley appliance designed for the HLH technique.
When the modified Hawley appliance is used in conjunction with headgear, the following treatment results can be achieved:
• Unilateral or bilateral distal movement of the molars by distal positioning of the C-clasp to achieve Class I molar relationships
• Distal maxillary traction, applied to the whole maxilla as a unit, for orthopedic action to control maxillary growth and correct point A–point B (A-B) discrepancy
• Mandibular forward displacement as an orthopedic force to achieve mandibular protraction
• Correction of deep bite by anterior placement of the acrylic resin pad and opening of posterior bite and extrusion of molars by cervically placed headgear.
• Correction of anterior open bite or open bite tendency by the addition of posterior occlusal acrylic resin coverage to the modified Hawley in conjunction with high-pull headgear
• Maxillary arch expansion, if needed, by the addition of a jackscrew to the modified Hawley appliance
Lip bumper
The third appliance used in the HLH technique is the lip bumper, which consists of two molar bands with a double buccal tube—one a round 0.040- or 0.045-inch tube for insertion of the lip bumper bow and one for insertion of the archwire—and an acrylic resin or plastic pad located behind the lower lip.
In patients that need some buccal expansion, the pad can be extended toward the buccal segments to separate perioral muscle force, facilitate natural arch expansion, and perhaps initiate bone remodeling. Many investigators have reported on the stability of this type of expansion that takes place during occlusal development.19,45
The lip bumper has several indications in early orthodontic treatment, especially in some types of Class II malocclusion. As mentioned earlier, many investigators have reported use of different types of lip bumper and the transverse and vertical changes they have on occlusion.17,42,43
As a part of the HLH technique, the lip bumper is used in conjunction with headgear and a modified Hawley appliance for the following conditions:
• Class II division 1 malocclusions associated with deep bite, deep curve of Spee, and retruded and sometimes crowded mandibular incisors are usually the result of early loss of mandibular primary canines or primary first molars, combined with lip dysfunction. These cases are ideal for lip bumper application.
• The lip bumper can upright permanent molars, procline mandibular incisors, correct curve of Spee, and reduce overbite in patients with Class II division 1 malocclusion who exhibit deep bite and tipped mandibular permanent molars due to early loss of primary molars.
• In patients with Class II division 1 malocclusion who have normal overbite or open bite tendency but minor mandibular incisor crowding and retrusion due to hyperactivity or dysfunction of the lower lip, a regular lip bumper cannot be applied because it can produce greater bite opening. In these patients, if it is necessary to release the incisors from lip pressure, the author recommends using the combination of a lip bumper and a lower holding arch, which will have the same effect on the mandibular incisors but prevent any changes in the molar area (Fig 11-3).
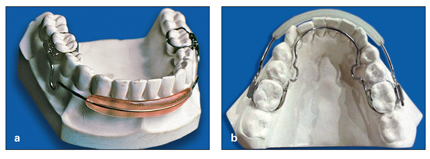
Fig 11-3 (a) Simple lip bumper. (b) Combination of lip bumper and lower holding arch for the HLH technique.
The lip bumper can achieve the following:
• Increase in arch length (distal molar movement; labial anterior movement)
• Disruption of the equilibrium between the perioral musculature and the tongue to increase arch width and promote alveolar growth
• Correction of the curve of Spee by uprighting the molars, proclining the anterior teeth, and facilitating eruption of the posterior segment
• Reduction of overjet by preventing lip muscle dysfunction and proclining the incisors
Strategy and Tactics of HLH Application
Application of triple appliances (HLH) with the proper modifications during the mixed dentition is a simple, effective way of achieving early Class II correction. Selection of the proper type of headgear, determination of the necessary design modifications for the Hawley appliance (such as anterior inclined surface, bite plane, or posterior occlusal coverage), and proper use of the lip bumper are critically important to the success of the HLH technique.
For early intervention in Class II division 1 malocclusion, the HLH approach may be applied as a two-phase or a one-phase treatment. For treatment of Class II division 2 malocclusion, the HLH technique has some differences in tactics, which are designed to address the specific characteristics of this anomaly.
Two-phase strategy for Class II division 1 malocclusion
Two-phase HLH application is used for management of Class II dental malocclusion or Class II malocclusion with minor A-B discrepancy. This tactic usually is started during the middle mixed dentition to establish normal permanent molar relationships, normal overjet, and normal overbite. After the interceptive HLH therapy has established Class I molar relationships, an interim phase continues until all permanent canines and premolars erupt. The interim phase can include use of a Hawley retainer or be limited to observation. Phase 2 takes place during the permanent dentition and involves minor final adjustment.
The advantage of early HLH intervention during the mixed dentition is the possibility for normal eruption of the canines and premolars with normal interdigitation that may not need any further treatment (see cases 11-1 and 11-2). In the two-phase approach, phase 1 (HLH treatment) usually takes 1 to 1.5 years; the interim phase of observation and guidance of eruption takes about 1 year; and phase 2 (final alignment) takes about 1 year. However, permanent canines and premolars may exhibit normal interdigitation after eruption, eliminating the need for phase 2. This prospect is based on the finding that, if Class I molar relationships are achieved, normal interdigitation of buccal segments will follow, as Poulton47 has shown. Canine and premolar tooth buds move distally and follow the root movement of the maxillary permanent first molars after they are distalized.
One-phase strategy for Class II division 1 malocclusion
The one-phase HLH treatment strategy is applied for correction of skeletal Class II malocclusions with moderate or severe A-B discrepancies, usually starting around the late mixed dentition or before the growth spurt (skeletal maturation assessment value of 4 to 7) and continuing until eruption of the permanent dentition (excluding third molars) is completed. It is a continuous treatment approach with no interim phase. The one-phase HLH treatment is followed by complete bonding for final tooth alignment. It usually takes about 2 to 2.5 continuous years of treatment from HLH to the end of comprehensive treatment.
The first step is establishment of normal permanent molar relationships combined with control of maxillomandibular discrepancy by controlling maxillary growth, promoting mandibular growth, or both. The second step starts with the bonding of premolars after they erupt and retraction, if needed, to establish normal interdigitation in the molar and premolar segments. The next step is canine alignment and retraction, which might be accompanied by Class II elastics. The final step is incisor retraction and final adjustment before retention. Depending on the severity of the skeletal jaw discrepancy, the use of headgear might be continued to the final stage of treatment, even after normal molar relationships are established, or to provide anchorage.
A significant advantage of this type of early intervention is that sagittal abnormalities, whether the result of maxillary protrusion, mandibular retrusion, or a combination, can be controlled with the HLH approach, while the vertical and transverse dimensions of the malocclusion can be controlled by taking advantage of the patient’s growth potential.
Strategy for Class II division 2 malocclusion
Early treatment of Class II division 2 malocclusions has some specific differences in tactics. The major characteristic of Class II division 2 malocclusions, besides Class II interdigitation, is deep bite and maxillary incisor crowding with severe retroclination of the maxillary central incisors. Therefore, the first steps in treatment are to control overbite with a thick anterior bite plate that will disarticulate the posterior dentition, encouraging eruption of those teeth, and to facilitate molar retraction with the cervical headgear. The next step is 2 × 4 maxillary bracketing to achieve anterior alignment and some proclination of the central incisors. This measure will facilitate mandibular growth and allow for accelerated dentoalveolar development that might have been restricted by locked occlusion caused by maxillary incisor retroclination and deep bite.
In the next step, after some overbite reduction, a lip bumper is applied if the mandibular incisors are also crowded and retroclined; later, this is followed by mandibular incisor bonding.
One important goal of early intervention in Class II division 2 malocclusion is to control the child’s overbite at an early age by taking advantage of the patient’s growth; this type of treatment is very difficult to manage later.
Case Reports
The following case reports present examples of early treatment with the HLH procedure, applied in either one phase or two phases of treatment.
Case 11-1: Two-phase interceptive treatment and observation
A 10-year, 5-month-old girl in the late mixed dentition had a Class II division 1 malocclusion, a 9.2-mm overjet, and deep overbite. The maxillary incisors had normal inclination, the mandibular incisors were slightly uprighted, and she had a large A-B discrepancy (point A–nasion–point B [ANB] angle = 7.4 degrees) resulting from mandibular retrognathia (Figs 11-4a to 11-4d).
Treatment:
The treatment plan was use of the HLH technique alone: cervical headgear, a maxillary modified Hawley appliance with anterior inclined surface, and a mandibular lip bumper. Treatment resulted in significant changes in the patient’s occlusion, soft tissue profile, and molar relationships (Figs 11-4e to 11-4j). The A-B discrepancy (ANB) was reduced from 7.4 to 0.8 degrees and overjet from 9.2 to 2.9 mm.
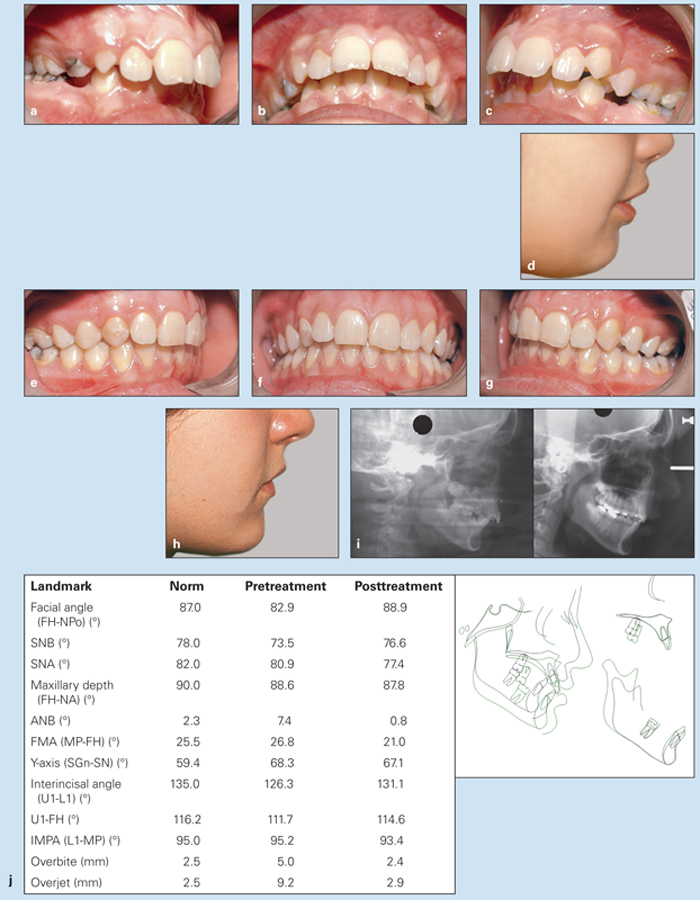
Fig 11-4 Management of severe overjet and deep overbite in a 10-year, 5-month-old girl in the late mixed dentition. She was treated only with the HLH technique. (a to c) Pretreatment occlusion. (d) Pretreatment soft tissue profile. (e to g) Posttreatment occlusion. (h) Posttreatment soft tissue profile. (i) Pretreatment (left) and posttreatment (right) cephalometric radiographs. (j) Changes in cephalometric measurements and superimposition of pretreatment (black) and posttreatment (green) tracings.
Case 11-2: Two-phase interceptive treatment and observation
A 9-year-old girl had a Class II division 1 malocclusion, minor overbite, a 7.9-mm overjet, a steep mandibular plane, and a slight open bite tendency (Figs 11-5a to 11-5d). Maxillary incisor protrusion had caused lip incompetence, but the mandibular dentition was good.
Treatment:
Treatment involved only the application of the HLH technique (combination headgear) with one stage of active treatment and a second stage of observation. Instead of a lip bumper, a lower holding arch was used to preserve leeway space and prevent molar eruption. A maxillary Hawley appliance was used for maxillary incisor retraction, and the headgear also aided maxillary retraction. Figures 11-5e to 11-5j show the results of treatment.

Fig 11-5 Management of minor overbite and severe overjet in a 9-year-old girl with a Class II division 1 malocclusion. (a to c) Pretreatment occlusion. (d) Pretreatment soft tissue profile. (e to g) Posttreatment occlusion. (h) Posttreatment soft tissue profile.
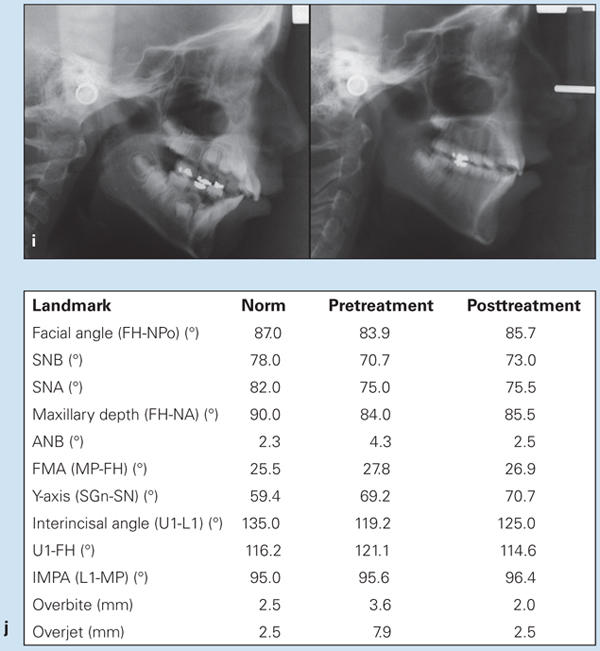
Fig 11-5 (cont) (i) Pretreatment (left) and posttreatment (right) cephalometric radiographs. (j) Changes in cephalometric measurements.
Case 11-3: Two-phase interceptive treatment and observation
A 9-year-old girl presented with a Class II division 1 malocclusion, a 7.6-mm overjet, an A-B discrepancy of 7.1 degrees, impinging deep bite, and mandibular retrognathism caused by clockwise rotation (Figs 11-6a to 11-6c).
Treatment:
This patient was treated with a two-phase active HLH procedure, including combination headgear for retraction of the maxillary first molar while controlling extrusion, and a combination lip bumper and lower holding arch (see Fig 11-3b) was used to control uprighting of the mandibular molars while preventing lip dysfunction. After Class I molar relationships were achieved, a Hawley retainer was placed during the interim phase (at first 24 hours a day and then 12 hours’ use at night) until the canines and premolars had erupted (Figs 11-6d to 11-6f). Figures 11-6g and 11-6h show the pre- and posttretment cephalometric radiographs, superimposition of tracings, and measurements.

Fig 11-6 Management of severe overjet, impinging deep bite, and mandibular retrognathism in a 9-year-old girl. (a to c) Pretreatment occlusion. (d to f) Posttreatment occlusion.
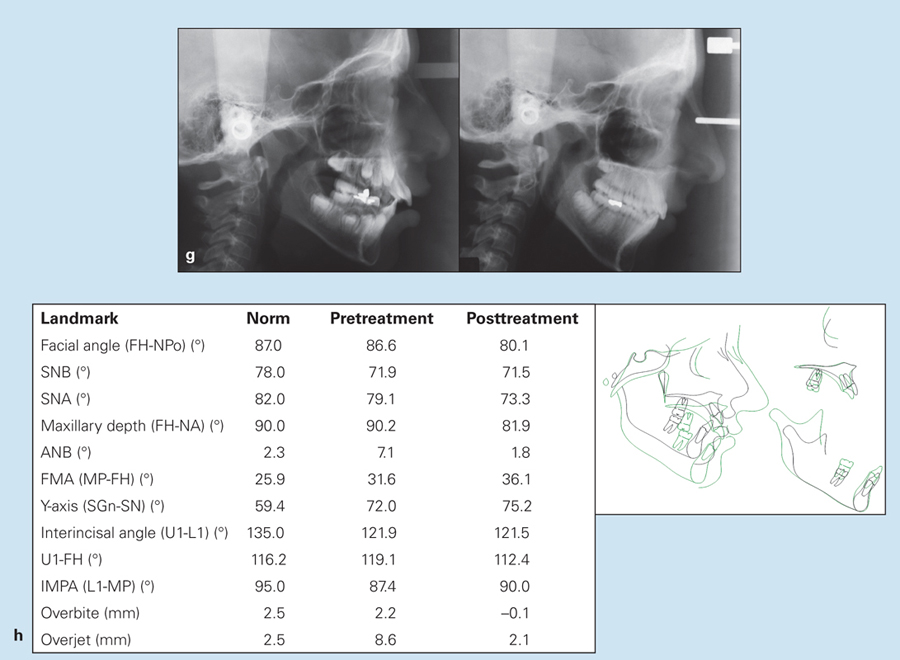
Fig 11-6 (cont) (g) Pretreatment (left) and posttreatment (right) cephalometric radiographs. (h) Changes in cephalometric measurements and superimposition of pretreatment (black) and posttreatment (green) tracings.
Case 11-4: Two-phase treatment with HLH and comprehensive treatment
A 9-year, 7-month-old girl in the middle mixed dentition presented with a Class II division 1 malocclusion, an 11-mm overjet, and severe overbite that had resulted in a collapsed mandibular dentition and retrognathia (retrognathic chin). Here lips were apart, and lip dysfunction continued to worsen the irregularities (Figs 11-7a to 11-7d).
Treatment:
The treatment approach was designed as two-phase HLH treatment. In phase 1, cervical headgear was used to retract the maxillary molars and reduce overbite; an inclined maxillary Hawley appliance was used to stimulate mandibular growth by unlocking the collapsed mandible, helping forward mandibular growth; a lip bumper was used to control lip dysfunction and alleviate the lip force directed at the mandibular incisors, thereby correcting mandibular incisor retroclination, uprighting mandibular molars, and correcting the curve of Spee. Figure 11-7e illustrates the maxillary dentition and spontaneous distal movement of the buccal segments achieved by cervical headgear and good compliance. Phase 2 was started after complete eruption of the canines and premolars. Use of the headgear was stopped, and maxillary Nance anchorage was placed. Figures 11-7f to 11-7k show the posttreatment results, which included correction of the Class II malocclusion, correction of the severe overjet (reduction from 11.0 to 1.9 mm), correction of the deep bite (4.6 to 0.8 mm), reduction in the ANB angle from 6.2 to 2.7 degrees, and a change in the retrognathic chin from 82.5 to 85.9.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



