(1)
Department of Endodontics, New York University College of Dentistry, New York, NY, USA
Abstract
This chapter describes the indications and value of periapical, bitewing, panoramic, and cone beam computed tomography (CBCT) in the diagnostic process. The selection of appropriate radiographs is described in the context of ALARA (as low as reasonably achievable) in terms of radiation exposure. The importance of using more than one radiograph for diagnosis is stressed.
The biology and selection of appropriate sensibility and other clinical tests is critical to the diagnostic process. The importance of using more than one test is emphasized. Diagnostic complications are also reviewed. All sensibility tests are subject to false-positive (i.e., a positive response from a necrotic pulp) and false-negative responses (i.e., a negative response from a vital pulp).
In order to establish a diagnosis and treatment plan, the clinician must synthesize the results of radiographs, sensibility tests, and other clinical findings. No single radiograph or sensibility test is ever sufficient. Information drawn from additional radiographs or sensibility tests may be invaluable in reaching a diagnosis and treatment plan. The importance of periodontal probing is emphasized. Periodontal probing may provide important information that is not observed on radiographs or visual examination.
3.1 Radiographs
Radiographs are an essential part of the diagnostic process. The dentist must choose between several types of radiographs including conventional, digital, and cone beam techniques. There should be a specific goal for each image while simultaneously attempting to limit the patient’s exposure to radiation.
3.1.1 Periapical Radiographs
A periapical radiograph represents a basic starting point and provides an overall view of the teeth and the supporting structures in the suspect quadrant. The final diagnosis and treatment plan must not be made on the basis of a single radiograph. A slight change of angulation may allow a clinician to visualize complicating factors such as additional roots, periapical pathosis, fracture, or periodontal defect that were not apparent on the initial radiograph. A periapical radiograph should allow visualization of the entire tooth as well as adjacent teeth in the quadrant. The full extent of periapical pathosis must be visible. The relationship between root apices and the mandibular canal or maxillary sinus should be observed (Figs. 3.1, 3.2, and 3.3).




Fig. 3.1
Preoperative radiograph indicates dystrophic calcification of the canal and periapical pathosis (Courtesy of Dr. Joshua Most)

Fig. 3.2
Use of surgical operating microscope and enhanced lighting enabled treatment of the tooth (Courtesy of Dr. Joshua Most)

Fig. 3.3
Healed lesion (Courtesy of Dr. Joshua Most)
Clinical Tips
-
A sharper image of a tooth results from slightly increasing vertical angulation thus foreshortening periapical radiographic images.
3.1.2 Bitewing Radiographs
The bitewing radiograph provides an excellent view of the pulp chamber and may reveal previous pulp caps or calcifications that were not apparent on periapical radiographs. Visualization of the pulp chamber is of value in difficult diagnostic situations. For example, a markedly constricted pulp chamber, under a deep restoration, may be evidence of long-term inflammation and calcification. This could be a valuable clue in determining the cause of a patient’s pain. Visualization of the chamber is also helpful prior to establishing access. A calcified chamber makes it more challenging to establish access and identify the canals. Knowledge of a calcified chamber is important in preventing perforation of the floor of the chamber during access.
Clinical Tips
-
Accessing a tooth with full coverage is particularly challenging because radiographs will not demonstrate chamber anatomy.
-
Teeth with diffuse calcification in their chambers and full coverage are prone to perforation unless the clinician recognizes the potential problem.
-
Radiographs taken before full coverage of the tooth are helpful in serving as a guide during access. The clinician is advised to develop access using slow speed after the roof of the chamber is removed. This step is helpful in preventing perforation of the chamber floor especially in teeth with full coverage or extensive restorations.
3.1.3 Panoramic Radiographs
Although a panoramic radiograph is useful in scanning for gross pathosis, it does not provide sufficient detail to be of value in searching for dental defects such as caries or cracks. When the clinician suspects pathosis of non-endodontic origin, it is useful in scanning the maxillae and mandible. The panoramic radiograph has been largely replaced by cone beam radiographs because of its three-dimensional capability.
3.2 Cone Beam Computed Tomography (CBCT)
The cone beam radiograph (CBCT), the newest of the radiographic modalities, has important attributes useful for an endodontist. However, it should not be used as a routine scanning device. The advantages of CBCT include three-dimensional imaging of periapical pathosis as well as canal anatomy and proximity of root apices to vital anatomic structures (Fig. 3.4).
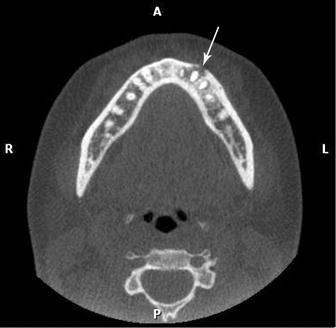
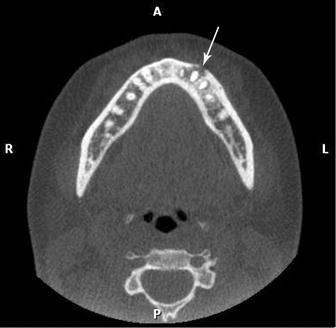
Fig. 3.4
Cone beam computed tomography (CBCT) of mandibular left premolar area. Arrow indicates buccal bone destruction
Clinical Tips
-
Three-dimensional images of periapical pathosis close to the maxillary sinus, floor of the nose, or mandibular canal are invaluable.
-
A radiologist may be required to completely review a CBCT image.
3.2.1 ALARA
Undue radiation exposure is a factor that must be considered. ALARA is an acronym for “as low as (is) reasonably achievable,” which means making every reasonable effort to maintain patient exposure to ionizing radiation as far below the dose limits as practical [11].
3.2.2 Field of View (FOV)
Field size limitation ensures that an optimal FOV can be selected for each patient based on diagnostic needs and the region to be imaged. In general, the smaller the scan volume, the higher the resolution of the image and the lower the effective radiation dose to the patient.
3.2.3 Limited Field of View (FOV)
For most endodontic applications, limited or focused FOV CBCT is preferred over large volume CBCT for the following reasons:
-
Decreased radiation exposure
-
Increased resolution to improve diagnostic accuracy
-
Focus on anatomic area of interest
3.2.4 Position Statement: Cone Beam Computed Tomography
The American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology jointly developed a position statement concerning cone beam computed tomography (CBCT). It is intended to provide scientifically based guidance to clinicians regarding the use of CBCT in endodontic treatment. The document, available at (www.aae.org/colleagues/), will be periodically revised to reflect new evidence [1].
3.2.5 Interpretation
Clinicians ordering a CBCT are responsible for interpreting the entire image, just as they are for any other radiographic image. Any radiograph has the potential to demonstrate findings that are significant to the health of the patient. There is no informed consent process that allows the clinician to interpret only a specific area of an image. Therefore, the clinician can be liable for a missed diagnosis, even if it is outside his/her area of practice [2]. Any questions by the practitioner regarding image data interpretation should be referred to a specialist in oral and maxillofacial radiology.
3.2.6 Recommendations
CBCT should only be used when the question for which imaging is required cannot be answered adequately by lower dose conventional dental radiography or alternate imaging modalities. Initial studies regarding the use of CBCT for a variety of endodontic-related imaging tasks have demonstrated the effectiveness and comparability of CBCT to conventional radiography [3, 7, 9, 11].
3.2.7 Research: CBCT vs. Biopsy
A study investigated the differentiation of radicular cysts from granulomas. Cone beam computed tomography (CBCT) imaging was compared with the existing standard, biopsy, and histopathology.
Based on the inconsistency of the radiologists’ reports, as evidenced by statistical analyses, it was concluded that CBCT imaging is not a reliable diagnostic method for differentiating radicular cysts from granulomas.
Surgical biopsy and histopathologic evaluation remain the standard procedure for differentiating radicular cysts from granulomas [13] as well as other pathosis.
3.3 Diagnostic Testing
There are a number of sensibility tests that are useful in identifying pulp/periapical disease. Each test offers the potential of providing clues during the diagnostic process. Attempts to predict the histology of the pulp based only on clinical signs and symptoms or on electric pulp and/or thermal tests and radiographs have not been successful [5, 8].
The initial history of the chief complaint, medical and dental histories, and diagnostic radiographs represent the starting point in the inquiry and may lead the clinician to a tentative diagnosis even before sensibility tests are administered. The tests all have a degree of subjectivity associated with them, and the dentist’s ability to interpret the findings is crucial.
No single test is definitive and each test should be confirmed by use of other tests. Only then can information drawn from the history of the chief complaint, radiographs, and sensibility tests be synthesized into a meaningful complete story. The pieces of the puzzle must fit. Where there is a discordant note, the clinician must reassess the evidence.
An example of a discordant note occurs when an apparent periapical lesion is associated with a root apex on radiographs but the tooth in question repeatedly tests vital on sensibility tests. A vital response to stimuli would not be expected in a tooth with a necrotic pulp and periapical pathosis. At this stage of the diagnostic process, reassessment is in order, and a non-odontogenic origin of the lesion would have to be explored.
That puzzle represents a signal to reach out for help. For example, an oral surgeon might be of assistance in performing a biopsy on the suspect lesion. A cone beam radiograph would also be helpful in providing a three-dimensional view of the lesion.
Clinical Tips
-
Do not start endodontic treatment when in doubt about the origin of pain or the apparent odontogenic basis of an apical lesion.
-
Recognize that commonly used diagnostic tests are subjective and can be misinterpreted.
-
Depending on the results of a single test is dangerous.
3.3.1 Diagnostic Testing
This section will describe test techniques, their biological basis, and significance and the treatment indicated.
Sensibility Tests
Thermal
-
Cold
-
Heat
-
Electric
Clinical Tests
-
Palpation
-
Percussion
-
Bite block
-
Transillumination
Assessment of pulp vitality is an important aspect of diagnosis. Responsiveness of a tooth to the application of stimuli is the basis of traditional sensibility tests [6, 8, 12]. A positive response to a sensibility test means only that there is at least some vital neural responsive tissue in the root canal. It should not be interpreted to mean that the tissue is normal or healthy.
For example, a tooth with a vital pulp and a deep carious lesion or exposure may respond normally to electric and cold sensibility tests, but that response does not indicate a healthy pulp. The clinician must interpret the results of sensibility tests with caution. These tests may be complicated by a number of clinical factors including age of the patient, recent trauma, dystrophic calcification, and the presence of large restorations. High levels of patient anxiety may also complicate the diagnostic process.
Patients’ responses are subjective in nature as are the interpretations of clinicians. It is critical that clinicians recognize that there is no single definitive test. The information drawn from the history of the chief complaint, radiographs, and sensibility tests must be synthesized to reach a final diagnosis and treatment plan.
Thermal Tests
Information collected from testing with cold or heat provides an indication only of the presence or absence of functioning nerve fibers. The tests do not provide information about the blood flow and actual biological status of the tooth. A clinician may conclude that a positive response to a test means that pulp tissue is healthy, but this is not always an accurate assumption. It is advisable to consider these tests as broad screening devices that allow us to categorize teeth as vital (responsive to stimuli) or non-vital (nonresponsive). Thermal tests are divided into the application of cold and/or heat.
False-Negative and False-Positive Sensibility Tests
All sensibility tests are subject to false-positive (i.e., a positive response from a necrotic pulp) and false-negative responses (i.e., a negative response from a vital pulp) [8, 12].
One study compared results of a cold test using ethyl chloride and the outcomes of electric pulp testing to the results of endodontic access and clinical verification of pulp vitality in 59 teeth of unknown pulpal status [12]. The probability that a negative test meant a true necrotic pulp was similar for the cold and electric tests (89 % vs. 88 %): the hot gutta-percha tests exhibited a much lower ability to detect a true negative (48 %). The probability that a positive test represented a true vital pulp was similar to the cold, electric, and hot gutta-percha test (90, 84, and 83 %, respectively). Overall, the cold and electric tests had similar accuracy values (86 % vs. 81 %), and both were more accurate than the heat tests (71 %).
Other studies have reported that the cold test is more accurate (80 %) in testing human advice of more than 1,000 teeth; 2 different electric testers each resulted in approximately 5 times higher false-positive results than did the cold test. Even when gingival controls were utilized, a commercial electric tester resulted in approximately twice the number of false-positive results as compared to a cold test [5
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


