Etiology and diagnosis
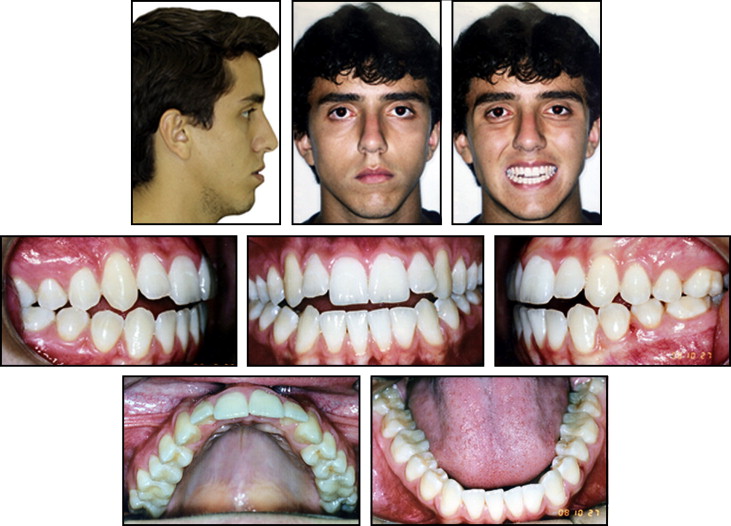
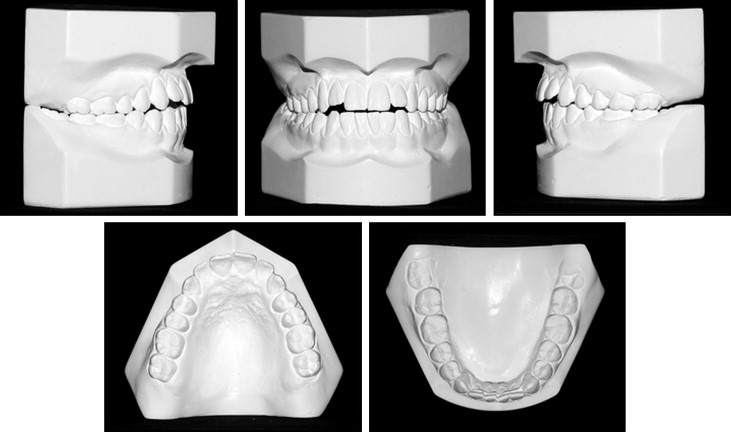
The patient was a 19-year-old Brazilian man. His medical history was noncontributory, and the extraoral examination showed a hyperdivergent facial profile, increased lower third of the face, labial incompetence, and increased nasolabial angle with the maxilla and mandible posteriorly positioned in the sagittal view. Intraorally, he had an anterior open bite, a deep curve of Spee in the maxillary arch, maxillary posterior teeth with excessive lingual crown inclinations, maxillary and mandibular midlines shifted 1 mm to the left, no significant transversal cant, proclined maxillary and mandibular incisors, and a Class I malocclusion ( Figs 1 and 2 ).
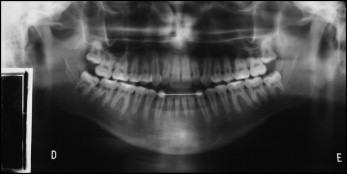
The panoramic radiograph showed signs of left condylar remodeling, vertically positioned maxillary and mandibular third molars, and a mandibular arch fixed retainer (canine to canine) from previous treatment ( Fig 3 ). The lateral cephalometric radiograph showed a narrow symphysis, proclined and protrusive maxillary and mandibular incisors, a long soft palate, decreased retroglossal and retropalatal airway spaces, and an increased mandibular occlusal plane angle ( Fig 4 ). Previous treatment relapses causing open bite and poor facial esthetics were the main concerns for a new orthodontic treatment.

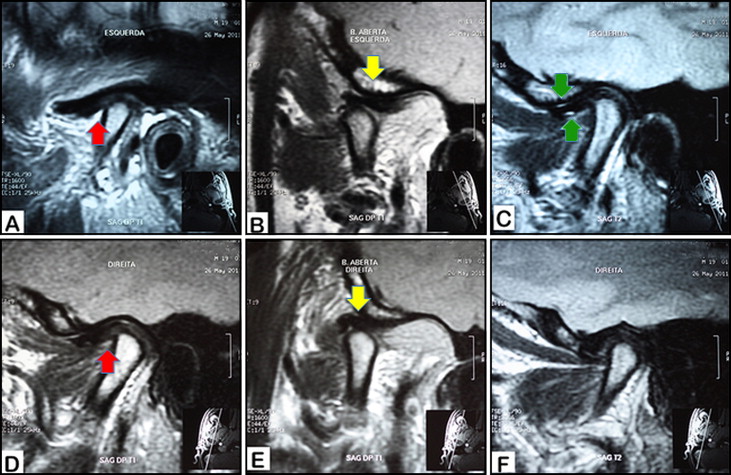
The physical examination of the patient showed signs of TMJ internal derangement that suggested further investigation with a magnetic resonance imaging (MRI) evaluation. Slight articular disc displacements with reduction were observed on the right and left TMJs with both discs’ morphology preserved ( Fig 5 ). The left fast spin echo weighted MRI immediately after surgery showed a level 1 hypersignal on the upper and lower TMJ compartments ( Fig 5 , C ).
Treatment alternatives
Intrusion of the maxillary and mandibular posterior teeth with temporary anchorage devices is an alternative for the treatment of anterior open bite in adults. Although the technique is not new, the immediate results are not predictable, and long-term results have yet to be published. Additionally, facial improvement would be restricted to mandibular counterclockwise rotation with no significant effect on the nasolabial angle and a minimal impact on the facial profile. For a surgical approach, 2 alternatives included (1) maxillary posterior impaction associated with chin advancement and vertical reduction, and (2) maxillomandibular counterclockwise rotation and advancement with vertical chin reduction. Maxillary posterior impaction would provide limited facial improvement because counterclockwise rotation of the mandible would be tied to the maxillary occlusal plane angle. This planning would be similar to orthodontic camouflage without the surgery.
Maxillomandibular counterclockwise rotation and advancement would better address the patient’s facial esthetic expectations but would increase TMJ loading and the risk for condylar resorption and osteoarthritis.
All treatment options were discussed with the patient and his parents, and they decided on a combined orthodontic and surgical treatment plan including double-jaw surgery.
Treatment progress
Before the surgery, Roth prescription 0.018-in slot brackets were placed on the maxillary and mandibular dentitions. Leveling and alignment were achieved in 3 segments (UR3-7, U2-2, and UL3-7) in the maxillary arch with this progression of archwires: 0.014-in nickel-titanium, 0.016 × 0.22-in nickel-titanium, 0.016 × 0.022-in stainless steel, and 0.017 × 0.025-in stainless steel. The same archwire progression was used with a continuous arch form in the mandibular arch.
Before surgery, the patient was advised to avoid potential deleterious habits (ie, clenching) to the TMJs and was referred to a nonsurgical TMJ specialist. A comprehensive screening by a rheumatologist showed no autoimmune disease involvement. The following medications were prescribed before surgery to control possible condylar resorption: vitamins C, D, and E; calcium; and omega-3 fatty acid. The surgery and initial recovery period were uneventful.
The immediate presurgical CBCT image (T1) was obtained 1 week before surgery, consisting of 3-piece LeFort I maxillary osteotomies, bilateral sagittal split ramus osteotomies with careful and passive proximal and distal segment repositioning, genioplasty, and methylmethacrylate implants on both zygomatic and infraorbital rims to improve the anteroposterior projection of the region. Immediately after surgery (T2), a bilateral Class I occlusion, normal overbite, and normal overjet had been achieved, and a new CBCT image was acquired. The palatal splint was removed 8 weeks after surgery, and postsurgical orthodontic treatment was resumed. After surgery, the patient was maintained with clonazepam (0.5 mg daily) for 1 year to control the bruxism that could affect bone healing and increase TMJ loading.
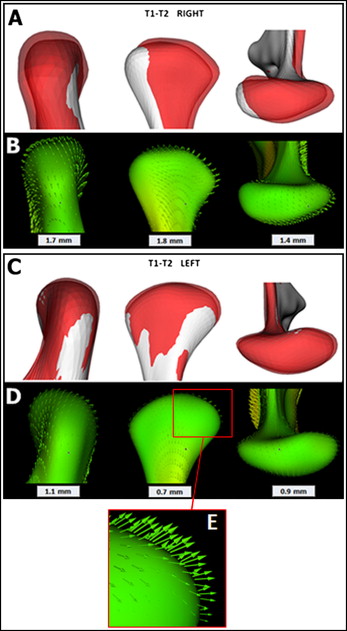
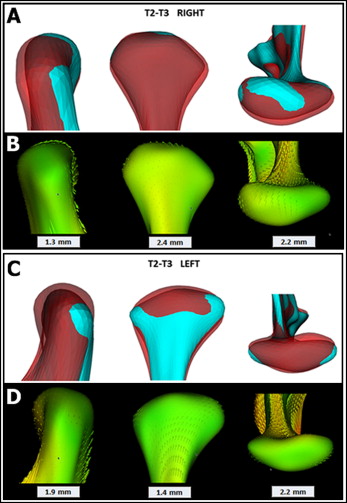
The maxillary sectioned arch was changed to a continuous arch 0.017 × 0.025-in copper-nickel-titanium and then to a continuous 0.017 × 0.025-in stainless steel archwire. Four months after surgery, the occlusion showed progressive shifting toward a slight canine Class II occlusion on the left side that remained 1 year after surgery (T3) as shown in a new CBCT image. Segmentations of all CBCT images were completed using open-source software ITK-snap ( http://www.itksnap.org ). Surgical and postsurgical 3D cranial base registrations were obtained with an automated rigid voxel-wise method for accurate assessment of condylar changes that were computed using SPHARM-PDM toolbox (freeware: http://www.nitrc.org/projects/spharm-pdm ). This method establishes correspondent surfaces based on their morphology; it is a precise tool for longitudinal measurement of 3D surface structures. Right and left condylar changes are shown as semitransparent overlays, displacement or remodeling direction vectors, and quantifications of surgical (T2-T1) and 1-year postsurgical (T3-T2) intervals ( Figs 6 and 7 ). During surgery, the predominant condyle displacement directions were posteriorly, superiorly, and laterally in both the right (1.7, 1.8, and 1.4 mm) and left (1.1, 0.7, and 0.9 mm) TMJs, respectively ( Fig 6 ). One year after surgery, the predominant right condyle was displaced anteriorly (2.4 mm), superiorly (2.2 mm), and medially (1.3 mm), whereas the left condyle moved posteriorly (1.4 mm), inferiorly (2.2 mm), and medially (1.9 mm) ( Fig 7 ). The left condyle was significantly smaller at 1 year after surgery. At this point, the possibility of other systemic medications was discussed with the patient and his parents to control the left condylar resorption: the disease-modifying antirheumatic drug (etanercept), a TNF-inhibitor, piroxicam, celecoxib, and doxycycline. All of these options were refused because of the potential side effects of long-term usage.
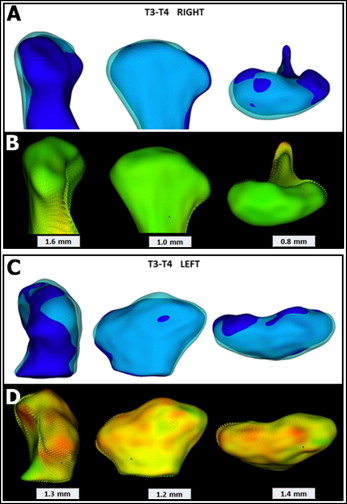
Because of the overall right and left condylar changes observed and left Class II canine tendency, it was decided to maintain the Class II mechanics with intermaxillary elastics to decrease condylar loading and allow possible TMJ adaptation. Debonding was postponed for another year. A new CBCT image was acquired 2 years after surgery (T4). Condylar changes were once again monitored and quantified between 1 and 2 years after surgery ( Fig 8 ). The predominant directions of condyle displacement and remodeling were anterior, inferior, and lateral in both the right (1.0, 0.8, and 1.6 mm) and left (1.1, 1.4, and 1.3 mm) condyles, respectively. The 2-year follow-up showed a slight left condyle overall dimensional decrease relative to the 1-year follow-up assessment ( Fig 8 ).
At the 2-year follow-up, the patient had no complaints, and the occlusion seemed to be stable within 3 months without intermaxillary Class II elastics. The patient and his parents agreed to debonding after we showed them our TMJ concerns and consequent occlusion limitations. The importance of close follow-up was emphasized because of the possibility for further condylar changes and consequent relapse. A mandibular fixed bar retainer (canine to canine) was bonded, and a maxillary removable retainer was constructed ( Fig 9 ).
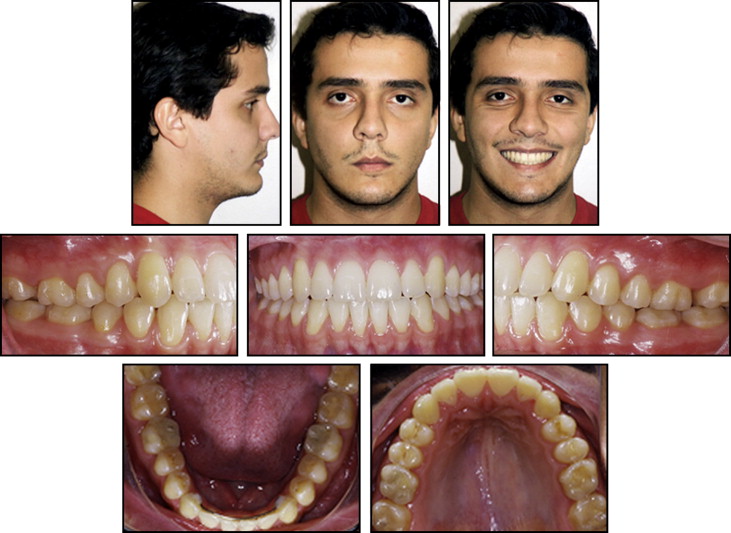
Treatment results
The patient’s overall facial esthetics was improved in both profile and the frontal view. Overbite and overjet were within normal limits, and a Class I relationship was achieved with the exception of the left canine, which remained with a slight Class II sagittal relationship. The mandibular midline was slightly shifted to the left; this could be explained by the remodeling direction of the left condyle. All anterior teeth had significant gingival dehiscences that were already present from the first treatment because vertical elastics were used to correct the open bite. Increased dehiscence with the second treatment was related to the orthodontic compensation of skeletal instability. The left canine area showed a 1-mm open-bite tendency even though the mandibular left canine was 1 to 2 mm more superior than the right one ( Figs 9-12 ). The superimpositions of the T1 and T3 cephalometric tracings showed significant counterclockwise rotation of the occlusal plane angle, maxillary advancement, mandibular advancement, and vertical reduction and advancement of the chin. The regional superimposition on the palatal bone showed uprighting of the maxillary incisors obtained with the 3-piece maxillary osteotomies and the anterior segment clockwise rotation. The mandibular plane superimposition showed significant mandibular incisor extrusion at the 1-year follow-up ( Fig 13 , A and B ). Overall postsurgical changes observed 2 years after surgery showed significant soft-tissue swelling resolution, slight maxillary incisor uprighting, and distal translation of the mandibular molars ( Figs 14 and 15 ).




