
Fig. 23.1
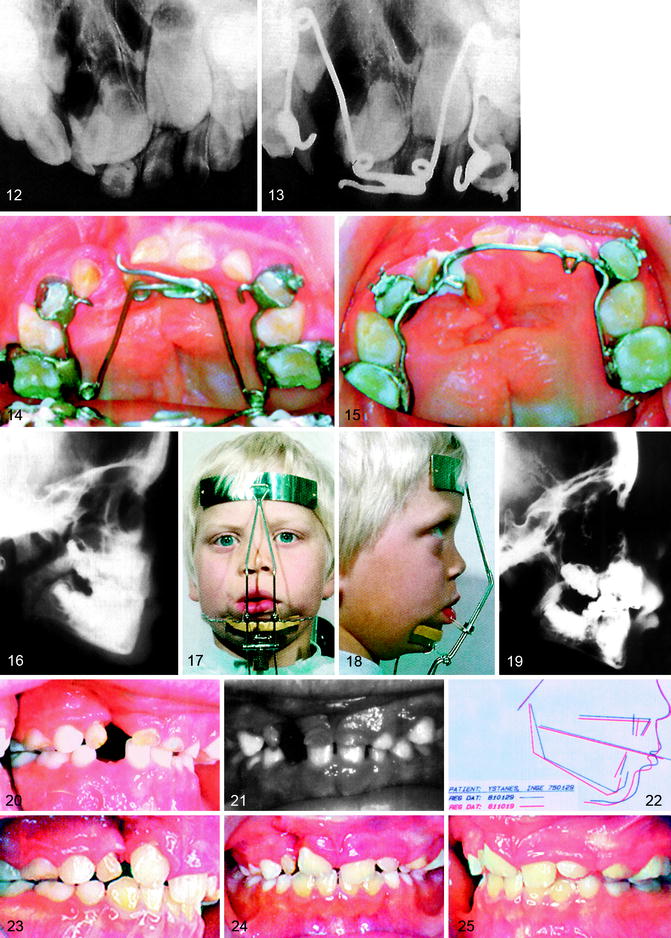
Complete UCLP, category 2A. (1–2) At birth, January 1975; (3–4) after presurgical orthopedics; (5–6) lip closure at age 3 months; (7–12) at 6 years moderate anterior and unilateral posterior crossbites with a slight concave profile; (13–27) interceptive orthopedics from age 6 years includes transverse expansion for 3 months using a quad-helix, (14) followed by protraction for 6 months using a facial mask, (17–18) and retention using a fixed palatal archwire (15) to encourage spontaneous eruption of upper permanent incisors into normal position. A nice dental smile was achieved without early orthodontic alignment of the upper incisors (28–33). Alveolar bone grafting at 10.5 years. Two right upper lateral permanent incisors erupted into the cleft area; (34) facial profile at 12 years (35–41); conventional orthodontics at 13.5 years lasting for 18 months. The two upper second bicuspids were missing, and the supernumerary right upper lateral permanent incisor was removed; (42–48) dental occlusion at 18.5 years; (49–50) cephalometric graphic analysis at 6, after interceptive orthopedics at 15 and at 18 years; (51–53) facial appearance at 15 years; (54–59) and facial appearance at 18.5 years
-
Eliminate anterior crossbite
-
Eliminate posterior crossbite
-
Create optimal space to permit spontaneous eruption of the incisors
-
Improve nasal respiration
-
Improve tongue placement
23.3.1.3 Alignment of Maxillary Incisors
In spite of achieving optimal dental space after transverse expansion, the permanent incisors often erupt rotated and retruded, tipped, or retroclined, placing them in crossbite. After transverse expansion, alignment of the permanent incisors is easily performed, giving the child a nice dental smile equal to that of his or her classmates (Fig. 23.2; in Fig. 23.1, incisor alignment was not needed):
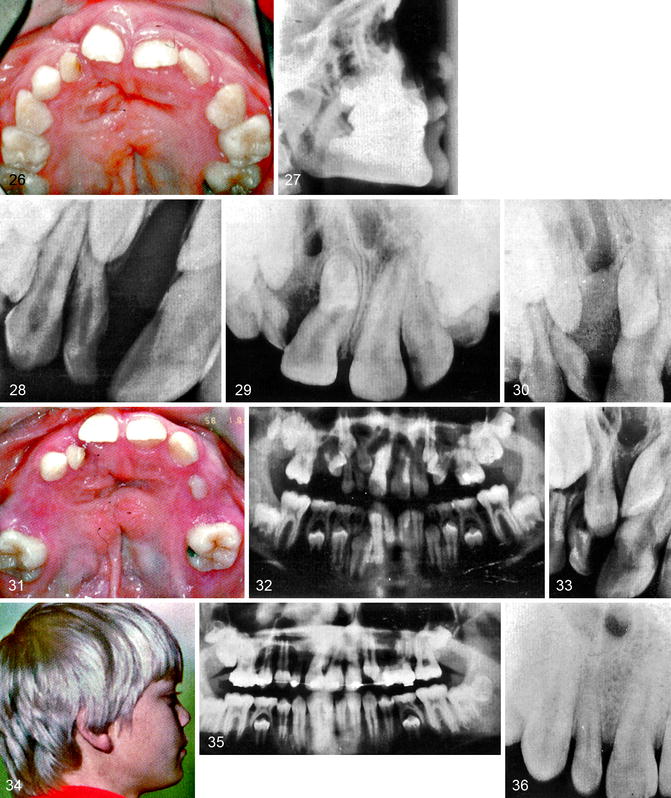
Fig. 23.2
(a–h) Interceptive orthopedics (Bergen rationale). (a, b) Transverse maxillary widening using a modified quad-helix appliance. (c, d) Followed by maxillary protraction with a facial mask (Delaire type). (e, f) Correction retained with a fixed palatal arch with brackets and tubes for early alignment of the upper incisors. Retention is utilized until deciduous anchor teeth are shed. (g, h) A nice dental smile as early as possible
-
Straightening of malpositioned incisors
-
Creating an optimal aesthetic incisor relationship to the facial midline
23.3.1.4 Secondary Alveolar Bone Grafting
The use of primary periosteoplasty at age 3 months was rejected after introduction of secondary bone grafting (Bergland et al. 1986). It is usually performed between 8 and 11 years of age with the orthodontist selecting the appropriate age:
-
Eliminate remaining bony clefts and improve bony support of contiguous teeth
-
Enhance orthodontic closure of the missing incisor space in the cleft area
-
Stabilize of separated jaw segments
-
Close oronasal fistulas
-
Provide bony support to alar base in cases with nasal asymmetry
-
Eliminating mucosal recesses
23.3.1.5 Conventional Orthodontics in the Permanent Dentition
The orthodontic treatment goals are similar to those for nonclefts, using the same general orthodontic principles utilized for noncleft patients: To establish ideal dental function, facial aesthetics, and speech. Extraction of mandibular teeth to compensate for a hypoplastic upper jaw is usually not indicated until after the critical mandibular growth period has passed. In CLP patients, a bonded palatal fixed retainer is often necessary after treatment involving arch expansion to avoid relapse of the corrected palatal arch form:
-
Improve the relationship of the lips
-
Achieve harmonious balance of the dentition in the opposing jaws
-
Achieve favorable skeletal maxillomandibular jaw relationship
-
Achieve normal incisor overjet and overbite
-
Correct dental axial inclinations
-
Avoid the use of artificial teeth
-
Achieve functional dental occlusion
-
Achieve optimal nasal breathing
23.3.1.6 Dental Adjustments at Ages 16–17 Years for Girls and 18–19 Years for Boys
In cases with major skeletal jaw discrepancies, orthognathic surgery may be needed to normalize the skeletal jaw relationship and achieve a well-balanced facial appearance with stable dental occlusion. If two or more teeth are absent in the same dental segment, a small bridge is normally needed. However, dental implants are likely to become an important aspect of future prosthetic replacements.
23.4 Outline of CLP Treatment Procedures in Bergen
To appreciate our treatment philosophy, a brief summary of the treatment approach and concepts of the Bergen Cleft Palate Center will be presented. Along with the Oslo CP Center, it serves a population of five million. Due to demographic distribution, many patients must travel distances up to 2,000 km to either center. Hardships are compounded by the need to travel in very cold weather during winter; therefore, the planning and coordination of health services are crucial for optimal utilization of available resources. Treatment costs and travel expenditures are covered by the government’s social security program. The Bergen CLP Team treats about 55 newborn babies yearly. Treatment procedures are coordinated between the Department of Plastic and Reconstructive Surgery, University Hospital of Bergen; the CLP Center at the Department of Orthodontics and Facial Orthopedics, Faculty of Medicine and Dentistry, University of Bergen; and the Eikelund Center for Speech Pathology.
23.4.1 Plastic Surgery
Since 1986, in complete clefts of the lip and palate, a Millard lip closure is performed at 3 months combined with a single-layer vomerplasty for closure of the anterior part of the palate. The soft palate and isolated palatal clefts are closed at 12 months using a von Langenbeck technique. Alveolar bone clefts are left open until secondary bone grafting at 8–11 years of age. Between 1971 and 1986, the lip closure was combined with a periosteoplasty of the cleft alveolar process (Schjelderup and Johnson 1983).
23.4.2 Interceptive Orthopedics
23.4.2.1 Protraction Facial Mask
Extraoral heavy forces from a facial mask directed forward and downward from the maxillary cuspid area have been shown to correct midfacial retrusion at an early age (Delaire et al. 1972, 1976; Tindlund 1987, 1989, 1994a, b; Tindlund and Rygh 1993a, b; Tindlund et al. 1993a, b, 1994). Protraction from the maxillary cuspid area produces an adequate horizontal and vertical force to increase midfacial vertical height as well as anteroposterior length. In some instances, it also can reduce an anterior open bite by lowering the palatal plane. For this reason, early correction of anterior and/or posterior crossbites during the deciduous and mixed dentition is highly recommended:
Bergen rationale:
1.
Transverse expansion coupled with
2.
Protraction of the upper jaw and
3.
The use of fixed palatal arch retention after treatment
When considering a treatment plan for young children who travel long distances, it is important to consider patient comfort as well as treatment efficiency.
In cases of marked midfacial retrusion, interceptive orthopedics is started at 6 years and often lasts for 15 months with an average of six visits (two visits for a transverse expansion of about 10 mm during a 3-month period and an additional four visits for the use of protraction forces for 12 months).
23.4.2.2 Quad-Helix Spring (with Four Bands and Hooks)
A fixed palatal expansion appliance can be easily combined with the use of an extraoral facial mask (Figs. 23.1 and 23.2) (Rygh and Tindlund 1982) providing:
1.
Controlled transverse expansion when needed
2.
Adequate fixation for anterior protraction by a facial mask
3.
Use with edgewise appliance for the alignment of incisors
4.
Well tolerated by small children without sedation, causing a minimum of discomfort
5.
Minimum of chair time
6.
Can be easily kept clean
The creation and use of a modified quad-helix [Rocky Mountain: maxillary quad-helix. 0.38 (0.985 mm) Blue Elgiloy (Ricketts)] appliance (Rygh and Tindlund 1982) is shown in Fig. 23.3. Four preformed bands with brackets or tubes are placed on the second deciduous molars and deciduous cuspids and are soldered to the quad-helix spring. The first deciduous molars serve as additional anchorage. Permanent molars are banded only when the second deciduous molars are missing. Hooks for elastics are positioned mesiolingually to the cuspid bands. The elastics are attached to the protraction facial mask (Fig. 23.2c, d). The elastic forces are directed forward and downward from the anterior maxillary segment, resisting the normal counterclockwise rotational effect. The quad-helix appliances when used with brackets and tubes permit alignment of upper incisors after their eruption (Figs. 23.1 and 23.3j–l).
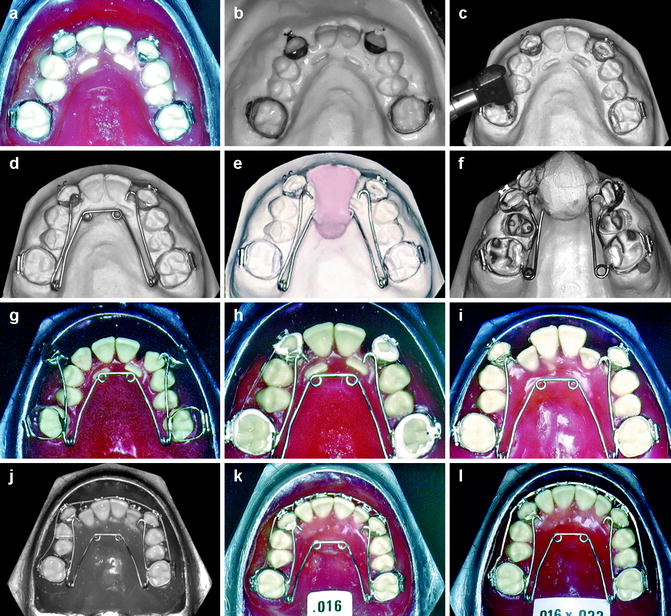
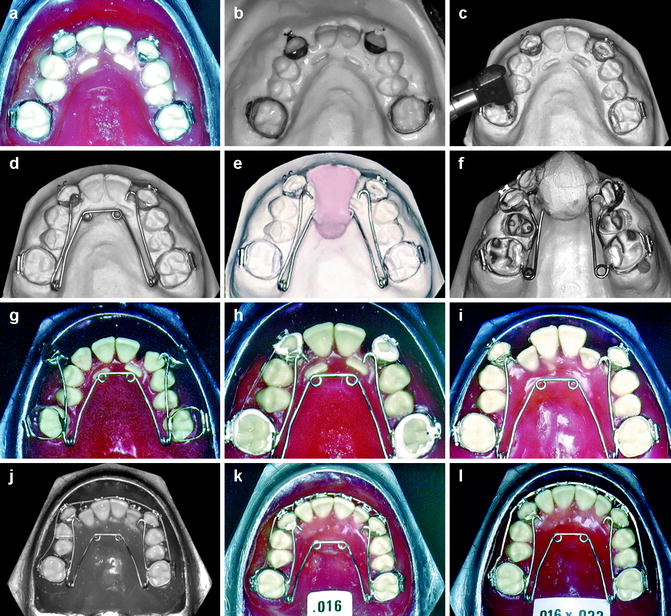
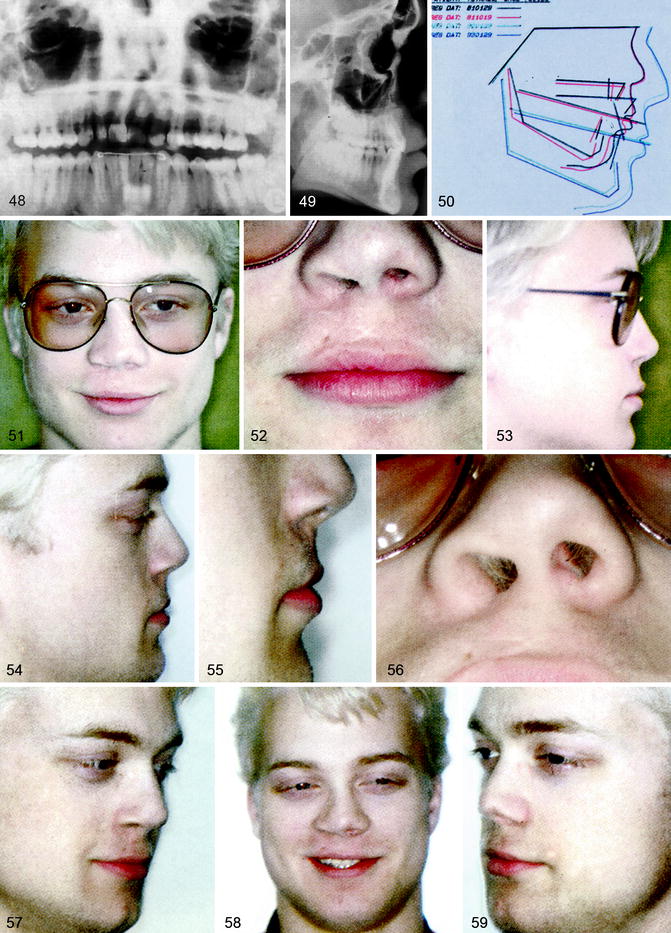
Fig. 23.3
(a–l) Fabricating a modified quad-helix appliance. (a, b) Bilateral posterior crossbite with lack of space for erupting lateral permanent incisors. Bands with brackets or tubes are fitted to the upper deciduous cuspids and deciduous second molars and carefully replaced into an alginate impression. (c) Plaster removed underneath soldering zones. (d) Quad-helix arms are precisely adjusted. (e, f) Quad-helix arms are soldered to all four bands. (g) Each arm is individually activated. (h) Cemented. (i–k) Combined with round labial arches for alignment of incisors. (l) Labial incisor root torque with rectangular archwire
23.4.2.3 Transverse Expansion
The modified quad-helix appliance is removed from the teeth and adjusted and activated at 6-week intervals (Fig. 23.2a, b). A resiprocal force of about 200 g on each side is optimal. The arch increases in width approximately 3 mm per month, irrespective of cleft type (Tindlund et al. 1993b). The cuspid segments often need more expansion than the molar area. Because there is a great tendency for relapse, overexpansion is necessary.
With transverse expansion of the maxillary arch, a downward clockwise rotation of the mandible occurs without any forward movement of the maxilla (Tindlund et al. 1993b). By comparing the use of fixed quad-helix appliances with removable expansion plates on noncleft patients, Hermanson et al. (1985) found that a fixed quad-helix appliance was more effective with fewer visits, less costly, and required shorter treatment time. Further, a removable plate would not readily resist the forward-downward traction to the cuspid area from a facial mask. As a rule, transverse expansion is completed before protraction is started.
23.4.2.4 Protraction
The quad-helix appliance is formed to make passive contact with the incisors, by bends or by a soldered-on extension (Fig. 23.2a, b). In cases where no transverse expansion is needed, or if the quad-helix spring is inconvenient after the expansion period, a simple palatal arch is soldered to four bands on second deciduous molars and cuspids (Fig. 23.2e, f). The intraoral appliance is used as anchorage for the facial mask (Scheu: Great Lake Reversed Pull Face Crib, 2500.1 small) (Fig. 23.2c, d). No other mask fixation is needed other than the two intraoral elastics [Unitek: Latex ex-oral 1/4”LGT; Unitek/3M: “Fran” 8oz. 1/4” (404–736)] from hooks in the cuspid areas. The force used for facial protraction is about 350 g on each side, totaling 700 g. The facial mask is used mainly at night for 10–12 h. Sleeping disturbances have not been reported. Patient cooperation is excellent in almost all cases. Within a few days, the children manage to put on the mask themselves, and complaints about soreness are very rare. It is important that the elastics are attached to the anterior segment and inclined downward and forward about 15° to the occlusal plane. Several facial masks of various designs are now available. If the use of protraction forces is delayed until the permanent incisors are fully erupted, elastic forces from hooks placed on the arch wire between the lateral incisor and cuspid area may be utilized. In most cases, the incisors should be advanced bodily to obtain surface bone deposition at subnasal (A-point) by use of edgewise arch wires with labial root torque (Fig. 23.3l).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


