Plan Your Work, Then Work Your Plan
The history of diagnosis and treatment planning has followed an interesting trail over the past 100 years. From Angle’s early commitment to nonextraction treatment and his battles with Calvin Case1,2 to Tweed’s extraction philosophy in the midtwentieth century, the discussions have continued. More recent appliances (fixed and removable) and treatment philosophies are promoting nonextraction treatment. Today, the debate concerning nonextraction treatment versus extraction treatment continues.
In our practice in Arlington, Texas, approximately 85% of patients are treated without extraction. The average number of extraction cases in the United States is about 20% of all patients treated, with some individual orthodontists extracting up to 50%. A percentage of these cases might be considered borderline. Of course, worldwide differences in patient characteristics, such as skeletal patterns, tooth sizes and shapes, and soft tissue profiles, etc, could change these percentages significantly.
The following eight factors help to clarify the sometimes difficult treatment decision between extraction and nonextraction:
1. Facial and muscle patterns
2. Mandibular functional patterns
3. Tooth size and form
4. Arch length discrepancy
5. Unusual eruption patterns
6. Growth
7. Habits
8. Compliance
“Begin with the end in mind,” is another Stephen Covey3 truism. However, it is necessary to first establish goals and understand how they can be achieved. The ends, or goals, of treatment were discussed in detail in principle 4. To ensure that these goals can be achieved, orthodontists must discipline themselves to compile high-quality diagnostic records. The quality of patients’ records can be a direct reflection of the quality of the treatment provided (Fig 5-1).
Fig 5-1 A bright and colorful room displaying a Peter Max painting of the American flag serves as a positive setting for the patient during diagnostic record taking.
Chapter 4 in my original book4 details the fundamentals of diagnosis and treatment planning. The remainder of the present principle discusses additional factors that help to complete the process.
Cephalometrics
No matter what cephalometric analysis is used, three basic measurements must be obtained from the cephalometric tracing before a proper treatment plan can be produced:
1. Sagittal skeletal pattern
2. Vertical skeletal pattern
3. Incisor position
Sagittal skeletal pattern
The first cephalometric determination to be made is the patient’s skeletal type: Class I, II, or III skeletal pattern. Addressing the skeletal discrepancy at the beginning of treatment will enable the clinician to determine the necessary type and direction of orthopedic force. The measurements sella-nasion–point A (SNA), sella-nasion–point B (SNB), point A–nasion–point B (ANB), and nasion–point A– porion (NA-Po) and the Wits appraisal can help to provide the answer.
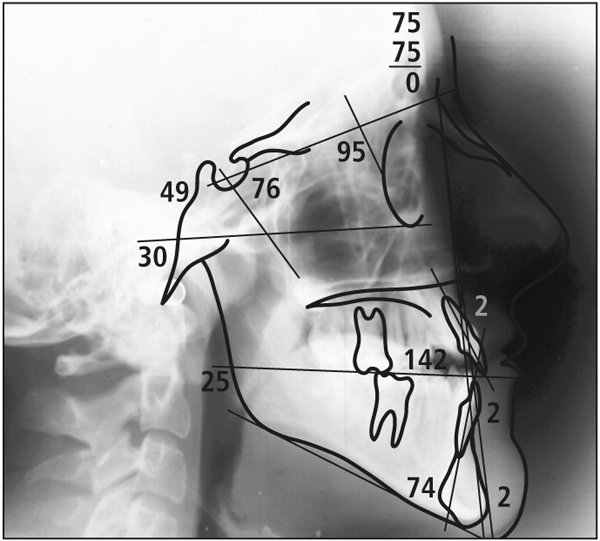
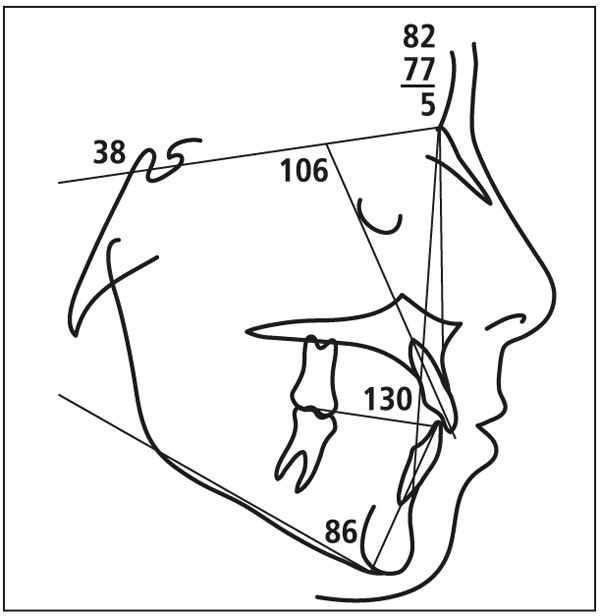
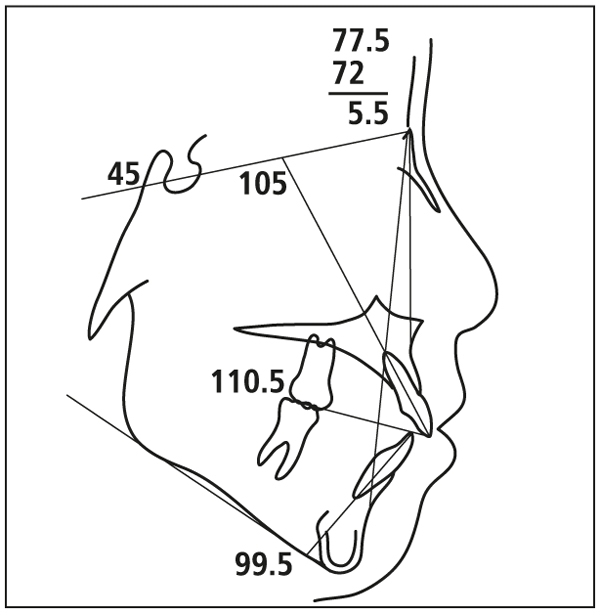
In most cases, the ANB angle will provide the needed information. For a patient with a Class II skeletal pattern, it is necessary to determine if the patient exhibits maxillary protrusion or mandibular deficiency. The angles SNA, SNB, and ANB are very helpful in this diagnosis. For Class III patients, the Wits appraisal may be more meaningful, especially in those with high-angle Class III malocclusions (Fig 5- 2).
Fig 5-2 To determine Class III skeletal patterns cephalometrically in high-angle cases, the Wits appraisal is often more accurate than point A–nasion–point B (ANB).
Vertical skeletal pattern
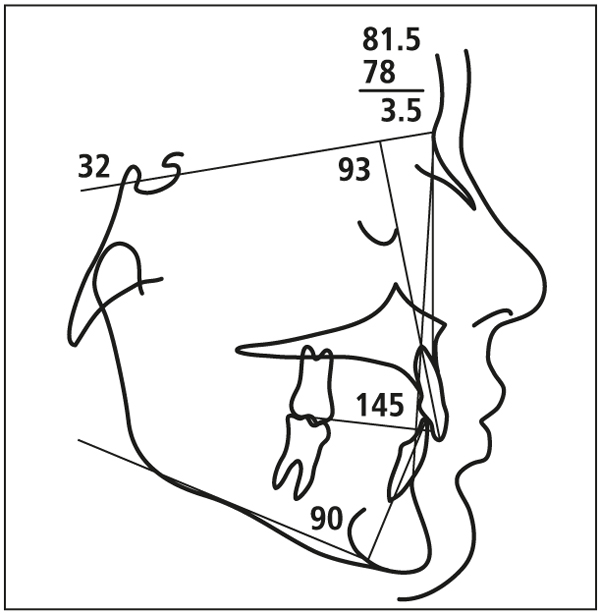
Whether the patient has a high-, medium-, or low-angle skeletal pattern will also influence treatment decisions. The sella-nasion–mandibular plane (SN-MP), Frankfort mandibular plane angle, occlusal plane–mandibular plane, and y-axis are measured and compared to provide an accurate assessment of the patient’s skeletal vertical pattern.
In keeping with the “keep it simple, stupid” (KISS) principle, SN-MP is routinely used as the reference measurement. A simple analysis follows:
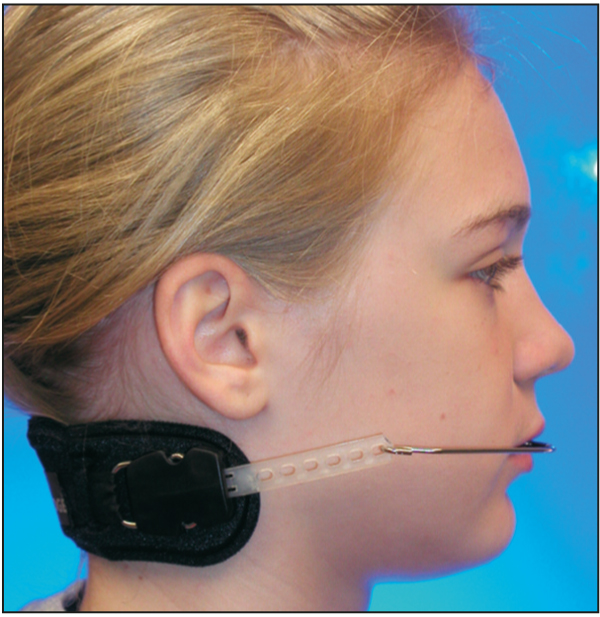
1. When the SN-MP angle is 35 degrees or less (Fig 5-3), Class II skeletal patterns can best be treated with a cervical facebow (Fig 5-4). During the treatment of a skeletal Class III patient using a face mask, the force vector is often directed at 45 degrees in relation to the occlusal plane, depending on the smile line.
2. If the SN-MP angle is 36–41 degrees (Fig 5-5), the vertical dimension is best managed with the use of a combination-pull facebow (occipital and cervical straps) in patients with a skeletal Class II relationship (Fig 5-6). The elastic force vector of a face mask used to treat high-angle Class III patients should be directed parallel to the occlusal plane to prevent the extrusion of the maxillary teeth.
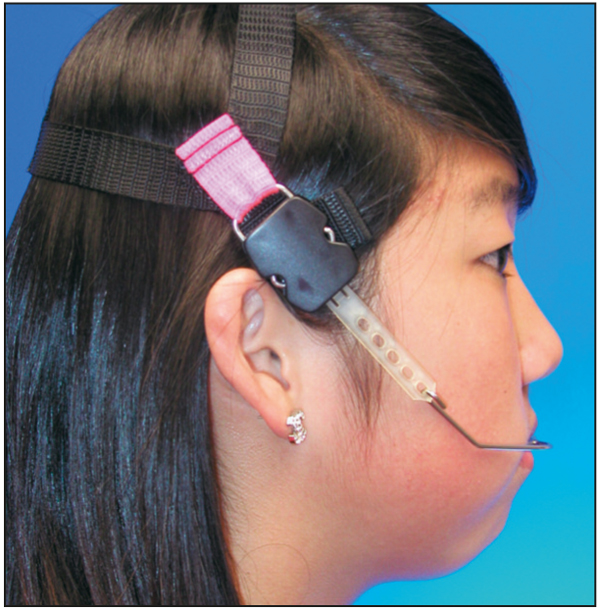
3. If the SN-MP angle is 42 degrees or greater (Fig 5-7), every effort is made to inhibit further vertical growth of the maxilla. A high-pull facebow combination is prescribed for patients with a high-angle skeletal Class II pattern (Fig 5-8). If the diagnosis is a high-angle skeletal Class III pattern, the elastic force vector of the face mask is directed almost parallel to the occlusal plane. For high-angle patients with arch length discrepancies, extraction therapy may be indicated.
Fig 5-8 Soft tissue profile of the same patient wearing a high-pull facebow. Notice how the outer bow is bent at the first molar area.
Incisor position
The third factor analyzed with the cephalometric tracing is the position of the incisors.
Mandibular incisors
As stated in chapter 4 of The Alexander Discipline,4 control of the mandibular incisor position is critical for long-term stability. Tweed and others have demonstrated that the outcome is unstable when these incisors are advanced. Yet in contemporary orthodontics, the desire to treat all patients without extractions has led to the routine, indiscriminate flaring of mandibular incisors. In a future volume of this series, the danger of such treatment with regard to postorthodontic stability will be thoroughly explored.
Clinical experience with both extremes of incisor position indicates that:
1. In most cases, the best and most stable position for mandibular incisors is the position in which the patient presents. Maintaining these teeth in their original positions is the goal. In high-angle cases, the incisors may be more upright. Treatment of low-angle deep bite cases may require that these incisors be proclined from their original position.
2. In extraction cases, mandibular incisors are usually uprighted. If an adequate interincisal angle is also achieved, this treatment is stable. The soft tissue profile must be evaluated carefully when the incisors are uprighted so that a concave profile is not produced.
3. Studies have indicated that mandibular incisors can be advanced up to 3 degrees and remain stable—the 3-degree rule. Beyond that critical 3 degrees, instability is more likely. Perhaps the only time that mandibular incisors are intentionally advanced is when they are initially abnormally lingually inclined. This situation is often found in patients with Class II division 2 or Class II division 1 deep bite. Advancing the incisors in these patients will improve the interincisal angle and soft tissue profile. The patient must be advised of the need for lifetime retention to ensure long-term stability because the 3-degree rule has been violated.
Maxillary incisors
With the exception of Class II division 2 malocclusions, most maxillary incisors are positioned almost normally at the beginning of treatment. As with the mandibular incisors, the goal is to keep them in that original position. Maintenance of good torque control of the maxillary incisors, along with the mandibular incisors, will result in a balanced interincisal angle. This is critical for acceptable functional occlusion and long-term stability. Often in patients with Class II division 1 patterns, these incisors are flared and spaced. When the spaces are closed and the arch is consolidated, the incisors will be uprighted to normal positions.
Study Casts
Maxillary intermolar width
The maxillary intermolar width (transverse discrepancy) is measured from the lingual central grooves at the cervical line on the maxillary first molars. If the maxillary transverse dimension is narrow (less than 33 mm), then rapid palatal expansion is routinely performed to provide adequate arch width. Moreover, additional maxillary arch length is gained, so that a borderline extraction case often becomes treatable without extraction.
Mandibular arch length discrepancy
Too often, the decision to extract teeth is focused only on the tooth size–arch length discrepancy. Although a critical issue, other factors must be considered before an irreversible extraction decision is made. These factors are discussed in principles 17 and 18.
Panoramic Radiograph
Assessment of the panoramic radiograph must focus on areas where problems can occur. The interproximal bone level must be checked, especially in adult patients. The root shape and position are critical to observe. Occasionally, an angulated or curved root is revealed by the radiograph (Fig 5-9)./>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses