Piezocision-assisted orthodontic treatment is an innovative, minimally invasive surgical technique designed to help achieve rapid orthodontic tooth movement. Microsurgical interproximal openings are made in the buccal gingivae to let the piezoelectric knife create the bone injury that will lead to transient demineralization and subsequent accelerated tooth movement. When this procedure was first described, cuts were made simultaneously at the maxilla and the mandible. In recent years, the technique has evolved to a more staged approach, with selected areas or segments of the arch demineralized at different times during orthodontic treatment to help achieve specific results. The purpose of this article was to report the use of sequential piezocision in the correction of a Class III malocclusion, in a total treatment time of 8 months.
During the last decade, orthodontic innovations have changed and heightened clinicians’ and patients’ expectations. Although recent advances include appliances that are more acceptable to patients, especially to self-conscious adults, the length of orthodontic treatment is still a major concern. There have been many attempts to shorten treatment time, including rapid distraction of the canines and corticotomy-facilitated treatment. Corticotomy is an intentional injury to the cortical bone that was first described in 1892 as a surgical approach to correct malocclusion. This procedure was later modified and popularized by Kole, Suya, and Generson et al, as they referred to the “bony block” mechanical movement concept. These attempts have demonstrated that a combined corticotomy and osteotomy procedure could result in a shorter treatment time. In 2001, Wilcko et al revisited their original technique, adding bone to increase the alveolar thickness and allow tooth movement without creating dehiscences. They defined their approach as accelerated osteogenic orthodontics. They suggested that tooth movement in patients who underwent selective decortication might be due to a demineralization-remineralization process. This observation is part of a greater event that is known in the orthopedic literature as the regional acceleratory phenomenon, where a dynamic healing process occurs at the site of the osseous injury; the healing is proportional to the extent of the surgical insult. A recent publication has shown clearly that this is the mechanism. A localized surge in osteoclastic and osteoblastic activity results in a decrease in bone density and an increase in bone turnover. The regional acceleratory phenomenon begins within a few days of the surgery and usually peaks in 1 to 2 months, and then slows down and disappears as remineralization sets in.
Although effective and highly predictable, corticotomy-assisted orthodontic treatment is quite invasive because it requires extensive flap elevation and osseous surgery, which can cause postsurgical discomfort as well as various postoperative complications. Vercellotti and Podesta proposed the use of a piezoelectric knife instead of a high-speed surgical bur to decrease the surgical trauma and still achieve rapid tooth movement. Because of its micrometric and selective cut, a piezoelectric device produces safe and precise osteotomies without osteonecrotic damage. In 2009, Kim et al introduced the corticision technique as a minimally invasive alternative to create a surgical injury to the bone without flap reflection. In this technique, they used a reinforced scalpel and a mallet to go through the gingiva and cortical bone, without raising flaps. This surgical injury was deemed enough to induce the regional acceleratory phenomenon effect and move the teeth rapidly during orthodontic treatment. This technique, although innovative, has a few major drawbacks: the inability to graft soft or hard tissues during the procedure to correct inadequacies and reinforce the periodontium, and transient postsurgical dizziness from the repeated malleting during the surgery. In 2009, we proposed a new and minimally invasive procedure that we called “piezocision.” This approach combines microincisions to the buccal gingivae that allow for the use of the piezoelectric knife to decorticate the alveolar bone to initiate the regional acceleratory phenomenon. Although it is minimally invasive, it also has the advantage of allowing for hard-tissue or soft-tissue grafting via selective tunneling to correct gingival recessions or bone deficiencies in patients.
When this procedure was first described, the piezocision cuts were made simultaneously in both arches to correct the malocclusion. In this case report, we present a new application of piezocision-assisted orthodontic treatment. Sequential piezocision is introduced as a tool to correct a Class III malocclusion in a total treatment time of 8 months.
Diagnosis and etiology
A 25-year-old woman sought orthodontic treatment with chief complaints of misaligned teeth and an unfavorable smile. Her medical and family histories were not contributory. She had a slightly concave profile with a prominent nose and chin ( Fig 1 ).

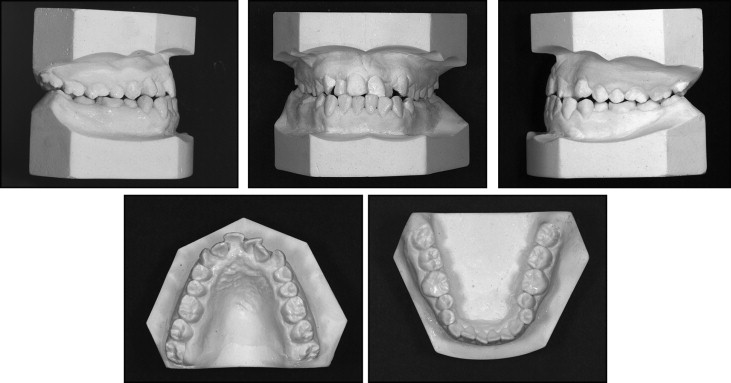
The intraoral examination showed that she had healthy periodontal tissues and good oral hygiene. Her maxilla was constricted. Her maxillary right second premolar, maxillary right canine, right and left lateral incisors, and maxillary left central incisor were in crossbite. She exhibited a Class III malocclusion with a narrow maxilla ( Fig 2 ). The space analysis done on the study models showed 7.5 mm of crowding in the maxillary arch and 2 mm of crowding in the mandibular arch. The radiographic evaluation showed no visible pathologies ( Figs 3 and 4 ). She had composite fillings on the maxillary central incisors, maxillary left lateral incisor, and mandibular first molars.


The cephalometric analysis showed a skeletal Class III pattern with an ANB angle of −1.2° and a Wits value of −9 mm ( Table ). The SNB value was in the normal range (78.4°), showing that the slight Class III pattern was due to the retracted position of the maxilla (SNA, 77.2°). IMPA and the angle axis of L1 to NB showed that the mandibular incisors were upright.
| Cephalometric measurement | Initial | Final |
|---|---|---|
| SNA (°) | 77.2 | 76.8 |
| SNB (°) | 78.4 | 78 |
| ANB (°) | −1.2 | −1.2 |
| FMIA (°) | 74 | 75 |
| FMA (°) | 18 | 21 |
| IMPA (°) | 88 | 84 |
| Wits appraisal (mm) | −9 | −6 |
| Interincisal angle (°) | 135.2 | 130.2 |
| Angle axis of U1 to NA (°) | 27.9 | 37.4 |
| Angle axis of U1 to SN (°) | 105.1 | 114.2 |
| Angle axis of L1 to NB (°) | 18.1 | 13.7 |
| Distance of U1 to NA (mm) | 11 | 15 |
| Distance of L1 to NB (mm) | 9 | 10 |
Treatment objectives
The treatment objectives for this patient were to correct the crossbites, resolve the crowding in the maxillary and mandibular arches, and achieve Class I molar and canine relationships. Ideal overjet and overbite relationships were also desirable to improve the occlusion and for anterior and lateral guidance. Other treatment objectives were to correct the incisor positions, maintain upper lip support for satisfactory facial harmony, and achieve favorable smile esthetics and profile.
Treatment objectives
The treatment objectives for this patient were to correct the crossbites, resolve the crowding in the maxillary and mandibular arches, and achieve Class I molar and canine relationships. Ideal overjet and overbite relationships were also desirable to improve the occlusion and for anterior and lateral guidance. Other treatment objectives were to correct the incisor positions, maintain upper lip support for satisfactory facial harmony, and achieve favorable smile esthetics and profile.
Treatment alternatives
Three treatment alternatives were presented to the patient.
One alternative included extraction of the maxillary first premolars to resolve the crowding and align the maxillary arch, and maxillary advancement surgery to correct the malocclusion and the profile. This option would correct the dental problems and significantly improve the facial profile. The patient was not willing to have orthognathic surgery under any circumstances and expressed that her primary concern was not to correct her facial appearance. Therefore, the surgical option was excluded.
Since the patient refused to have orthognathic surgery, extractions in the maxilla would create a more prominent Class III pattern; hence, the option of extractions to correct the crowding was eliminated.
Another alternative involved using surgically assisted rapid palatal expansion to create space to align the maxillary teeth and intermaxillary elastics to correct the malocclusion.
When the patient expressed her concern regarding treatment time, a third option was presented. This option would use piezocision to shorten the treatment time and also to create a more pliable bone structure to expand the maxillary arch. The amount of crowding in the maxillary arch was more than what could be resolved with expansion alone; therefore, interproximal reductions, especially on the teeth with the composite fillings, were also planned. Because the amount of correction needed in the maxilla was more significant than that in the mandible, a different therapeutic approach, concomitant with the piezocisions, was devised. The piezocisions were planned in a sequential manner, starting with the maxillary arch; after correction of the crossbites, the mandibular arch would be bonded and the mandibular piezocisions performed. The total treatment time for this option was estimated to be less than 1 year. The patient, refusing the orthognathic surgical treatment, decided to undergo piezocisions in conjunction with nonextraction treatment.
Rhinoplasty was also mentioned as another esthetic intervention to complement her profile at the end of the treatment.
Treatment progress
Treatment was started by bonding the maxillary arch only, from second molar to second molar but excluding the maxillary left lateral incisor because of the lack of space. A 0.014-in nickel-titanium alloy archwire was placed; bite-rising cones were placed on the mandibular molars to open the bite and create the interocclusal space for the crossbite corrections.
Piezocisions on the maxillary arch were done 9 days after the initial bracket placement. Local anesthesia was given, and 6 vertical interproximal incisions were made with a blade below the interdental papilla on the buccal aspect of the maxilla mesial to the first molars, and mesial and distal to the canines. These incisions were minimal, just to give access to the piezosurgical knife (Satelec; Acteon Group, Merignac, France), which was then used to create the alveolar decortication through the gingival opening to a depth of approximately 3 mm ( Fig 5 ). A prescription for a nonsteroidal anti-inflammatory drug was given, and the patient was advised to rinse twice a day with chlorhexidine for a week. Because of the rapid and temporary demineralization that occurs after piezocision as a result of the regional acceleratory phenomenon effect, the orthodontic appointments were scheduled every 2 weeks instead of every 4 weeks. The wire sizes progressed from 0.014-in nickel-titanium alloy to 0.016 × 0.022-in nickel-titanium alloy archwires for leveling and alignment. Once the crossbites were corrected, the bite opening cones on the mandibular molars were removed. Two and a half months after the maxillary piezocision, the mandible was bonded, and a 0.016-in nickel-titanium alloy archwire was placed. Piezocisions on the mandible were done 2 weeks later. Six vertical interproximal incisions were made in the same manner as described for the maxilla ( Fig 6 ). The archwires progressed from 0.016-in nickel-titanium alloy to 0.016 × 0.022-in stainless steel for leveling and alignment. Class III elastics were used to correct the Class III relationship. The orthodontic treatment was completed in 8 months. Fixed retainers were placed in both arches, and Hawley plates were given for retention.





