In this case report, we introduce the combined use of multiloop edgewise archwire and microimplant anchorage to treat an 18-year-old Chinese woman who had a severe anterior open bite and a retrusive chin. Her diagnosis included a skeletal Class II base with severe anterior open bite, backward rotated mandible, and mesially tipped buccal dentition. The treatment plan emphasized vertical control of the posterior dentoalveolar dimension. Microimplant anchors were placed in the mandibular buccal segment to provide rigid anchorage and deliver intruding forces to the posterior teeth; a multiloop edgewise archwire was applied to generate uprighting forces to the maxillary and mandibular posterior teeth. Intrusion and uprighting of the posterior teeth contributed to the counterclockwise rotation of the mandibular plane, which consequently contributed to the facial profile improvement. Orthognathic genioplasty was implemented to further improve the chin prominence. After 1.5 years of retention, ideal intercuspation was evident, and the improved facial contour was stable.
Highlights
- •
Severe skeletal open bite is corrected by combined use of MEAW and mini-screw mechanism.
- •
Vertical dimension control is critical to achieve favorable rotation of the mandibular plane.
- •
Genioplasty intervention is implemented to further improve chin prominence.
In this case report, we introduce the combined use of multiloop edgewise archwire (MEAW) and microimplant anchorage (MIA) to treat an 18-year-old Chinese woman with a severe anterior open bite and a retrusive chin. The patient had a skeletal Class II base with severe anterior open bite, backward rotated mandible, and mesially tipped buccal dentition. The treatment plan was designed with an emphasis on vertical control of the posterior dentoalveolar dimension. The MIA placed in the mandibular buccal segment provided rigid anchorage and delivered intruding forces to the posterior teeth; the MEAW was applied to generate uprighting forces to both the maxillary and mandibular posterior teeth. Intrusion and uprighting of the posterior teeth contributed to the counterclockwise rotation of the mandibular plane, which consequently contributed to the facial profile improvement. Orthognathic genioplasty was implemented to further improve the chin prominence. After 1.5 years of retention, ideal intercuspation was evident, and the improved facial contour was stable. The mechanism and efficacy of MIA combined with MEAW in treating patients with skeletal Class II open bite are discussed.
Skeletal Class II malocclusion with severe anterior open bite is one of the most difficult malocclusions to treat orthodontically because it is often caused by clockwise rotation of the mandible or excessive growth in the vertical dimensions in the buccal segments.
In Chinese people, a skeletal open bite is often accompanied by a retrusive and undersized chin and a clockwise-rotated mandible, leading to a facial profile with marked convexity and excessive lower facial height. In adults, the most effective treatment of skeletal open bite is surgical repositioning of the maxilla or both jaws. However, surgical invasiveness and economic cost considerations are greater than for orthodontic treatment alone, which is cause for rejection by many patients and their families.
The MEAW technique has been found to be effective in treating patients with open-bite malocclusions. The treatment mechanism is mainly uprighting of the posterior teeth and partial extrusion of the anterior teeth, with limited effects in posterior intrusion.
Recently, the use of MIA for anterior open-bite correction by intruding the buccal segment has been reported. Intrusion of the molars enables counterclockwise rotation of the mandible, thus correcting the open bite and improving the facial profile of patients with skeletal Class II open bite. In this case report, we introduce the combined use of MEAW and MIA, aiming to correct a severe skeletal open bite by simultaneous uprighting and intruding of the buccal segment.
Diagnosis and etiology
The patient was an 18-year-old woman with chief complaints of frontal open bite and chin retrusion. She admitted to a habit of tongue thrusting and could not achieve lip closure at rest.
A convex profile due to a retrognathic mandible was noted. A shallow labiomental fold, an increased lower facial height, and circumoral musculature strain on lip closure were observed. The patient had an Angle Class I molar relationship with a severe anterior open bite up to 7 mm and moderate crowding in both the maxillary and mandibular dentitions ( Figs 1 and 2 ).
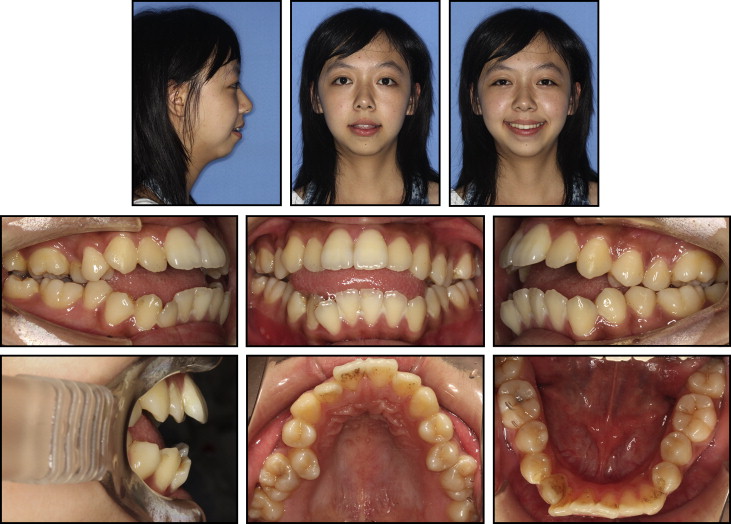
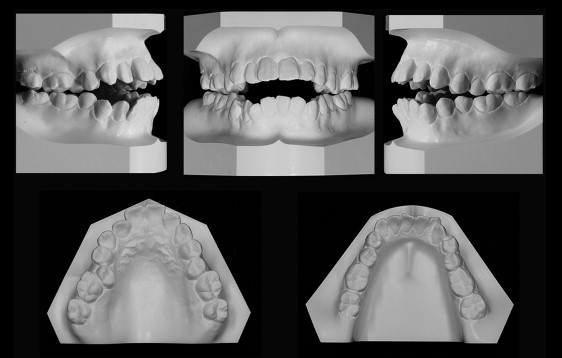
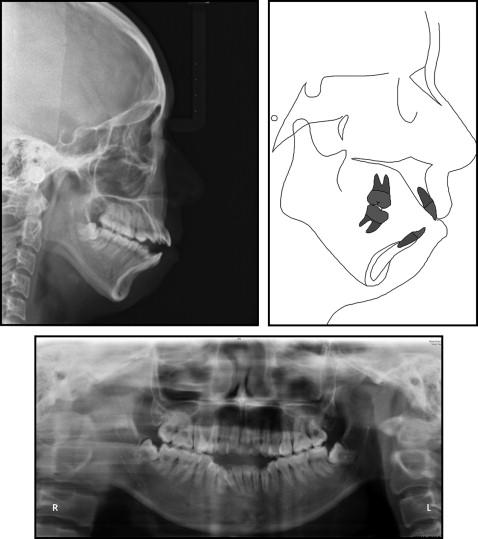
The lateral cephalometric analysis showed a skeletal Class II jaw relationship with mandibular retrusion (ANB, 8.5°) and a severe high mandibular plane angle (FMA, 38.5°). Both the maxillary and mandibular incisors were proclined labially ( Fig 3 , A ; Table ).
| Measurement | Norm | Pretreatment (18 y 2 mo) | Posttreatment (20 y 0 mo) | Difference | |
|---|---|---|---|---|---|
| Mean | SD | ||||
| Angular (°) | |||||
| SNA | 82.8 | 4.0 | 78.3 | 77.7 | −0.6 |
| SNB | 80.1 | 3.9 | 69.9 | 70.5 | 0.6 |
| ANB | 2.7 | 2.0 | 8.4 | 7.2 | −1.2 |
| OP/SN | 16.1 | 5.0 | 30.9 | 29.2 | −1.7 |
| U1/SN | 105.7 | 6.3 | 105.9 | 91.4 | −14.5 |
| U1/MxP | 118.0 | 6.0 | 121.7 | 108.4 | −13.3 |
| IMPA | 96.5 | 6.4 | 102.2 | 90.1 | −10.1 |
| FMA | 27.3 | 7.1 | 38.5 | 35.8 | −2.7 |
| Linear (mm) | |||||
| Me-MxP | 64.0 | 4.0 | 66.5 | 65.2 | −1.3 |
| N-Mxp | 54.0 | 3.5 | 47.9 | 48.3 | 0.4 |
| U6-MxP | 28.0 | 2.1 | 26.9 | 25.8 | −1.1 |
| L6-MnP | 32.0 | 2.0 | 34.6 | 33.2 | −1.4 |
No symptoms of temporomandibular disorder were detected.
This patient was diagnosed with an Angle Class I malocclusion with a skeletal Class II base, a high mandibular plane angle, and a severe anterior open bite.
Treatment objectives
The treatment objectives were to (1) correct the tongue habits through musculature enforcement; (2) align and level the dental arch; (3) normalize the overjet and overbite relationships, closing the dental open bite; (4) upright the maxillary and mandibular posterior teeth, accomplishing normal and stable interdigitation; (5) intrude the mandibular posterior teeth and reduce the mandibular plane angle; and (6) improve the facial profile.
Treatment objectives
The treatment objectives were to (1) correct the tongue habits through musculature enforcement; (2) align and level the dental arch; (3) normalize the overjet and overbite relationships, closing the dental open bite; (4) upright the maxillary and mandibular posterior teeth, accomplishing normal and stable interdigitation; (5) intrude the mandibular posterior teeth and reduce the mandibular plane angle; and (6) improve the facial profile.
Treatment alternatives
Three treatment choices were considered for this patient. The first was orthodontics with orthognathic surgery, with a LeFort I osteotomy for maxillary impaction and a bilateral sagittal split ramus osteotomy for mandibular autorotation. The second choice was a pure fixed-appliance approach, aiming to achieve a compromised result without skeletal correction. The third option was fixed-appliance therapy complemented by localized surgery in the chin. The first option was not adopted because of the patient’s skeptical attitude toward the extensive surgery, nor was the second option because of its limited improvement in facial esthetics. With the third option, the genioplasty surgery was fully explained to the parents, and the predictive computer-generated tracings and photographs of the genioplasty helped the parents to realize the esthetic changes of this localized surgery ( Fig 4 ).




