People with disabilities and other special needs present unique challenges for oral health professionals in planning and carrying out dental treatment. This article presents a schema for planning dental treatment that encourages the oral health provider to fully consider multiple medical, social, psychologic and dental findings when preparing treatment recommendations for a patient with special needs. If these factors are fully integrated, the resulting treatment recommendations provide the best chance of helping the individual achieve and maintain a lifetime of oral health
There are many terms used to describe people who have trouble receiving dental treatment in a routine manner. These include “people with special needs,” “children with special health care needs,” “people with disabilities,” “people with complex needs,” and other terms. Some of these terms, such as “children with special health care needs” or people with “developmental disabilities” have definitions that are found in federal regulations and used for collection of data and funding purposes. Other commonly used terms such as “people with special needs,” “people with disabilities,” or “people with complex needs” do not have generally agreed upon definitions, but are useful in describing populations who present challenges in providing oral health services. For the purpose of this clinically focused article the terms “people with special needs,” “people with disabilities,” and “people with complex needs” are used interchangeably and are defined as people who have difficulty accessing dental treatment services because of complicated medical, physical, social, or psychologic conditions. This article discusses considerations in planning dental treatment for people with special needs.
The population of people with special needs is increasing dramatically
It has been established that people with chronic medical illnesses, developmental disabilities, and psychosocial issues experience more oral health care problems than others who do not suffer from these conditions. Advances in medicine have increased the likelihood that people today live longer with comorbidities that would previously have shortened their lifespan. Patients with special needs have also seen a gain in life expectancy. Thirty years ago, for example, the typical person with Down’s syndrome would have a life expectancy of roughly 12 years compared with 60 years today. Because of these advances, the number of people with special needs who need oral health services is growing dramatically. According to United States Census 2000, roughly 50 million people, or almost 20% of the population, has a long-standing condition or disability. In addition to those with chronic morbidities or disabilities, the aging population of America also has problems with obtaining basic oral health care services. 3.6% of noninstitutionalized United States citizens over age 65 report needing care but are unable to obtain it. The 2000 Surgeon General’s Report on Oral Health indicates that people with developmental disabilities are at a significant disadvantage in obtaining hygiene services, have worse hygiene than their non-disabled counterparts, and have an increased need for periodontal treatment than the general population. Untreated dental disease has been found in at least 25% of people with cerebral palsy, 30% of those with head injuries, and 17% of those with hearing impairment. A study commissioned by the Special Olympics concluded that individuals with intellectual disabilities have poorer oral health, more untreated caries, and a higher prevalence of gingivitis and other periodontal diseases than the general population. There is also a relation between disability and income. People from lower socio-economic groups and those covered by Medicaid have more dental disease and receive fewer dental services than the general population and many individuals with disabilities are in these lower socio-economic groups. The large increase in the number of people with special needs now living in society and seeking dental treatment provides new challenges for dental providers. Among the challenges are those related to developing and implementing appropriate plans of treatment for these individuals (Special Olympics, unpublished data, 1999).
Challenges in providing oral health care for people with disabilities
There are numerous challenges in providing oral health services for people with special needs that go beyond the normal considerations for other populations. These challenges require oral health professionals to have extraordinary training, empathy, patience, and the desire to be successful. There are a number of areas where providing oral health services for these populations presents unique challenges.
First there is a need to understand and to be prepared to work with people with a wide variety of general health conditions. Although oral health professionals do not need to have complete knowledge of every general health condition that their patients present with, it is essential that they have the knowledge and experience to gather and apply the information they need. This implies the training and ability to function in health care teams and get consultations from physicians, social workers, and other general and social service professionals.
Oral health professionals should be well acquainted with the social service agencies, community living arrangements, and advocacy organizations operating in their community and the social context in which oral health services take place. They also need to understand and use appropriate language when interacting with individuals with special needs and their caregivers. There is a growing movement advocating the use of “People First” language. This language emphasizes the fact that disability is a part of the human condition and all people want to be described by their abilities rather than labeled by their disabilities. An oral health professional who does not understand this language and refers to people he treats as “the handicapped patients I see” risks alienating the individual, their caregiver, and those advocating for full inclusion in our society.
Oral health professionals must also realize the extraordinary vulnerability of people with special needs to abuse and neglect in our society. They need to understand how to recognize abuse and neglect and their role as mandated reporters. Oral health providers are health professionals and as a part of the health care team they may find that their patients are depressed, suicidal, or unable to cope with various living challenges. They have an obligation to intervene, provide basic diagnosis and counseling and make appropriate referrals for follow-up of these situations.
Oral health professionals need to understand how to prevent oral diseases in people with various disabilities. There are special challenges presented by working with someone where communication and even procedures need to be performed by a third person, the caregiver. Some people have limited physical ability to perform oral hygiene procedures and “partial participation” programs need to be designed and performed. This term refers to having the individual do as much as they are able to, but having a caregiver ensure that needed prevention procedures are completed. There are numerous informational, physical, and behavioral obstacles to be addressed. These are described in detail in “Overcoming Obstacles to Dental Health,” a training package for caregivers of people with disabilities. In addition to this package, there is a large body of literature that describes the challenges and techniques for helping people with special needs prevent oral diseases.
Challenges in providing oral health care for people with disabilities
There are numerous challenges in providing oral health services for people with special needs that go beyond the normal considerations for other populations. These challenges require oral health professionals to have extraordinary training, empathy, patience, and the desire to be successful. There are a number of areas where providing oral health services for these populations presents unique challenges.
First there is a need to understand and to be prepared to work with people with a wide variety of general health conditions. Although oral health professionals do not need to have complete knowledge of every general health condition that their patients present with, it is essential that they have the knowledge and experience to gather and apply the information they need. This implies the training and ability to function in health care teams and get consultations from physicians, social workers, and other general and social service professionals.
Oral health professionals should be well acquainted with the social service agencies, community living arrangements, and advocacy organizations operating in their community and the social context in which oral health services take place. They also need to understand and use appropriate language when interacting with individuals with special needs and their caregivers. There is a growing movement advocating the use of “People First” language. This language emphasizes the fact that disability is a part of the human condition and all people want to be described by their abilities rather than labeled by their disabilities. An oral health professional who does not understand this language and refers to people he treats as “the handicapped patients I see” risks alienating the individual, their caregiver, and those advocating for full inclusion in our society.
Oral health professionals must also realize the extraordinary vulnerability of people with special needs to abuse and neglect in our society. They need to understand how to recognize abuse and neglect and their role as mandated reporters. Oral health providers are health professionals and as a part of the health care team they may find that their patients are depressed, suicidal, or unable to cope with various living challenges. They have an obligation to intervene, provide basic diagnosis and counseling and make appropriate referrals for follow-up of these situations.
Oral health professionals need to understand how to prevent oral diseases in people with various disabilities. There are special challenges presented by working with someone where communication and even procedures need to be performed by a third person, the caregiver. Some people have limited physical ability to perform oral hygiene procedures and “partial participation” programs need to be designed and performed. This term refers to having the individual do as much as they are able to, but having a caregiver ensure that needed prevention procedures are completed. There are numerous informational, physical, and behavioral obstacles to be addressed. These are described in detail in “Overcoming Obstacles to Dental Health,” a training package for caregivers of people with disabilities. In addition to this package, there is a large body of literature that describes the challenges and techniques for helping people with special needs prevent oral diseases.
Developing a treatment plan for a person with special needs
The process of developing a dental treatment plan typically progresses through several phases. The first phase involves gathering data about the individual, which is then used to develop a diagnosis or set of diagnoses. A set of treatment recommendations are then determined, and discussed with the patient and/or their caregiver. After discussion, a plan of treatment is developed to address the various diagnoses. The patient or caregiver must be informed about the benefits, risks, and alternatives to all the treatment options. The process of obtaining informed consent for someone who cannot provide their own consent can be complex, but is beyond the scope of this article.
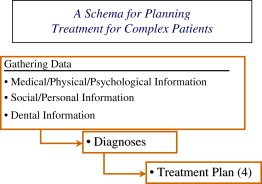
While the general schema described above for developing dental treatment plans is commonly followed by dentists for all patients, there are important elements within the three phases described above that may receive little attention for healthy patients with uncomplicated histories, yet are critical to consider for people with special needs. This article presents a “Schema for Planning Treatment for Complex Patients” which is diagrammed in Fig. 1 . The “(4)” after “Treatment Plan” in the diagram indicates that there are four distinct phases of the plan, which are discussed below.
Gathering data
The traditional format for gathering data about an individual’s health history follows the schema described in Box 1 . The process described here follows this format but places much greater emphasis on gathering data about the areas of family history and social history. These areas are often neglected when dentists gather data about patient’s health histories. As listed in Fig. 1 , the emphasis in gathering data for people with complex histories and treatment needs is on medical, physical, and psychologic information; social and personal information; and finally dental information. The order in which these areas are listed is designed to counteract the tendency of dentists to focus on dental history and problems first.
-
ID = identifying data (age, ethnicity, source of data)
-
CC = chief concern
-
HPI = history of the present illness
-
MH = medical history
-
DH = dental history
-
SH = social history
-
EX = examination (this includes clinical, radiographic, and laboratory examinations)
-
DX = diagnosis (or differential diagnosis)
-
P = plan (including phases, ethical considerations, and further diagnostic steps)
Box 2 presents a series of questions that can guide the oral health provider in gathering data of particular importance for a person with one or more disabilities. The questions are divided into four sections.
-
Medical information
- a.
What is the disability?
- b.
How severe?
- c.
What is the long- and short-term prognosis?
- d.
What treatment is being (or will be) given and what are the side effects?
- e.
What medications are being taken and what are the side effects?
-
Social/personal information
- a.
What is the effect of the disability(-ies) on the patient’s life?
- b.
What are the effects of the dental problems on the patient’s life?
- c.
What would the effect of dental treatment be on the patient’s life?
- d.
What is the person’s ability to understand, communicate, and perform procedures?
- e.
What support persons are available?
- f.
What are the expectations of the patient and support persons?
- g.
What financial support is available?
-
Dental information
- a.
What dental abnormalities are associated with the disability(-ies)?
- 1.
Do the abnormalities need treatment?
- 2.
What considerations are there in treating these abnormalities?
- 1.
- b.
What other dental problems exist?
- c.
How does the person’s disability(-ies) affect the delivery of dental services?
- 1.
What behavioral, psychologic, pharmacologic supports are needed?
- 2.
What position modifications are needed?
- 3.
What precautions or special procedures need to be employed?
- 1.
- d.
How does the disability and associated problems affect the maintenance of oral health?
- 1.
What oral hygiene procedures can and will be performed?
- 2.
How will dental appliances be tolerated and cared for?
- 3.
Will it be possible to establish a schedule of recall appointments which can be kept?
- 1.
- e.
What is the prognosis for the future?
- 1.
What is the prognosis for dental health and/or dental problems with and without treatment?
- 2.
What is the risk and benefit of each procedure that might be indicated?
- 1.
-
Treatment plan
- a.
What, when, how, and who for each of the following:
- 1.
Emergency treatment
- 2.
Preventive program
- 3.
Initial treatment
- 4.
Future maintenance treatment
- 1.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


