Since the advent and the popularization of orthognathic surgical procedures in correcting dentofacial deformities, the analysis of the facial soft tissue and the associated esthetic outcome has probably been and still is the most challenging and unsatisfactory component in the global orthodontic-surgical treatment planning process. The need for an ideal procedure capable of assessing accurately the final three-dimensional (3D) configuration of the facial envelope is crucial in a surgery in which the final goals are to improve the esthetic facial appearance and to establish a functional and stable occlusion. Soft-tissue profile changes related to the skeletal maxillary and/or mandibular movements is classically elaborated and adjusted over the underlying bone using previously reported cephalometric ratios of soft to bone tissue movements, which are based on mean values of responses and on a simple correlation of one variable with another or using linear regression equations. Moreover, ratios have been calculated from linear changes limited to specific two-dimensional cephalometric landmarks in the midsagittal plane. This method is restrictive, and its accuracy and reliability in predicting realistic profile changes are questionable. In fact, the main disadvantage of such an approach is that it does not take into account the more complex geometric 3D interactions of highly variable individual parameters (e.g., soft-tissue tension, thickness, length and redistribution, muscle strain, posture and tonus, postoperative edema, growth) and technical parameters (e.g., type of osseous fixation, surgeon’s expertise and skill, postoperative edema, skeletal long-term stability and relapse, soft-tissue closure). The following methods for the prediction of facial soft-tissue outcomes have been described in the literature and are separately reviewed in this chapter:
- •
The lateral cephalometric “line drawing” tracing prediction (manual and computer-assisted)
- •
The photographic prediction
- •
The computerized video imaging (videocephalometric) prediction
- •
The 3D computer-assisted prediction
LATERAL CEPHALOMETRIC “LINE DRAWING” TRACING PREDICTION (MANUAL AND COMPUTER-ASSISTED)
The cephalometric soft-tissue analysis for planning orthodontic treatment was reported as early as the 1930s and rapidly became an excellent and irreplaceable tool also in the treatment planning process for patients who required orthognathic surgery. The literature is replete with reports describing different, more or less accurate methods of cephalometric analysis, planning and predicting surgical soft-tissue outcomes based on specific landmark repositioning in response to determined skeletal movements, which allow quantification, classification, and communication of patient data.
Three cephalometric methods are commonly used: (1) the “cut-and-paste” hand planning technique, which involves manual cutting, moving, and repositioning of cephalometric acetate tracings to obtain the desired esthetic profile as well as a Class I occlusal relationship ; (2) the computer-assisted technique, which generates soft-tissue prediction profile tracings by using software for digitizing the lateral cephalometric radiograph ; and (3) the computer-assisted video imaging technique, which integrates video images with the patient’s lateral cephalogram tracing, allowing a two-dimensional image simulation of the suitable soft-tissue profile outcome. This last technique is discussed separately in a further specific paragraph. In all three techniques the soft-tissue profile is adjusted and changes are planned according to previously reported soft-tissue to bone-tissue ratios. Factors influencing accuracy of such a prediction tracing include comprehension of profile planning, accuracy of surgery, methods of fixation, degree of soft-tissue stripping, degree of relapse, accuracy and reproducibility of tracings, soft-to-hard tissue ratio, reliability of cephalometrics and of photography, limitation of profile planning, anteroposterior planning, and variation of lip morphology and posture. Authors comparing the accuracy and predictability of the manual versus computed technique have found quite similar values in mandibular advancement planning results, with only a few points differing between prediction and outcomes of cephalometric tracings. On the other hand, the hand technique has been found more accurate in the maxillary and bimaxillary prediction of soft-tissue changes, particularly in the lip area. This can be explained by the limited number of soft-tissue points provided by the software programs, which are probably insufficient to closely reproduce such complex regions. Conversely, the freedom of artistic license allowed by the hand technique results in a more accurate prediction tracing.
Historically the first studies on soft-tissue changes after orthognathic surgery were conducted on the modifications occurring in the lower lip and chin after mandibular reduction procedures, as early as the late 1950s. Conversely, it was not until mid 1970s that the first reports on soft-tissue changes associated with maxillary surgery (advancement, intrusion, retrusion, or bimaxillary) were published.
Cephalometric studies reporting profile soft-tissue changes and related soft- to bone-tissue ratios are reviewed and analyzed separately depending on the specific surgical orthognathic procedure.
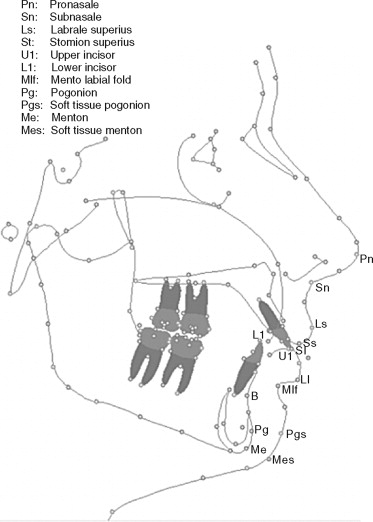
The hard- and soft-tissue cephalometric landmark points are depicted in Figure 17-1 .
MANDIBULAR SURGERY
The lower lip, the mentolabial fold (Mlf), and the neck-chin angle are the anatomic regions most strongly influenced by the anterior or posterior surgical repositioning of the mandible.
Mandibular Advancement
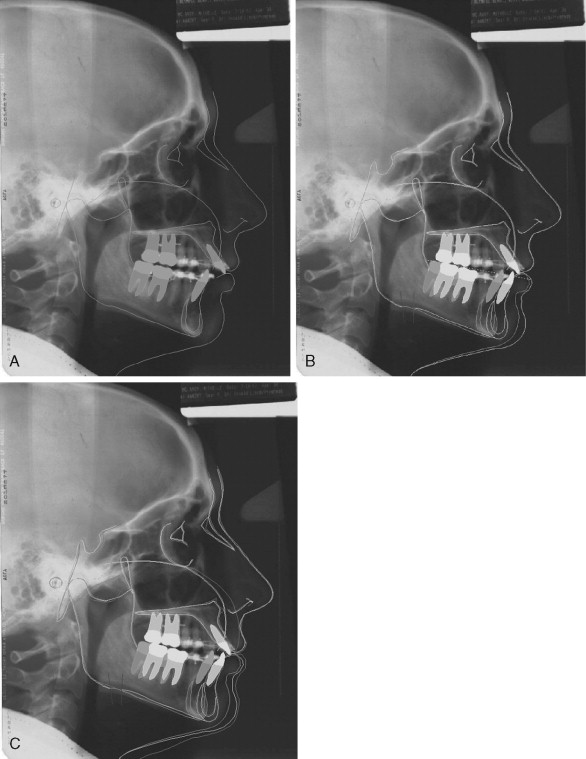
The main changes affect the lower lip, with a global reduction in thickness, lengthening, and straightening, as well as the chin area, with a decrease in the lower labial sulcus or mentolabial fold depth, whereas changes on the upper lip (minor anterior movement) are usually negligible, temporary, and limited to only patients with Class II deep-bite deformities ( Figure 17-2 ). The lower lip also presents the most variable soft- to bone-tissue ratios (Li : L1), ranging from 0.38 : 1 to 0.80 : 1, contrary to the chin ratios (Mlf : B and Pg′ : Pg), which are almost invariably in a 1 : 1 relationship, probably because of the tight attachment of the mental soft tissue to the underlying skeletal bases.
Mandibular Setback
The lower lip has been found to become more everted and shorter, with a closure of the mentolabial fold, whereas the upper lip can sometimes be displaced posteriorly with a discrete opening of the nasolabial angle. The Li : L1 ratio was around 0.6 : 1, and in the chin region Pg′ followed Pg and the B point in an almost 1 : 1 ratio. These ratios have been constantly found in several studies regardless of the magnitude of the setback movement.
Genioplasty
The most unpredictable points when a genioplasty is planned are the superior and inferior vermilion, as well as Pg′ and Me′.
MAXILLARY SURGERY
Soft-tissue changes related to maxillary surgery have proven to be relatively more predictable than in mandibular surgery, regardless of the type and the amount of skeletal movement produced. The nasolabial angle and the upper lip are the anatomic regions most strongly influenced by anterior or posterior surgical repositioning of the mandible.
Total Maxillary Advancement
The main changes induced by total maxillary advancement are located in the nasal region and the upper lip. The vermilion border of the upper lip (Ls) typically advances horizontally with a rotational and translational movement around the subnasale, following the upper incisor (U1) in soft- to bone-tissue ratios ranging from 0.33 : 1 to 0.9 : 1. The latter high value has been reported only by one group who employed a V-Y technique for the closure of the maxillary vestibular incision, which prevented the thinning and shortening of the upper lip invariably associated with maxillary advancements. The thinning of the upper lip may result in the loss of the visible vermilion border, which is esthetically undesirable. On the other hand, vertical changes in the upper lip related to the horizontal movement of U1 are too variable to be correctly predicted in a ratio. The nasal effects imply a decreasing of the nasolabial angle, widening of the alar bases (which can be limited by using the alar base cinch suture procedure), deepening of the supratip break, and nasal tip elevation (1 mm for every 6 mm of superior movement of U1). In some patients the tip elevation may produce quite esthetic changes, such as the disappearance of the nasal hump that usually accompanies maxillary advancement or impaction.
Total Maxillary Intrusion
Surgical repositioning of the maxilla mainly affects the morphology of the nose and upper lip in both vertical and horizontal dimensions. *
* , , , , , .
The decrease in the amount of the visible vermilion due to an inward rolling of the upper lip, a downturning of the corners of the mouth, and a widening of the alar base of the nose are the main undesirable esthetic effects associated with the decrease of the face height resulting from this procedure. Some authors have clinically observed that probably such changes are mainly related to postoperative muscular reorientation of the oronasal area rather than to the amount of skeletal movement. The ratios of vertical shortening in the upper lip related to the superior impaction of the maxilla have been reported to range from 0.2 : 1 to 0.4 : 1 by authors who did not perform an anatomic reorientation of the facial muscles around the oronasal area. Conversely, it was shown that when a functional orientation of the musculature is accomplished (V-Y closure of maxillary vestibular incision and alar base cinch suture), the postsurgical lip closely approaches its preoperative morphology, presenting only a minimal and negligible shortening (10%). This finding is of capital importance in planning and predicting the final suitable vertical maxillary impaction and the resultant lip-to-tooth relationship. After the posterior maxillary intrusion, the soft-tissue chin (Mlf and Pg′) has been found to autorotate on the same arc as the bony chin in a 1 : 1 ratio, with the Mlf angle unfolded from the inferior labial sulcus.
Maxillary Retrusion
The upper lip and the nasal soft tissues closely follow the skeletal movements posteriorly. As observed in advancement and intrusion cases, there is also a widening of the alar bases, with a tendency for the tip of the nose to rotate downward, with a resulting opening of the nasolabial angle. This may in some patients result in a parrot’s beak nasal appearance. The same deformity can also be found after inferior repositioning of the maxilla and downgraft. There is also a tendency for the upper lip to thicken following the maxillary posterior movement.
BIMAXILLARY SURGERY
Different studies have confirmed that the soft-tissue response associated with double-jaw surgery is similar to those found in single-jaw procedures, with the exception of the nasolabial angle and vertical movement of the lower lip and chin.
PHOTOGRAPHIC PREDICTION
First described by Henderson in 1974, the photographic soft-tissue profile planning technique has been progressively abandoned owing to the difficulty in correctly obtaining a satisfactory superimposition of an enlarged photograph on the cephalometric radiograph. This technique involves the following steps: the production of a lateral cephalometric tracing, the production of a transparent positive profile photograph enlarged to a 1 : 1 size corresponding to the size of the cephalogram, superimposition of the photograph on the cephalometric tracing, sectioning of the photograph along the predicted osteotomy lines, and manipulation until the desired esthetic profile as well as a Class I occlusion relationship are obtained. One of the greatest concerns with this technique is that the photograph has to be enlarged in order to perfectly match the lateral cephalometric tracing, with the possibility of some degree of distortion of important profile’s landmarks, which can affect the final accuracy of the prediction. Moreover, it has been shown that it is very difficult to take a photograph with a head’s posture that closely corresponds to the position of the head in a cephalogram, unless the photo is taken in a cephalostat at the same time as the cephalogram is taken.
A variation of this method has been proposed by Kinnebrew and colleagues as follows: production of a cephalometric tracing; projection of a 35-mm slide on the cephalometric tracing, which is sized to the profile soft-tissue silhouette; production of a composite tracing with facial and dental features; production of a “want list” image of desired changes; and superimposition of the last image on the pretreatment image, which indicates the soft-tissue change and thus dictates the specific bony changes based on the available soft- to hard-tissue ratios. Other episodic photographic prediction studies involve the use of photocephalometric techniques or Moiré stereophotogrammetry.
PHOTOGRAPHIC PREDICTION
First described by Henderson in 1974, the photographic soft-tissue profile planning technique has been progressively abandoned owing to the difficulty in correctly obtaining a satisfactory superimposition of an enlarged photograph on the cephalometric radiograph. This technique involves the following steps: the production of a lateral cephalometric tracing, the production of a transparent positive profile photograph enlarged to a 1 : 1 size corresponding to the size of the cephalogram, superimposition of the photograph on the cephalometric tracing, sectioning of the photograph along the predicted osteotomy lines, and manipulation until the desired esthetic profile as well as a Class I occlusion relationship are obtained. One of the greatest concerns with this technique is that the photograph has to be enlarged in order to perfectly match the lateral cephalometric tracing, with the possibility of some degree of distortion of important profile’s landmarks, which can affect the final accuracy of the prediction. Moreover, it has been shown that it is very difficult to take a photograph with a head’s posture that closely corresponds to the position of the head in a cephalogram, unless the photo is taken in a cephalostat at the same time as the cephalogram is taken.
A variation of this method has been proposed by Kinnebrew and colleagues as follows: production of a cephalometric tracing; projection of a 35-mm slide on the cephalometric tracing, which is sized to the profile soft-tissue silhouette; production of a composite tracing with facial and dental features; production of a “want list” image of desired changes; and superimposition of the last image on the pretreatment image, which indicates the soft-tissue change and thus dictates the specific bony changes based on the available soft- to hard-tissue ratios. Other episodic photographic prediction studies involve the use of photocephalometric techniques or Moiré stereophotogrammetry.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


