Establish Goals for Stability
Few things in orthodontics are truly new. The basic method of tooth movement has changed little since the early 1900s. Of course, the Alexander Discipline has benefited greatly from improvements in materials and procedures, such as newer metallurgy and bracket bonding. Specific approaches, techniques, and materials will continually change, but the fundamental truths will always remain the same.
Early in the history of orthodontics, just getting the teeth to move must have been very exciting. The idea was to get the teeth “straight.” History has shown, however, that this goal is not enough. That word relapse has continually raised its ugly head. Getting the teeth straight was very important, but time has shown that keeping them straight is another challenge. Therefore, the next level of orthodontics is to keep the teeth straight.
During this past century, orthodontists have learned some facts regarding the placement of teeth at the end of treatment that will affect the total outcome of the treatment. One truth that cannot be debated is the precept “Primum non nocere” (“First, do no harm”). It is possible for orthodontic treatment to cause plenty of harm: overexpansion, flaring, extrusion, poorly tipped roots, and the list goes on. It is the responsibility of the orthodontist to position the teeth so that the chances for healthy, stable results are more favorable. For example, orthopedic forces should control and/or encourage good growth. Orthodontic forces should not move the teeth into positions that will be unstable.
There are many unresolved issues in orthodontics:
- Are there limits or boundaries in orthodontics?
- What is the “standard of care”?
- How much of orthodontics has become a science, rather than remaining an art?
- Has the specialty of orthodontics matured to the point at which the majority of orthodontists would examine the same patient and agree on the goals and specific treatment plan?
Role of the Patient
The most important factor in the formula for success is the patient. Three factors will always prevent orthodontics from being an exact science: the patient’s growth, habits, and compliance.
Predicting the cephalometric skeletal changes that will result from orthodontic or orthopedic forces is at best an erratic science. Treating growing children is like attempting to hit a moving target. The amount and direction of growth will have a significant role in determining the result. When a specific orthopedic force is applied, each human being can respond differently.
In general, orthopedic improvement can be accomplished in most growing patients. The sagittal skeletal dimension can be altered favorably in growing patients. Vertically growing patients with a high mandibular plane angle can be improved, although their direction of growth is not as favorable as that of patients with a lower mandibular plane angle. The most predictable orthopedic improvement can be observed when the transverse dimension is expanded.
Habits such as thumbsucking, mouth breathing, bruxism, and tongue thrusting can have detrimental effects on the treatment outcome, regardless of the skeletal pattern.
In most patients, however, the key to success is patient compliance. As discussed in principle 20, orthodontists are only as good as their patients.
Evidence-Based Orthodontics
In one of his lectures many years ago, Dr Fred Schudy from Houston, Texas, jokingly stated, “Figures don’t lie … but liars figure.” When discussing the goals in orthodontic treatment, I rely on very specific research performed by various people. Residents from the Baylor College of Dentistry orthodontic department have performed much of my research, many times using patient records from my office. This could create a conflict of interest if I had personally selected these records. To prevent this from occurring, I have adopted some rules for use of my case records.
The resident is given complete access to all records. There is no “cherry picking”; I have never selected the patient records to be used in any study. The residents select the cases that they will study based on their study protocol. They are not permitted to remove any records from the office. Orthodontic residents from other universities in the United States and from around the world have studied these records. This is important so that the doctors around the world who hear the results of these studies can be confident of their objectivity.
It is incumbent on all orthodontists to practice evidencebased orthodontics, whenever that evidence exists. All results discussed in research must be accompanied by statistical data. It is the goal to arrive at a statistically valid mean. That mean will always have a range, however (the standard deviation). The numbers and measurements presented in research are often just guidelines, not absolute values. As Dr Peter Buschang says, “There is no such thing as a ‘mean’ patient.” As always, there will be exceptions to every rule; however, the principles advocated in this book are an attempt to make orthodontics more of a science and less of an art.
The following goals, when achieved, have been found to help create healthy, esthetically pleasing, and stable results:
- Mandibular incisors balanced on basal bone
- Maxillary incisors positioned to create a good interincisal angle
- Canine expansion prevented
- Proper artistic root positioning
- Upright mandibular first molars
- Normal overbite and overjet
- Functional occlusion in centric relation
The 15 Keys to Orthodontic Success
Throughout the history of modern orthodontics, the diagnostic records of the patient have been used to evaluate the patient’s problems and determine the resultant treatment plan. These records consist of a lateral cephalogram, panoramic radiograph, study casts, intraoral photographs, and facial photographs. From each of these records, critical information is obtained and then evaluated. After much research and evaluation of particular measurements from many patients’ long-term records, certain norms appear evident; these norms have helped to establish set goals for the treatment of patients.
Among all of the possibilities, 15 measurements taken from the diagnostic records can provide a brief yet accurate determination of goals necessary to achieve successful treatment and long-term stability for the individual patient.
Cephalometrics: The tetragon-plus analysis
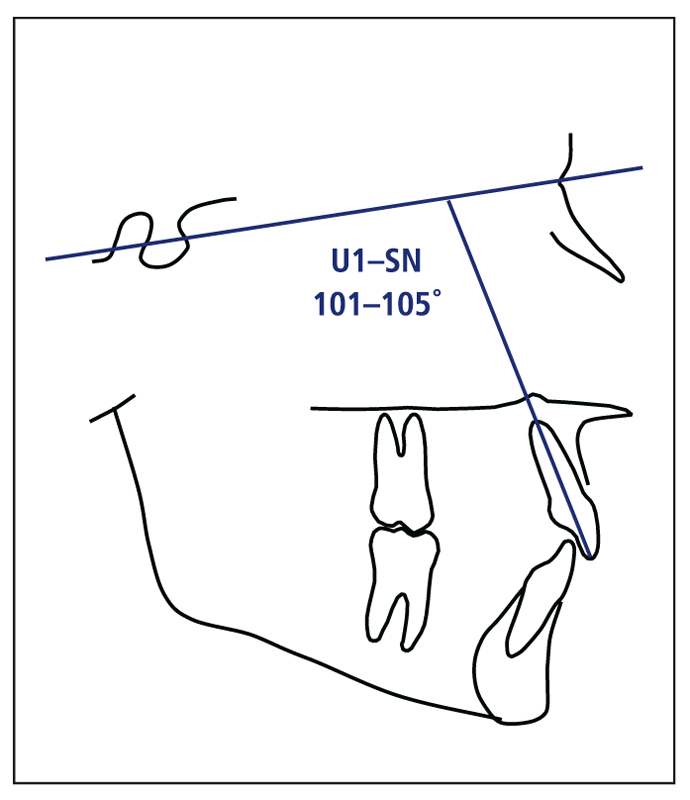
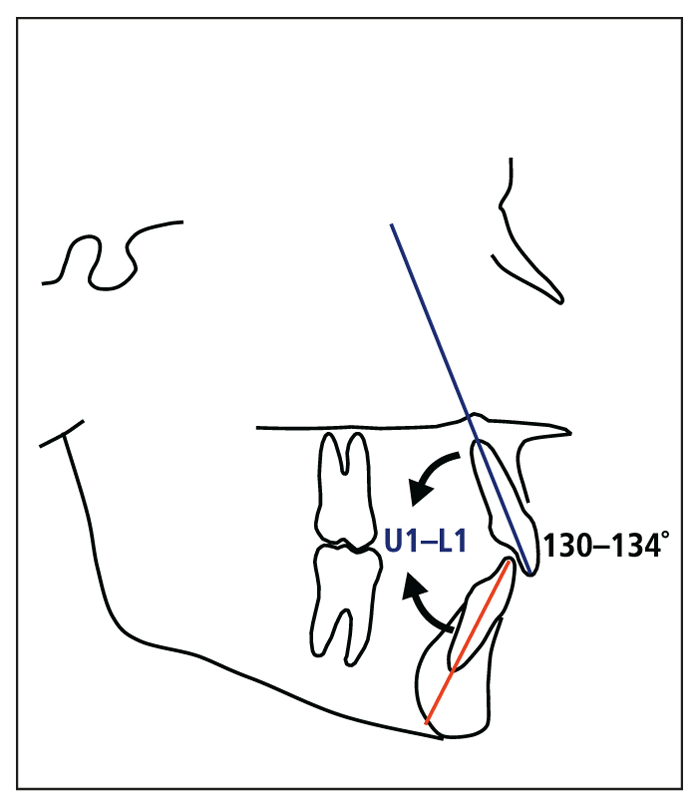
Certain established cephalometric measurements can be influenced and/or controlled during treatment. Among these are the mandibular incisor–mandibular plane (IMPA), or the mandibular incisor inclination; sella-nasion–mandibular plane (SN-MP), or the mandibular plane angle; maxillary incisor–sella-nasion (U1-SN), or the maxillary incisor inclination; and maxillary incisor–mandibular incisor (U1-L1), or the interincisal angle. When these four measurements are combined, a four-sided figure, or tetragon, is formed (Fig 4-1). A key to successful treatment can be the control of these angles or change to more ideal positions.
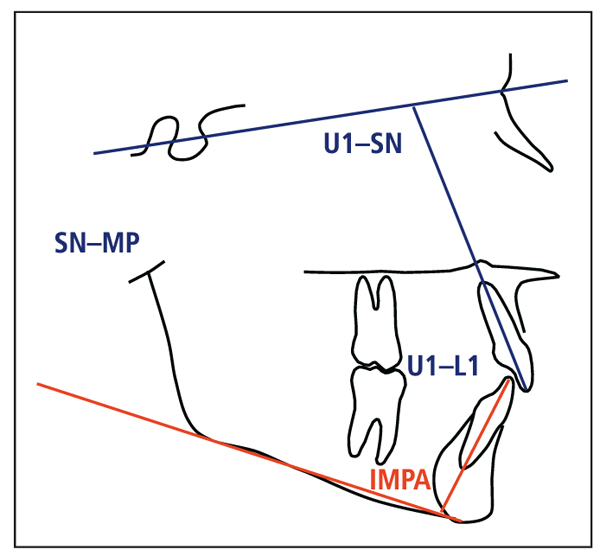
Fig 4-1 The tetragon: sella-nasion–mandibular plane (SN-MP); maxillary incisor–sella-nasion (U1-SN); maxillary incisor–mandibular incisor (U1-L1); mandibular incisor–mandibular plane (IMPA).
1. Mandibular incisor inclination
Three possibilities exist for an ideal posttreatment value for IMPA (Fig 4-2):
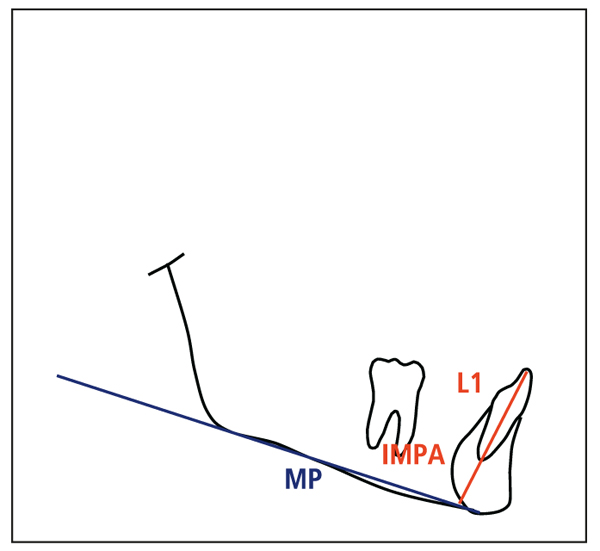
Fig 4-2 Mandibular incisor inclination: mandibular incisor (L1); mandibular incisor– mandibular plane (IMPA); mandibular plane (MP).
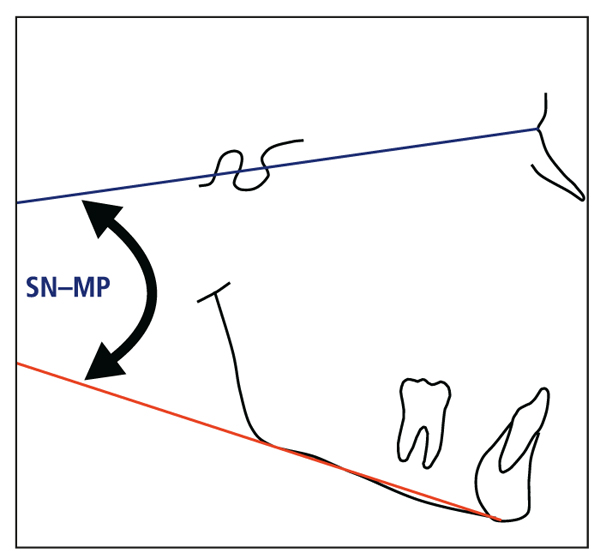
Fig 4-3 Mandibular plane angle (skeletal vertical control): sella-nasion–mandibular plane (SN-MP).
- In most nonextraction treatments, the mandibular incisors should be maintained within 3 degrees of their original position (the 3-degree rule).
- In patients with a deep bite, especially a division 2 deep bite, the mandibular incisors are often inclined lingually and should be advanced, sometimes significantly.
- In patients with bimaxillary protrusion, the incisors are often significantly flared. In these patients, the incisors should be retracted more than 3 degrees.
Because the majority of patients are treated without extraction, it is critical to control the position of the mandibular incisors and prevent labial flaring. This is perhaps one of the most common mistakes made in orthodontics because many clinicians fail to address this issue. Almost all studies indicate that violating the 3-degree rule (inclining the incisors more than 3 degrees from their original position) will result in a higher incidence of relapse in the long term.1–3 Clinically, –5-degree torque in the mandibular incisor bracket will help to control this critical position. This is discussed in greater detail in principle 17.
2. Mandibular plane angle
The goal is to maintain the mandibular plane angle (SNThe goal is to maintain the mandibular plane angle (SN 3). In very low-angle cases, the mandibular plane may have to be increased during treatment. In patients with average vertical dimensions and good growth potential, orthopedic forces, if managed properly, can be very successful without significantly increasing the vertical plane.
The problem arises when the patient presents with a high-angle vertical pattern. In such cases, maxillary molar control is critical to prevent molar extrusion.4 For example, if headgear is misused and only a cervical neck strap is prescribed for high-angle patients, the maxillary molars may be extruded, causing vertical openings. Specific controls are discussed in later principles.
3. Maxillary incisor inclination
In normal skeletal patterns, the maxillary incisor should be inclined 101 to 105 degrees relative to SN (Fig 4-4). An exception to this rule applies to patients with a high mandibular plane angle. Often in these types of cases, the mandibular plane angle. Often in these types of cases, the SN angle. In contrast, when a patient has a low-angle pattern, the maxillary incisor inclination can often be greater.
Controlling the inclination (torque) of the maxillary incisor is critical to the creation of adequate incisal guidance, which leads to the fourth angle in the tetragon. With the Alexander bracket prescriptions, incisor inclination (torque control) can be accomplished with a 0.017 × 0.025-inch stainless steel archwire in the pretorqued 0.018-inch slot anterior brackets.
4. Interincisal angle
The accepted angle between the maxillary and mandibular incisors (U1-L1) is from 130 to 134 degrees (Fig 4-5). As with the other measurements, U1-L1 may vary, depending on an individual’s skeletal vertical pattern. Although orthodontists have limited options for positioning of the mandibular incisors, the maxilla allows more freedom in the positioning of the maxillary incisors. However, the final position of the maxillary incisors is directly related to the position of the mandibular incisors.
5. Tetragon plus
Additional information garnered from the cephalogram is referred to as tetragon “plus.” T/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses