In the United States, motor vehicle collisions are the most prevalent cause of soft tissue damage to the face. More than 146,000 patients annually require hospital attention for facial soft tissue trauma. Soft tissue injuries to the face and neck can be one of the most challenging problems presented to the facial surgeon. The patient’s self-esteem may be compromised temporarily or permanently. The goal of treatment is to achieve a functional and aesthetic restoration without infection. Outcomes of these injuries are often dependent on timely diagnosis and repair.
INITIAL EVALUATION AND EARLY MANAGEMENT
Early diagnosis and definitive treatment are important when dealing with soft tissue injuries. A correct diagnostic assessment followed by a suitable therapeutic plan can reduce cosmetic and functional defects to a minimum. Life-threatening injuries are addressed initially followed by a complete evaluation. Obstruction of the airway and active bleeding should be corrected first. During the initial assessment it is important to determine the mechanism and time of injury. This information can be helpful during later exploration and debridement of wounds and the prediction of subsequent soft tissue healing.
Proper handling of soft tissue in the acute phase demands proper attention to principles of wound evaluation, preparation, and repair. Immediate wound care involves appropriate hemostasis and anesthesia. Most bleeding can be controlled with pressure dressings. In rare cases vessels may need to be ligated, but it is important to avoid indiscriminate clamping inside the wound because this may damage important structures. Scalp lacerations may require ligation and in some instances can result in a hemodynamic shock state secondary to blood loss.
Soft tissue injuries not involving the face require early treatment because secondary risk of infection increases with time. Ideally facial soft tissue injuries are treated as soon after the injury as possible, preferably within the first 8 hours. Because of the rich vascularity of the face there is, however, no “golden period” for suture repair. Facial soft tissue injuries are routinely closed primarily even if the injury took place many hours before treatment. Wounds that are older should be thoroughly cleansed and their margins freshened before closure.
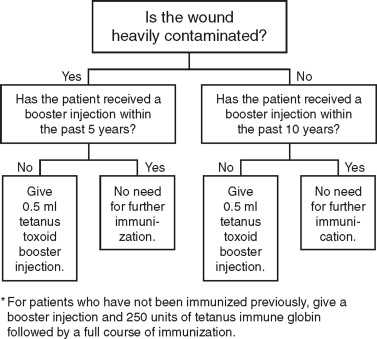
It is important to document tetanus immunization status. In wounds that are relatively clean (non–tetanus-prone), a booster injection within the past 10 years is sufficient. For heavily contaminated wounds (tetanus-prone) in patients without a booster injection within 5 years before the injury, a 0.5-mL tetanus toxoid boost injection should be given. Patients who have not received a booster within 10 years should receive a booster injection for any wound. For patients who are not immunized, they should receive both a booster injection and 250 units of tetanus immune globulin, followed by a full course of immunization ( Figure 17-1 ).
Once the patient is stabilized a decision must be made regarding the sequence of repair and whether to transfer the patient to the operating room for closure of the lacerations. In injuries that involve deep structures a general anesthetic affords the best opportunity for exploration and repair.
ANATOMIC CONSIDERATIONS
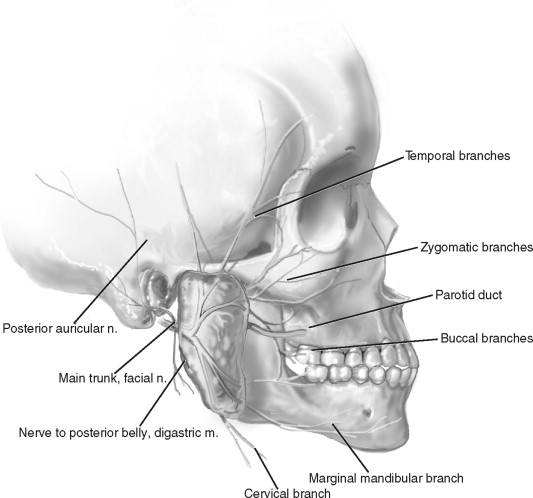
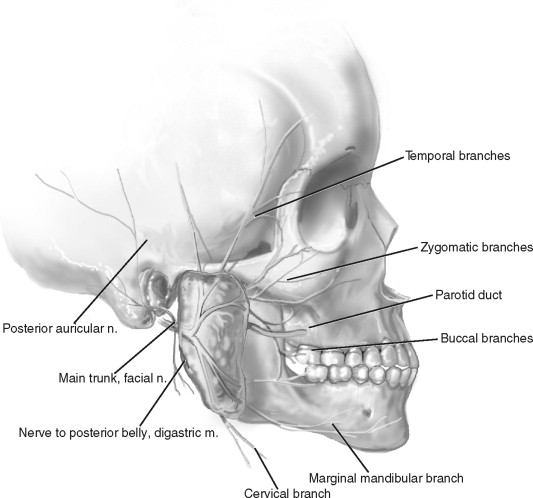
Facial injuries may extend to involve adjacent structures including nerves, ducts, blood vessels, and glands. Associated injuries including fractures of the facial skeleton should be identified. The facial nerve is an important anatomic structure to evaluate and document. The facial nerve exits the stylomastoid foramen and courses through the parotid gland, dividing it into deep and superficial portions ( Figure 17-2 ). The facial nerve divides into five branches within the gland. Various grading systems are available, including the House Brackmann score, for evaluating and documenting facial nerve deficits ( Table 17-1 ).
| Grade | Facial Movement | |
|---|---|---|
| I. | Normal | Normal facial function |
| II. | Mild dysfunction | Moderate-to-good function of forehead; complete closure of eye |
| III. | Moderate dysfunction |
|
| IV. | Moderately severe dysfunction |
|
| V. | Severe dysfunction |
|
| VI. | Total paralysis | No movement |
The parotid duct exits the gland, runs along the superficial surface of the masseter muscle, and penetrates the buccinator muscle to enter the oral cavity opposite the upper second molar. The parotid duct can be divided into three regions. The first region is the proximal portion of the duct where it emerges from the parotid gland. The middle region of the duct lies directly over the masseter muscle. In this location the duct is relatively straight and unprotected by overlying structures. This is the most common site of injury and the easiest to repair. The distal region refers to the portion of the duct anterior to the masseter muscle. The duct dives into the buccinator muscle and exits into the mouth adjacent to the maxillary second molar.
Other important anatomic landmarks to consider include the gray line of the eyelids, the vermilion border of the lips, and the alae of the nose. It is important to identify these landmarks in order to correctly reapproximate these areas.
ANATOMIC CONSIDERATIONS
Facial injuries may extend to involve adjacent structures including nerves, ducts, blood vessels, and glands. Associated injuries including fractures of the facial skeleton should be identified. The facial nerve is an important anatomic structure to evaluate and document. The facial nerve exits the stylomastoid foramen and courses through the parotid gland, dividing it into deep and superficial portions ( Figure 17-2 ). The facial nerve divides into five branches within the gland. Various grading systems are available, including the House Brackmann score, for evaluating and documenting facial nerve deficits ( Table 17-1 ).
| Grade | Facial Movement | |
|---|---|---|
| I. | Normal | Normal facial function |
| II. | Mild dysfunction | Moderate-to-good function of forehead; complete closure of eye |
| III. | Moderate dysfunction |
|
| IV. | Moderately severe dysfunction |
|
| V. | Severe dysfunction |
|
| VI. | Total paralysis | No movement |
The parotid duct exits the gland, runs along the superficial surface of the masseter muscle, and penetrates the buccinator muscle to enter the oral cavity opposite the upper second molar. The parotid duct can be divided into three regions. The first region is the proximal portion of the duct where it emerges from the parotid gland. The middle region of the duct lies directly over the masseter muscle. In this location the duct is relatively straight and unprotected by overlying structures. This is the most common site of injury and the easiest to repair. The distal region refers to the portion of the duct anterior to the masseter muscle. The duct dives into the buccinator muscle and exits into the mouth adjacent to the maxillary second molar.
Other important anatomic landmarks to consider include the gray line of the eyelids, the vermilion border of the lips, and the alae of the nose. It is important to identify these landmarks in order to correctly reapproximate these areas.
MANAGEMENT OF SOFT TISSUE WOUNDS
Once the patient has been stabilized the treatment of the soft tissue injuries is undertaken. Proper lighting is required to identify foreign bodies and injuries to vital structures.
Repair of soft tissue trauma is performed as soon as the patient’s condition allows. Local anesthetics or regional nerve blocks are given to reduce pain. A local anesthetic with vasoconstrictor may be useful in controlling bleeding. Hair present at the margins of a laceration can be cut, except in the area of the eyebrows because permanent alopecia may result.
Local anesthetic is injected before cleaning the wound, which allows more effective preparation. Lidocaine is a commonly used anesthetic, ranging in strength from 0.5% to 2%, and is usually given with 1 : 100,000 epinephrine. Local anesthetics containing epinephrine have been used successfully in all areas of the face but may not be optimal in areas where tissue monitoring is critical. Care should be taken to avoid disrupting important landmarks when injecting local anesthetic. Regional nerve blocks are helpful to avoid this disruption in areas where alignment of anatomic landmarks is critical. Topical anesthetics—such as a solution containing 0.5% tetracaine, 1 : 2000 adrenaline, and 11.8% cocaine (TAC)—may be helpful for some superficial wounds. Benefits of anesthetics include avoidance of pain at the injection site, better patient cooperation, and the absence of tissue distortion.
Facial wounds are often contaminated with bacteria and foreign material. Treatment is aimed at minimizing the bacterial wound flora and removing any foreign bodies. Copious irrigation with normal saline or other solution is undertaken. Pressure irrigation of the wound with saline reduces bacterial contamination. Pulse irrigation of contaminated wounds is used to dislodge foreign bodies and decrease the bacterial load of the tissues. Devitalized tissue is removed to prevent postoperative infection. Decontamination is more important than the use of antibiotics. Hydrogen peroxide impedes wound healing and is minimally bactericidal even when diluted to 1 : 100. Soft tissue cleaning and debridement are important, especially in wounds in which contamination may be a problem, including bites. A scrub brush and detergent soap may be necessary to remove deeply imbedded foreign material. Inadequate debridement may result in “tattooing” of the skin, which is difficult to treat secondarily.
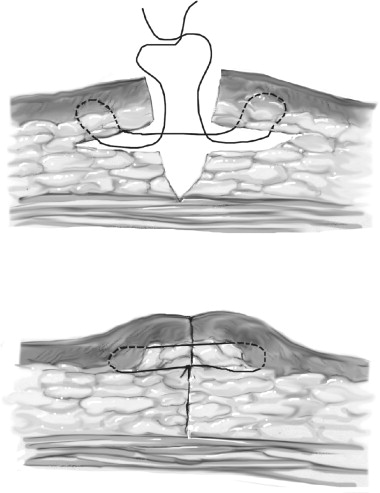
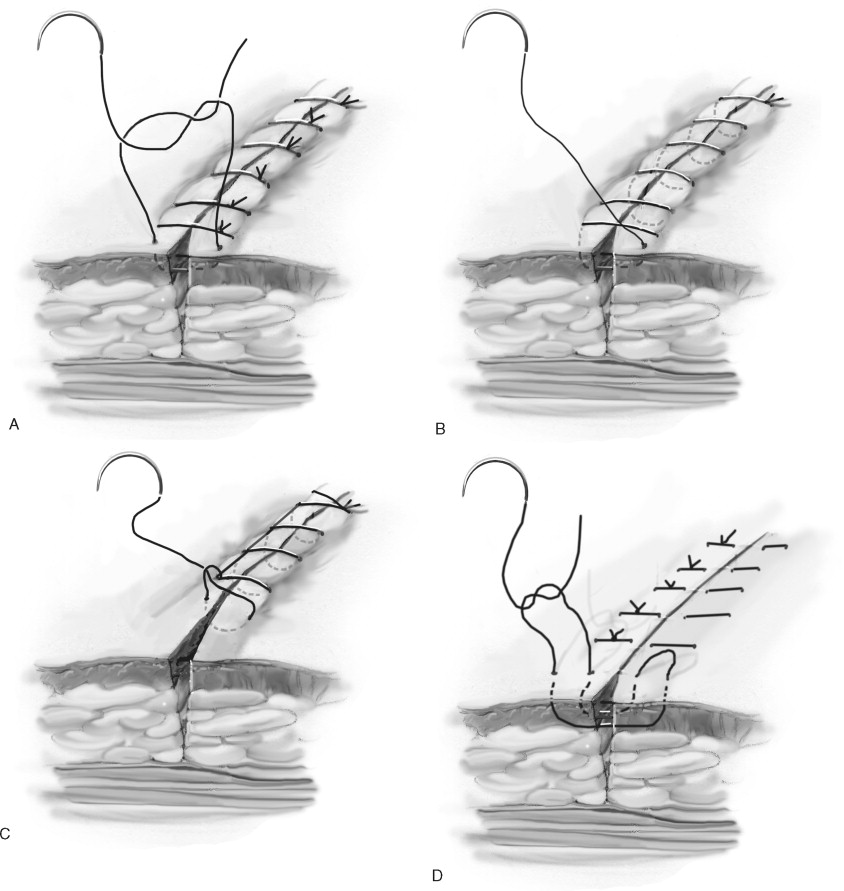
Closure of the wound usually will require a layered approach to minimize dead space and avoid significant tension at the skin edges. Techniques for closing wounds include suturing, applying adhesives, and stapling. For complex lacerations, sutures provide the best aesthetic results. Slight eversion of the wound edge should be performed ( Figure 17-3 ). Various types of suture techniques are available including simple interrupted, running, subcuticular, mattress, and locking ( Figure 17-4 ).

Suture material should be chosen based on the characteristics required for a specific wound, including condition of the wound, the strength of the suture, and the reaction of the surrounding tissues to the suture material. A variety of suture materials are available ( Table 17-2 ). Types of sutures include absorbable or nonabsorbable, coated or uncoated, natural or synthetic, and multifilament or monofilament. Synthetic sutures include nylon (Ethilon and Dermalon), polypropylene (Prolene and Surgilene), and Dacron (Mersilene, Tevdek, Polydek, Ethibond, and Ti-Cron). Natural, nonabsorbable sutures include silk, cotton, and metals. Natural absorbable sutures are made of catgut, chromic, and plain collagen. Synthetic, absorbable sutures include polyglycolic acid (Dexon), polyglactin 910 (Vicryl), and polydioxanone (PDS). The primary purpose for sutures is to approximate wound margins and enhance tissue healing. Wounds never regain more than 80% of the strength of intact skin.
| Suture | Types | Raw Material | Tensile Strength Retention in Vivo | Absorption Rate | Tissue Reaction | Contraindications | Frequent Uses |
|---|---|---|---|---|---|---|---|
| ABSORBABLE SUTURES | |||||||
| Surgical gut suture | Plain | Collagen derived from healthy beef and sheep | Individual patient characteristics can affect rate of tensile strength loss. | Absorbed by proteolytic enzymatic digestive process | Moderate reaction |
|
General soft tissue approximation and/or ligation |
| Fast absorbable surgical gut | Plain | Collagen derived from healthy beef and sheep | Nearly all of its original strength is lost within 7 days. | Completely absorbed by 21-42 days | Moderate reaction |
|
Intended for dermal (slow) use only |
| Surgical gut suture | Chronic | Collagen derived from healthy beef and sheep | Individual patient characteristics can affect rate of tensile strength loss. | Absorbed by proteolytic enzymatic digestive process | Moderate reaction |
|
General soft tissue approximation and/or ligation, including oral surgery |
| Coated Vicryl * Raplde (polyglactin 910) suture | Braided | Copolymer of lactide and glycolide coated with polyglactin 370 and calcium stearate | Approximately 50% remains at 5 days. All tensile strength is lost at approximately 14 days. |
|
Minimal to moderate acute inflammatory reaction | Should not be used where extended approximation of tissue under stress required or where wound support beyond 7 days required | Superficial soft tissue approximation of skin and mucosa only |
| Monocryl * (poliglecaprone 25) suture | Monofilament | Copolymer of glycolide and epsilon-caprolactone |
|
|
Minimal acute inflammatory reaction |
|
General soft tissue approximation and/or ligation |
| Coated Vicryl * (polyglactin 910) suture |
|
Copolymer of lactide and glycolide coated with polyglactin 370 and calcium stearate |
|
|
Minimal acute inflammatory reaction | Being absorbable, should not be used where extended approximation of tissue required | General soft tissue approximation and/or ligation |
| PDS * II (polydioxanone) suture | |||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


