Introduction
Repair of root resorption cavities has been studied under light microscopy, scanning electron microscopy, and transmission electron microscopy. The aim of this investigation was to demonstrate the use of microcomputed tomography (micro-CT) to assist in the identification of the region of interest for light microscopy preparation. This study also qualitatively illustrated the root resorption craters with 4 or 8 weeks of retention after 4 weeks of continuous light or heavy orthodontic force application.
Methods
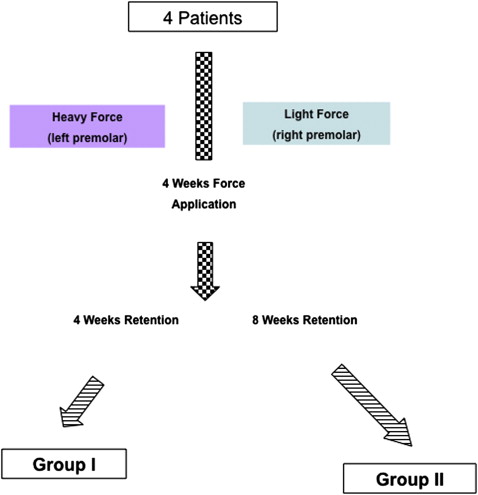
Four patients who required bilateral extractions of maxillary first premolars as part of their orthodontic treatment were divided into 2 groups (groups I and II) of 2. The maxillary left and right first premolars were loaded with light (25 g) or heavy (225 g) orthodontic force for 4 weeks. After 4 or 8 weeks of retention, the maxillary first premolars were extracted. The extracted teeth were investigated with micro-CT. By using 3-dimensional images created by the micro-CT, the largest resorption craters on the buccal and lingual sides were identified. Parasagittal sections of these resorption craters were studied histologically under hematoxylin and eosin staining.
Results
The use of micro-CT improved the efficiency and accuracy of histologic techniques. Comparatively, less root resorption was repaired by new cementum after heavy orthodontic force application and short retention time. The reparative processes seemed to depend on time, with longer retention time yielding the most amount of repair. Reparative cementum was a mixture of acellular and cellular cementum. Reparative processes seemed to commence at the central part of the resorption cavity and expand to the periphery.
Conclusions
Root resorption cavities have the potential to repair regardless of the orthodontic force magnitude. Correlative microscopy with micro-CT and conventional light microscopy adds a new dimension to current root resorption investigation techniques.
Brudvik and Rygh carried out studies on the repair of orthodontically induced inflammatory root resorption after application of 50 g of force for 21 days using light microscopy and transmission electron microscopy. They showed that the transition of active root resorption into a process of repair was associated with the invasion of fibroblast-like cells from the circumference of the resorption crater into the active root resorption site even with a light force. The formation of new tooth-supporting structures was seen in the periphery of the resorption lacunae, whereas active resorption by multinucleated odontoclast-like cells took place in the central parts. When orthodontic force was discontinued, the reparative process was similar to early cementogenesis during tooth development. It has been suggested that the epithelial cell rests of Malassez might have a significant role in mediating repair cementogenesis.
The resorptive defects are repaired by the deposition of new cementum and the reestablishment of new periodontal ligament. In a histologic study by Owman Moll and Kurol, 50 cN of buccally directed force was applied on maxillary first premolars for 6 weeks and passively retained up to 7 weeks. It was found that the repaired cementum was more of the cellular type than the acellular type. The acellular cementum occurred more often in the early phase of healing. The repair process did not vary with the location or the type of tissue, either on the buccal or the lingual side of the tooth, or in the cervical or apical parts of the root.
There are various patterns of repair in the resorption cavity. Depositions of cementum from both the periphery of the resorption cavity inward and the center outward have been identified. Brudvik and Rygh illustrated in their histologic studies that the repair process started in the periphery of the root resorption lacunae, while active resorption was still occurring beneath the main more centrally located and overcompressed hyalinized zone. Owman Moll and Kurol showed that healing cementum only occurred centrally in the bottom of the cavity and centrally and peripherally on 1 lateral wall of the cavity. This could be due to different sectioning orientations, or the specimens were collected at different times.
The aim of this investigation was to demonstrate the use of microcomputed tomography (micro-CT) to assist in the identification of the region of interest for light microscopy preparation. We also qualitatively studied the histology of root resorption craters after 4 or 8 weeks of retention after 4 weeks of continuous light or heavy orthodontic force application.
Material and methods
Eight first premolars were collected from 4 orthodontic patients (2 boys, 2 girls; age range, 10.3-15.3 years; mean, 13.7 years) who required bilateral maxillary first premolar extractions as part of their fixed appliance orthodontic treatment. They were recruited according to strict selection criteria as described previously. Ethics approvals were obtained from the Medical Faculty Ethics Committee of the University of Ondokuz Mayis in Samsun, Turkey, and the Human Research Ethics Committee of the University of Sydney in Surry Hills, New South Wales, Australia (EK:347 and 12-2005/1/8783, respectively). All subjects and their guardians consented to participate in this study after verbal and written explanations had been provided.
The subjects were divided into 2 groups (groups I and II) of 2 subjects in each group. They received a light conventional orthodontic force of 25 g on the maxillary left first premolar and a heavy conventional orthodontic force of 225 g on the maxillary right first premolar for 4 weeks. The premolars were then placed in retention, without orthodontic force application, for 4 or 8 weeks in groups I and II, respectively ( Fig 1 ).
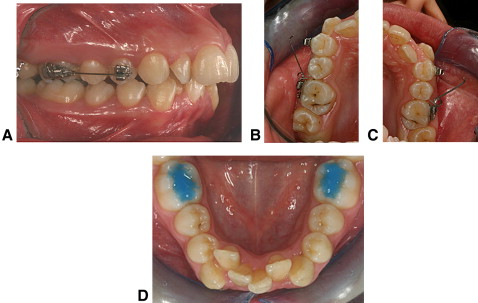
The 0.022-in slot SPEED brackets (Strite Industries, Cambridge, Ontario, Canada) were bonded on the buccal surfaces of the maxillary first permanent molars and the experimental maxillary first premolars ( Fig 2 , A ). Self-ligating brackets were selected to allow for standardized ligation of the experimental teeth. A buccally directed light orthodontic force of 25 g was induced by a 0.016-in titanium-molybdenum alloy cantilever spring (Rematitan, Dentaurum, Ispringen, Germany) ( Fig 2 , A and B ). A buccally directed heavy orthodontic force of 225 g was induced by a 0.017-in × 0.025-in titanium-molybdenum alloy cantilever spring (Beta III Titanium, 3M Unitek, Monrovia, Calif) ( Fig 2 , C ). The force magnitude was measured with a strain gauge (Dentaurum). Light-cured band cement (Transbond Plus, 3M Unitek) was bonded onto the occlusal surfaces of the mandibular first permanent molars to minimize occlusal trauma to the maxillary first premolars during the experimental period ( Fig 2 , D ).
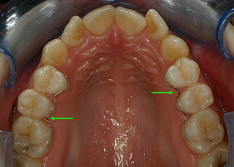
After 4 weeks of force application, the cantilever springs were removed, and the maxillary first premolars were retained by a custom-made passive retention wire bonded on the palatal surfaces of the maxillary first and second premolars and first molars with 0.0175-in multi-stranded stainless steel wire (TwistStraight, 3M Unitek) ( Fig 3 ). The maxillary first premolars were then extracted after either 4 or 8 weeks of retention. All extractions were performed by an oral surgeon who was instructed to avoid any forceps contact on the cervical cementum. Immediately after extraction, the teeth were stored in individual containers containing 10% buffered formalin for tissue fixation.
The extracted teeth were placed in a moist chamber of 10% buffered formalin and scanned by a desktop x-ray micro-CT system (SkyScan 1172, Aartsellaar, Belgium). Micro-CT is a variant of the medical CT scan system that allows nondestructive imaging of the internal microstructure of materials with high spatial resolution. The x-ray source was an air-cooled, sealed microfocus x-ray tube with a focal spot size less than 8 μ m. The x-ray tube was operated at 100 kV and 100 μ A with aluminum and copper filters. The x-ray detector consisted of a 1024 × 1024 pixel 16-bit charged coupled device camera with fiber-optic coupling to an x-ray scintillator. All teeth were scanned from the cementoenamel junction to the apex with resolution ranging from 14.38 to 16.11 μ m pixel size. Scanning of the teeth was done with 360° rotation around the vertical axis and a single rotation step of 0.2°. At each rotation step, an x-ray absorption radiograph was acquired. A total of 1800 x-ray absorption radiographs were acquired for each tooth and saved in 16-bit tagged image file format (TIFF).
After acquisition, an axial slice-by-slice reconstruction was performed with specific software (version 1.4.2, Nrecon, Aartsellaar, Belgium). Two-dimensional images were generated as 1024 × 1024 pixel bite-map images having an 8-bit greyscale dynamic range. Then, Studio Max software (version 1.2, Volume Graphics, Heidelberg, Germany) was used to collate the axial 2-dimensional slices to form a 3-dimensional (3D) reconstruction of the images.
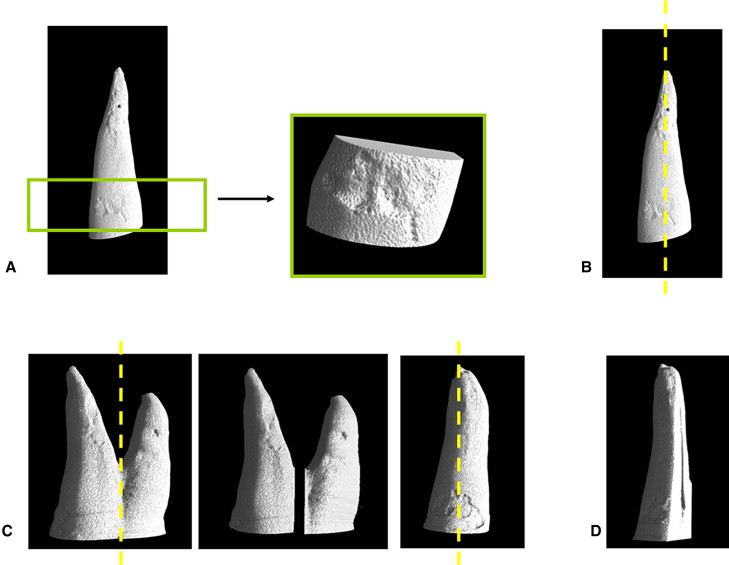
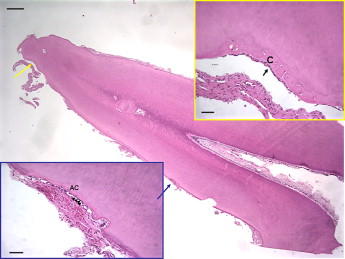
After micro-CT analysis, the teeth were prepared for histologic study. The samples were decalcified in 10% formic acid in phosphate-buffered formalin for approximately 4 weeks. The largest resorption craters on the buccal and lingual surfaces of each tooth were identified on the 3D images produced by the micro-CT scans ( Fig 4 , A ). By using these 3D images as a reference map, the specimens were grossly sectioned into 2 pieces for 1-rooted premolars or 4 pieces for 2-rooted premolars ( Fig 4 , B and C ). The samples were then embedded in paraffin ( Fig 4 , D ). Parasagittal sections of the mesiodistal aspects of the teeth were cut at 5 μ m with a microtome (Leica MicroSystems, Düsseldorf, Germany). Serial sections were stained with hematoxylin and eosin. From each specimen, the glass-containing sections with the longest root resorption crater length coronally and apically was chosen for the investigation. Color photographs were exposed in a light microscope with 1.25, 4, 10, and 20 times objective magnifications (OM). Histology was assessed for root resorption and associated repair.
Results
In group I, with 4 weeks of retention after 4 weeks of light orthodontic force, the buccal root showed 2 main areas of root resorption with associated repair: the apical third of the buccal root and the buccal surface of the buccal root at the cervical region ( Fig 5 ). On the lingual surface of the buccal root near the tooth apex, the resorption crater appeared to have extended into the dentin and was repaired by new cementum ( Fig 5 ). Cementocytes were also seen trapped in the new cementum; this might indicate repaired cementum of the cellular type. A layer of cementoblast-like cells overlaid the new cementum. However, the reparative cementum did not restore the anatomic contour of the root. Active root resorption craters were also evident near the root apex. The resorption crater was multiloculated and infiltrated with blood cells. The resorption crater on the buccal surface had also extended into the dentin ( Fig 5 ). The newly formed cementum in the bottom of the resorption cavity had no trapped cementocytes that indicated acellular cementum. However, the superficial layer of reparative cementum had incorporated cementocytes that indicated cellular cementum.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


