Introduction
The objective of this pilot randomized clinical trial was to investigate the relative effectiveness of anchorage conservation of en-masse and 2-step retraction techniques during maximum anchorage treatment in patients with Angle Class I and Class II malocclusions.
Methods
Sixty-four growing subjects (25 boys, 39 girls; 10.2-15.9 years old) who required maximum anchorage were randomized to 2 treatment techniques: en-masse retraction (n = 32) and 2-step retraction (n = 32); the groups were stratified by sex and starting age. Each patient was treated by a full-time clinic instructor experienced in the use of both retraction techniques at the orthodontic clinic of Peking University School of Stomatology in China. All patients used headgear, and most had transpalatal appliances. Lateral cephalograms taken before treatment and at the end of treatment were used to evaluate treatment-associated changes. Differences in maxillary molar mesial displacement and maxillary incisor retraction were measured with the before and after treatment tracings superimposed on the anatomic best fit of the palatal structures. Differences in mesial displacement of the maxillary first molar were compared between the 2 treatment techniques, between sexes, and between different starting-age groups.
Results
Average mesial displacement of the maxillary first molar was slightly less in the en-masse group than in the 2-step group (mean, –0.36 mm; 95% CI, –1.42 to 0.71 mm). The average mesial displacement of the maxillary first molar for both treatment groups pooled (n = 63, because 1 patient was lost to follow-up) was 4.3 ± 2.1 mm (mean ± standard deviation). Boys had significantly more mesial displacement than girls (mean difference, 1.3 mm; P <0.03). Younger adolescents had significantly more mesial displacement than older adolescents (mean difference, 1.3 mm; P <0.02).
Conclusions
Average mesial displacement of the maxillary first molar with 2-step retraction was slightly greater than that for en-masse retraction, but the difference did not reach statistical significance. This finding appears to contradict the belief of many clinicians that 2-step canine retraction is more effective than en-masse retraction in preventing clinically meaningful anchorage loss.
In many malocclusions, the goals of therapy can be achieved without extractions in the permanent dentition. But in some consequential percentage of cases, most orthodontists now agree that the goals of treatment cannot be achieved satisfactorily without the extraction of some permanent teeth. Extraction therapy is frequently indicated to correct severe crowding, retract the anterior teeth, correct molar mal-relationships, or modify the facial profile. In many of these patients, maxillary anchorage control is a consequential problem in orthodontic treatment.
The most common mechanism for making retraction space available involves the extraction of 1 premolar in each quadrant. To retract the anterior teeth into the extraction space, most treatment strategies involve attaching the anterior teeth to some structure posterior to them. The only structures available for this purpose (before the recent development of temporary anchorage devices) have been the maxillary and mandibular molars. But forces applied to the molars to retract the anterior teeth tend to displace the molars forward into the extraction spaces. This forward displacement is called “anchorage loss,” and its prevention is called “anchorage control.” In the mandibular dentition, anchorage loss is usually not a major problem because the molars are generally fairly resistant to mesial displacement. But, in the maxillary dentition, consequential mesial displacement of the first molar occurs more readily, and the problem can become severe. This is especially true in the treatment of Class II malocclusions.
Most techniques for retracting the anterior dentition involve preliminary bonding and leveling procedures soon after premolar extraction. After leveling, there are 2 general approaches to the problem of retracting anterior teeth with minimal mesial displacement of the maxillary first molar.
The most common approach is a sequential procedure in which the canines and incisors are retracted in 2 separate and distinct steps. In the first step, the canine in each quadrant is retracted to full contact with the tooth distal to the extraction space. In the second step, the canines are fastened to the teeth distal to them. The resulting grouping is then used as a single anchorage unit to retract the incisors. This procedure has been called the “2-step” technique.
In retracting the canines separately in the first step without adding the additional force that would be required to move the incisors at the same time, advocates of the 2-step approach assume that the load on the posterior teeth is lower, thus reducing the tendency of the maxillary molars to displace forward. In the second step, the posterior segments, now buttressed by the incorporation of the canines, are pitted against the reduced resistance of the incisors alone.
However, there are some conceivable disadvantages to the 2-step approach. Closing space in 2 steps rather than 1 might make treatment take longer. Also, when canines are retracted individually, they tend to tip and rotate more than when the anterior teeth are retracted as a single unit, thus requiring additional time and effort to relevel and realign.
Therefore, an alternative approach called “en-masse retraction” has come into use in which the incisors and canines are retracted as a single unit. One therapeutic technique that uses this approach is the MBT system developed by Bennett and McLaughlin. This en-masse technique has recently gained popularity because of its mechanical simplicity. But, in theory, it might be expected to tax the posterior anchorage more than the 2-step technique.
A randomized controlled clinical trial (RCT) was conducted to test the relative effectiveness of these 2 retraction techniques under actual clinical conditions. For this purpose, 64 maximum anchorage patents were randomized to treatment by 8 full-time clinical instructors, each experienced in the use of both retraction techniques. Each clinician treated the same number of patients. Differences in mesial displacement of the maxillary first molar were measured between the 2 treatment techniques, between the sexes, and between patients who started treatment at different stages of growth. Other parameters of interest were also investigated and will be reported later. The trial was designed with the assistance of Dr Edward L. Korn of the Biometric Research Branch, National Cancer Institute, Rockville, Md. It was conducted at the orthodontic clinic of the Department of Orthodontics, Peking University School of Stomatology, Beijing, China, in consultation with colleagues at the Craniofacial Research Instrumentation Laboratory of the Arthur A. Dugoni School of Dentistry at the University of the Pacific in San Francisco.
The primary purpose of the study was to test whether there were statistically significant between-treatment differences in mesial displacement of the maxillary first molar when maximum anchorage patients were randomized to both kinds of treatment. Our secondary purpose was to test the feasibility of performing an orthodontic RCT in this distributed setting.
Material and methods
Before the study, a power analysis was performed by Dr Korn to determine the required sample size. This analysis was based on the known variability of maxillary molar mesial displacement as measured in previous extraction studies at the University of the Pacific and the University of Medicine and Dentistry of New Jersey. It was determined that a sample size of 32 patients per group would be sufficient to detect a true mean difference of 1.75 mm between techniques at the P <0.05 level (2-sided) with 80% power. Therefore, the study was begun with the recruitment of a random sample consisting of 64 maximum-anchorage patients.
Potential patients were identified during their initial visits to the departmental clinic. Criteria for inclusion were that each selected patient (1) had a Class I or Class II malocclusion whose treatment required maximum anchorage control, (2) had erupted permanent canines and no missing permanent teeth, (3) had not yet reached his or her 16th birthday, and (4) was in good health with no chronic disease or disability.
A preliminary decision that each patient met these criteria was made by a full-time project screener (X.Z.), an orthodontist with 8 years of clinical experience. A stratified block randomization was then used to ensure that the samples for the 2 treatment techniques were well balanced for sex, Angle class, and starting age. After randomization to treatment technique, each patient was randomly assigned to care by 1 member of a panel of 8 clinicians. Each member of the panel was experienced in the use of both the en-masse and the 2-step technique. However, before assignment was confirmed, it was further required that the clinician to whose care each patient was assigned agreed with the project screener (5) that the patient required maximum anchorage control, and (6) that it was appropriate to treat the patient using the treatment technique to which the patient had been randomized.
The last 2 requirements were included to meet the ethical and therapeutically important condition that no clinician be asked to treat a patient using a technique that he or she considered inappropriate for that particular patient.
Stratified randomization ensured that the subsamples for the 2 treatment techniques were well balanced for sex, Angle class, starting age, and pretreatment crowding ( Table I ).
| Sex | Angle class | Crowding | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Treatment method | n | Starting age (mean ± SD) (y) | Female | Male | I | II | <3 mm | 3-6 mm | >6 mm |
| En-masse | 32 | 12.6 ± 1.1 | 20 | 12 | 15 | 17 | 20 | 11 | 1 |
| Two-step | 31 ∗ | 12.7 ± 1.2 | 19 | 12 | 16 | 15 | 21 | 10 | 0 |
∗ One patient, later lost to follow-up, was deleted from the group statistics.
Except for the requirement to use the prescribed retraction technique and some form of headgear, all treatment planning decisions for each patient were made by the treating clinician. These decisions explicitly included the type of headgear to be used, the choice of extraction pattern, and whether to use a transpalatal appliance (TPA) for additional anchorage support. Latitude in making all treatment decisions for each patient was delegated to the treating clinician because these decisions were considered to be part of the clinician’s unique treatment plan for the patient. (This issue will be considered further in the “Discussion” section of this article.)
The subjects for both techniques were treated with appliances of the same type (MBT prescription, 0.022 × 0.028-in bracket slot, 3M Unitek, Monrovia, Calif). The treatment protocols of the 2 samples differed solely as follows: in the en-masse sample, the canines were retracted with laceback until crowding was eliminated and a Class I canine relationship was attained, after which the remaining extraction space was closed by retracting the 6 anterior teeth as a single unit. In the 2-step sample, the canines were retracted first by laceback until they contacted the second premolars. The 4 incisors were then retracted by using sliding mechanics.
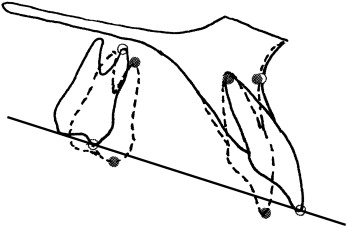
All measurements of tooth displacement reported in this article reflect differences in tooth position between beginning-of-treatment (T1) and end-of-treatment (T2) lateral cephalograms superimposed on the anatomic structures of the hard palate and the anterior maxillary process ( Fig ). Displacements of the maxillary incisors and molars were measured parallel and perpendicular to the pretreatment Downs occlusal plane. All measurements are the averages of replicate landmark locations and tracing superimpositions independently performed by blinded and calibrated investigators using previously reported computer-assisted techniques developed at the Craniofacial Research Instrumentation Laboratory at the University of the Pacific.
Reflection will make it apparent that what was being measured here was not “anchorage loss” per se. Rather, it was the total mesial displacement of the maxillary first molars between T1 and T2 after fixed appliance therapy. Hence, our measurements of molar displacement include not only treatment-associated changes during the periods of active space closure and subsequent finishing procedures, but also the effects of intercurrent growth changes throughout the active treatment period. A more precise measurement of anchorage loss during active space closure itself could have been obtained by generating an additional comparison cephalogram at the precise time that space closure was deemed complete. But this would have been technically difficult and of only academic value. For the purposes of this investigation, total mesial displacement of the maxillary first molar was used as an excellent surrogate measurement for “anchorage loss.” But beyond its surrogate role, we believed that total mesial displacement of the molar during treatment was the variable of greater interest to the clinical practitioner.
Statistical analysis
The primary hypothesis investigated in this study was the belief of most orthodontic clinicians that on average there would be significantly less mesial displacement of the maxillary first molar during 2-step retraction than during en-masse retraction. This hypothesis was tested in the null form—ie, that there would be no statistically significant difference in mesial displacement of the maxillary first molar between a sample of patients treated with the en-masse technique and an equivalent sample treated with the 2-step technique. The frequency, correlation, and t test procedures of the SAS statistical package (version 9.2, SAS Institute, Cary, NC) were used to analyze the data.
Results
The findings for maxillary molar displacement during space closure are reported in Table II . It can be seen that, relative to superimposition on palatal structures, no statistically significant difference in mesial displacement of the maxillary first molars was observed between the 2 retraction techniques. For the 2 treatment groups pooled, mean mesial displacement of the maxillary first molar at the molar cusp was slightly more than 4.3 ± 2.1 mm, with the apex moving forward by 2.7 ± 1.7 mm. In this study, mean mesial displacement of the maxillary first molar with respect to superimposition on palatal structures was slightly greater in the 2-step sample than in the en-masse sample; the best estimate of the average difference between the techniques was slightly less than 0.4 mm.
| Variable | En-masse (n = 32) | Two-step (n = 31) | Mean difference | P value |
|---|---|---|---|---|
| Maxillary first molar changes | ||||
| Mesial displacement at U6 cusp (mm) | 4.1 ± 2.0 | 4.5 ± 2.2 | −0.36 | 0.51 (NS) |
| Mesial displacement at U6 apex (mm) | 2.5 ± 1.8 | 2.9 ± 1.5 | −0.32 | 0.45 (NS) |
| Mesial crown tipping of U6 (°) | 7.4 ± 4.4 | 6.9 ± 4.8 | 0.43 | 0.71 (NS) |
| Extrusion of U6 cusp (mm) | 2.2 ± 1.5 | 2.0 ± 1.4 | −0.26 | 0.48 (NS) |
| Extrusion of U6 apex (mm) | 1.7 ± 1.4 | 1.8 ± 1.4 | 0.09 | 0.80 (NS) |
| Maxillary central incisor changes | ||||
| Retraction of U1 edge | 5.7 ± 2.0 | 5.7 ± 2.4 | −0.03 | 0.96 (NS) |
| Retraction of U1 apex (mm) | 0.1 ± 2.0 | 0.1 ± 1.6 | 0.08 | 0.86 (NS) |
| Extrusion at U1 edge (mm) | 2.6 ± 1.6 | 1.7 ± 1.5 | −0.87 | 0.029 ∗ |
| Extrusion at U1 apex (mm) | 0.2 ± 1.7 | −0.2 ± 1.6 | −0.37 | 0.38 (NS) |
| U1 lingual crown tipping (°) | 10.7 ± 5.1 | 10.1 ± 4.7 | −0.53 | 0.67 (NS) |
| Apical root resorption (mm) | −1.2 ± 1.8 | −1.4 ± 1.9 | 0.18 | 0.66 (NS) |
| Treatment time (y) | 2.5 ± 0.9 | 2.6 ± 0.8 | −0.1 | 0.58 (NS) |
∗ P <0.05, unadjusted for multiple comparisons; NS , not significant.
Extrusion of the maxillary molar, measured as the distance from the superimposed palatal structures to the molar cusp, was also similar for the 2 treatment groups. For the pooled sample of 63 (1 patient was lost to follow-up), its mean value increased an average of 2.1 ± 1.5 mm; the average difference between the 2 treatment groups was less than 0.3 mm. At the molar apex, downward displacement was slightly less, with the pooled average value 1.8 ± 1.4 mm and a mean between-treatment difference of 0.1 mm.
For a more complete picture of maxillary dental changes during space closure, corresponding statistics on incisor retraction and extrusion are also included in Table II . Retraction at the incisal edge was also extremely similar in the 2 samples, averaging 5.7 ± 2.2 mm for the 2 samples pooled, with a between-treatment mean difference of only 0.1 mm. The findings for retraction at the incisor apex were less expected and surprising. Essentially, no retraction of the incisor apex was detected in either treatment group (mean, –0.1 ± 17 mm).
Extrusion at the incisal edge of the maxillary central incisor was greater in the en-masse sample than in the 2-step sample. The mean difference of 0.9 mm between the 2 treatments was statistically significant ( P <0.03) but probably of little clinical importance. Part of the difference might be associated with the slightly greater lingual crown tipping observed in the en-masse group.
As a further control, we checked for between-sample differences in incisor root resorption and found that the mean difference was less than 0.2 mm. We also checked the mean difference in treatment time between the 2 treatment samples and found it to be less than 1.3 months.
In evaluating these findings, we investigated the possibility that there might have been consequential differences other than retraction technique between the en-masse and the 2-step samples. Such differences could have resulted either from chance distortions in the randomization process or systematic differences in the way treatment was delivered in the 2 samples. The second of these possibilities was particularly important in experimental designs such as this one in which, after randomization, each clinician was asked to make all treatment decisions entirely based on his or her judgment of what treatment plan was best for each patient. In this study, it therefore became desirable to know whether the differences in the clinicians’ in-course treatment decisions for individual patients concerning headgear type, TPA use, and extraction pattern were balanced between the 2 subsamples. Table III provides answers to this question.
| Headgear | TPA | Extraction pattern | ||||
|---|---|---|---|---|---|---|
| Treatment method | Cervical | High-pull | Used | Not used | U4-L4 | U4-L5 ∗ |
| En-masse (n = 32) | 24 | 8 | 27 | 5 | 22 | 8 |
| Two-step (n = 31) | 24 | 7 | 21 | 10 | 21 | 11 |
| Total (n = 63) | 48 | 15 | 48 | 15 | 43 | 19 |
∗ Includes 1 patient with congenitally missing mandibular second premolars in each treatment group.
The tabulated distributions for headgear type, use or nonuse of TPAs, and choice of extraction pattern were quite similar between techniques. The use of TPAs seemed slightly more conservative in the en-masse sample, and the choice of extraction pattern seemed slightly more conservative in the 2-step sample, but neither finding was statistically significant.
Early in the analysis of the data from the study, an extensive cephalometric comparison of the T1 state of the 2 treatment subsamples was made. This comparison examined 35 conventional cephalometric measurements. Results of the comparison are summarized in Table IV without correction for multiple comparisons.
| Variable | En-masse (n = 32) (mean ± SD) | Two-step (n = 31) (mean ± SD) | Mean difference | P value |
|---|---|---|---|---|
| Skeletal measurements | ||||
| SNA (°) | 83.1 ± 2.9 | 82.1 ± 3.0 | 0.99 | 0.18 |
| SNB (°) | 77.0 ± 3.4 | 76.7 ± 3.5 | 0.31 | 0.72 |
| ANB (°) | 6.1 ± 1.9 | 5.4 ± 1.9 | 0.68 | 0.16 |
| SNPg (°) | 76.7 ± 3.5 | 76.4 ± 3.5 | 0.31 | 0.72 |
| Gonial angle (°) | 129.5 ± 5.6 | 128.5 ± 5.8 | −1.00 | 0.49 |
| Maxillary length (Co-A) (mm) | 89.4 ± 5.3 | 91.9 ± 4.5 | −2.49 | 0.05 ∗ |
| Mandibular length (Co-Pg) (mm) | 110.5 ± 6.7 | 113.9 ± 4.6 | −3.40 | 0.02 ∗ |
| Wits appraisal (mm) | 3.1 ± 3.4 | 2.8 ± 3.4 | 0.29 | 0.74 |
| Facial plane angle (°) | 83.5 ± 3.3 | 83.9 ± 3.8 | −0.40 | 0.65 |
| Mandibular plane to SN plane angle (°) | 38.3 ± 5.4 | 37.8 ± 5.6 | 0.54 | 0.70 |
| Mandibular plane to FH plane angle (°) | 31.6 ± 5.2 | 30.3 ± 5.6 | 1.25 | 0.36 |
| Mandibular plane to palatal plane angle (°) | 28.6 ± 4.6 | 27.6 ± 5.3 | 1.05 | 0.41 |
| Anterior facial height (AFH) (mm) | 119.7 ± 6.6 | 122.2 ± 4.4 | 2.44 | 0.09 |
| Posterior facial height (PFH) (mm) | 78.0 ± 6.4 | 79.9 ± 6.1 | 1.86 | 0.24 |
| Lower facial height (LFH) (mm) | 64.2 ± 4.9 | 65.5 ± 2.6 | 1.31 | 0.19 |
| PFH/AFH (%) | 65.2 ± 3.6 | 65.4 ± 4.1 | 0.20 | 0.83 |
| LFH/AFH (%) | 53.6 ± 1.8 | 53.6 ± 1.4 | 0.05 | 0.89 |
| Y-axis angle (°) | 65.6 ± 3.8 | 65.3 ± 3.7 | 0.31 | 0.74 |
| Point A to sella, horizontal distance parallel to FH (mm) | 89.4 ± 5.8 | 91.2 ± 4.9 | −1.85 | 0.18 |
| Point B to sella, horizontal distance parallel to FH (mm) | 78.5 ± 6.7 | 81.2 ± 6.5 | −2.69 | 0.11 |
| Dental measurements | ||||
| Overjet (mm) | 6.8 ± 2.8 | 6.7 ± 2.3 | 0.08 | 0.90 |
| Overbite (mm) | 3.4 ± 2.0 | 3.6 ± 1.8 | −0.22 | 0.64 |
| Interincisal angle (°) | 106.6 ± 6.9 | 107.3 ± 4.9 | −0.71 | 0.64 |
| Occlusal plane to palatal plane angle (°) | 8.4 ± 3.0 | 7.7 ± 3.7 | 0.75 | 0.38 |
| U1 to SN angle (°) | 113.6 ± 6.3 | 113.0 ± 5.2 | −0.61 | 0.68 |
| L1 to MP angle (°) | 101.4 ± 6.2 | 101.9 ± 4.4 | −0.45 | 0.74 |
| U1 to NA angle (°) | 30.6 ± 6.9 | 31.0 ± 5.6 | −0.39 | 0.81 |
| U1 to NA distance (mm) | 8.0 ± 2.6 | 8.3 ± 1.9 | −0.37 | 0.52 |
| L1 to NB angle (°) | 36.8 ± 5.5 | 36.3 ± 4.6 | 0.41 | 0.75 |
| L1 to NB distance (mm) | 10.6 ± 2.4 | 10.1 ± 2.1 | 0.47 | 0.41 |
| Soft-tissue measurements | ||||
| Upper lip to E-plane (mm) | 4.8 ± 2.0 | 4.8 ± 1.7 | 0.02 | 0.96 |
| Lower lip to E-plane (mm) | 5.9 ± 2.9 | 6.2 ± 2.1 | −0.21 | 0.74 |
| Z-angle (upper lip) (°) | 61.1 ± 6.8 | 62.0 ± 5.5 | −0.95 | 0.55 |
| Z-angle (lower lip) (°) | 53.0 ± 9.1 | 53.5 ± 7.8 | −0.51 | 0.81 |
| H-angle (°) | 26.5 ± 4.7 | 25.8 ± 3.4 | 0.70 | 0.50 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


