Intellectual and developmental disorders can severely impair a patient’s ability to communicate and socialize. Individuals with such disorders tend to have unusual ways of learning, paying attention, and reacting to different sensations. Symptoms can range from very mild to very severe. To properly treat these patients and, if necessary, refer them for appropriate medical care, dental professionals must be able to recognize the signs and symptoms of each patient’s specific disability. This article gives details about behavior associated with intellectual and developmental disorders and describes specific techniques for care that may be used routinely at home and carried into the dental setting.
Intellectual and developmental disorders (I&DDs) can severely impair a patient’s ability to communicate and socialize. Individuals with such disorders tend to have unusual ways of learning, paying attention, and reacting to different sensations. Symptoms can range from very mild to very severe. To properly treat these patients and, if necessary, refer them for appropriate medical care, dental professionals must be able to recognize the signs and symptoms of each patient’s specific disability. Treating patients with I&DDs can be both challenging and rewarding.
As a parent of a child with autism–pervasive development delay, which is one type of I&DD, I can offer a personal as well as a professional perspective. Living with an individual with an I&DD involves ongoing challenges that dental professionals are unlikely to face in the short time the patient spends in the dental office. This article gives details about behaviors associated with I&DDs—behaviors that caregivers come to understand through constant care and supervision—and provides specific techniques that may be used routinely at home and carried into the dental setting. Researchers have not sufficiently studied the effectiveness of many suggested treatment accommodations for this patient population. So, to effectively provide good dental care to such patients, dental professionals must learn through interviews with caregivers about which behavior management techniques are most effective for each individual patient.
Today, dental and dental hygiene programs offer little formal education specific to the care of patients with I&DDs. To make up for this virtual absence of educational preparation for the care of patients with special needs, Special Olympics initiated an effort that brought about a modification in the Standards of Accreditation of all dental and dental hygiene schools in the United States. Beginning in 2006, all schools considered for accreditation by the Commission on Dental Accreditation must offer didactic and clinical opportunities to better prepare dental professionals for the care of persons with intellectual and other developmental disabilities. While these standards are in place, many schools still struggle to meet all of the clinical requirements to include significant experiences with this patient population. In fact, in a recent study conducted at the University of Iowa, graduating dental students reported that their comfort level in treating patients who are mentally compromised was equal to their comfort level for treating patients who are drug users, who are jailed, or who have HIV. In addition, a Special Olympics study conducted by Reuters Health found that “more than half of medical school deans and dental school deans, respectively, said that their graduates were ‘not competent’ to treat patients with intellectual disabilities.”
For patients with I&DDs, it is crucial to introduce the patient to the dental environment and provide patient-appropriate care in a slow and gentle manner that builds trust and cooperation. Caries risk must be part of the initial assessment, and it is important that both the parent/caregiver and patient be introduced to a viable home care regimen that is tailored to the patient’s abilities and not focused on the disabilities.
What are intellectual and developmental disorders?
I&DDs are classified as a complex group of neurobiological disorders that are caused by unusual brain development and that usually last throughout a lifetime. I&DDs include autism spectrum disorders (ASDs), which are associated with rigid routines and repetitive behaviors. Those afflicted have unusual ways of learning, paying attention, and reacting to different sensations.
Autism was first described in 1943 by American psychiatrist Leo Kanner of Johns Hopkins University. At the same time in Germany, Dr. Hans Asperger described a milder form of ASD, which eventually became known as Asperger’s syndrome. These disorders, along with several others, including but not limited to Rett syndrome, pervasive developmental disorder, and childhood disintegrative disorder, are seen in children with varying degrees of communication disorders or delays. For children experiencing developmental delays, skills develop at a slower rate than normal (based on age appropriateness, whether it be a communication or motor skill). The skills of a delayed child are present but are slow to emerge. Meanwhile, a child who presents with a disorder, such as an ASD, either has skills that develop abnormally (eg, the child once possessed a skill and then regressed, losing the skill) or does not develop skills at all at age-appropriate intervals. These developmental delays result in such symptoms as speech difficulties, lack of eye contact, isolation, and no fear of danger. I&DDs, including autism, can inhibit a person’s ability to communicate and develop social relationships and are often accompanied by extreme behavioral challenges.
Intellectual and developmental disorders and the dental professional
Dental professionals must be knowledgeable and comfortable treating patients who have these disorders. In the past, many dental professionals were not exposed in an educational setting to the challenges and rewards associated with treating this patient population. Based on the prevalence of these types of disorders, including ASDs, a dental professional will likely meet at least seven or eight patients this year who have been diagnosed with some form of an I&DD.
To provide the most appropriate treatment for each patient and to be successful in providing that care, the dental professional must take time to learn about each patient’s abilities prior to the initial dental visit. Dental professionals must request written information, which can be acquired in the form of a questionnaire prior to the visit. Furthermore, professionals must provide time during the initial visit to get to know the patient through interview and behavior assessment. These assessments should include inquiries about each patient’s situation at home and that patient’ specific abilities. Knowledge of the patient’s home environment and specific capabilities gives the dental professional a basis for tailoring dental care to the patient’s needs and capacities.
Intellectual and developmental disorders and the dental professional
Dental professionals must be knowledgeable and comfortable treating patients who have these disorders. In the past, many dental professionals were not exposed in an educational setting to the challenges and rewards associated with treating this patient population. Based on the prevalence of these types of disorders, including ASDs, a dental professional will likely meet at least seven or eight patients this year who have been diagnosed with some form of an I&DD.
To provide the most appropriate treatment for each patient and to be successful in providing that care, the dental professional must take time to learn about each patient’s abilities prior to the initial dental visit. Dental professionals must request written information, which can be acquired in the form of a questionnaire prior to the visit. Furthermore, professionals must provide time during the initial visit to get to know the patient through interview and behavior assessment. These assessments should include inquiries about each patient’s situation at home and that patient’ specific abilities. Knowledge of the patient’s home environment and specific capabilities gives the dental professional a basis for tailoring dental care to the patient’s needs and capacities.
Prevalence of intellectual and developmental disorders
Because autism is the most common form of I&DD, the following statistics are specific to ASDs to help put into perspective the significant size of this patient population. ASDs usually develop between ages 2 and 3, although recent research is beginning to look at diagnosis as early as 6 months of age. Autism is seen across all racial, ethnic, and social groups, with a male predominance of four to one. Symptoms can be very mild to very severe. Today 1 in 150 individuals is diagnosed with autism, making it more common than pediatric cancer, diabetes, and AIDS combined. It is seen in greater numbers than cerebral palsy, Down syndrome, and hearing and vision impairment ( Table 1 ). Three children per hour are diagnosed with ASDs, and the rate of diagnosis has increased 10-fold in the last decade, with 24,000 children currently diagnosed every year. Three million United States citizens have autism and the annual cost in the United States for caring for these individuals is estimated at $35 billion.
| Condition | Prevalence |
|---|---|
| Autism | 1 in 150 individuals |
| Cerebral palsy | 1 in 357 individuals |
| Juvenile diabetes | 1 in 450 individuals |
| Down syndrome | 1 in 800 individuals |
| Deafness/hearing loss | 1 in 909 individuals |
| Blindness/vision impairment | 1 in 1111 individuals |
Autism-specific etiologies
The etiology of autism is multifaceted, and no one particular factor has been proven to be “the” cause. The Centers for Disease Control and Prevention has called autism a national public health crisis whose cause and cure remain unknown. In May 2008, the International Meeting for Autism Research held its seventh annual meeting, with more than 850 presentations on various subjects related to autism, including etiology, biology, diagnosis, and treatment. Several of the presentations focused on the role of the environment as a risk factor for autism. Some discussion centered on the possibility that environmental factors may affect genetic risk factors.
Additionally, research is beginning to show that there is a familial pattern to symptoms of autism: If one child presents with symptoms, the parents are encouraged to be diligent in watching for signs/symptoms in other siblings, especially males. Other mechanisms being researched include nerve synapse connectivity and neuropathology of various structures of the brain. Preliminary research also indicates that a high percentage of patients with autism exhibit autoimmune disorders, such as food allergies or rhinitis. It has been demonstrated that maternal infections can result in the elevation of cytokines in the fetal environment, which in turn may be a risk factor for developmental disorders. Other hypotheses on the etiology of autism have been circulating for years, with no real definitive answers having been found. Some have speculated that autism might be a psychiatric disorder and have implicated the roles of amino acids, stress, prenatal aspartame exposure, vitamin A deficiencies, air pollution, and vaccinations. But the bottom line is that there is no answer yet and further research is needed in all areas of autism.
Signs and symptoms of autism
Autism is diagnosed according to a pattern of symptoms rather than one single symptom. The main characteristics involve difficulties with social interaction and communication, limited interests, and repetitive behavior. Early signs and symptoms of ASDs include:
- •
No big smiles or other warm, joyful expressions by 6 months of age or thereafter
- •
No back-and-forth sharing of sounds, smiles, or other facial expressions by 9 months of age (communication skills)
- •
No babbling by 12 months of age
- •
No back-and-forth gestures, such as pointing, showing, reaching, or waving by 12 months of age (motor skills)
- •
No words by 16 months of age
- •
No two-word meaningful phrases, without modeling or repeating, by 24 months of age
- •
Any loss of speech or babbling or social skills at any age
- •
Underdeveloped play skills for a particular age
- •
Oversensitivity to textures
As there is no medical test or biomarker for autism, diagnosis is based on observation of the child’s behavior, educational and psychological testing, and parent reporting. Several diagnostic tools are used in assessing for ASDs. The Autism Diagnostic Interview–Revised (ADI-R) and the Autism Diagnostic Observation Schedule (ADOS) are two of the most widely used. ADI-R can be used for both children and adults with a mental age of 18 months or above and contains 93 items. It focuses on behavior in three main areas: reciprocal social interaction, communication and language, and restrictive/repetitive stereotyped interests and behaviors. The ADOS is a semistructured assessment of communication, social interaction, and play or imaginative use of materials for individuals suspected of having autism or other ASDs. It enables the examiner to observe over a 30- to 45-minute period the occurrence or nonoccurrence of behaviors that have been linked to ASDs, and is appropriate for all age levels and developmental abilities. A team of specialists is usually involved in the diagnosis and evaluation. The team may include a neurologist, a psychiatrist, a developmental pediatrician, a psychologist, a gastroenterologist, an audiologist, a speech therapist, and an occupational therapist, as well as other professionals.
Preparation for treatment of patients with intellectual and developmental disorders
To treat patients with I&DDs, one needs an open mind and heart. Emotional skills may be more useful than intellectual and clinical skills. The ability to get close to the patient both physically and emotionally, and the ability to be guided by instinct and creativity, rather than by strict reasoning, are important. This is a very different and sometimes challenging way of practicing dentistry and dental hygiene, but it is often a rewarding experience. Much understanding of the patient’s condition can be obtained from the patient or parent/caregiver through documentation and interviews; however, because each patient is unique, most of the details are learned from one-on-one experience with the patient.
Documentation of the specific characteristics and abilities of the patient prior to the initial appointment is important for both the parent/caregiver and the dental professional. This provides an opportunity for the parent/caregiver to share with the dental professional all aspects of the patient’s life and abilities. Ultimately the family will recognize that the professional cares and understands that these disorders present differently in all cases. For the dental professional, a patient information form with questions about crucial aspects of the patient’s abilities is necessary to determine the proper skills and techniques required to provide successful dental treatment. This form should include sections for personal and medical information, dental experiences, oral habits, physical function, sensations, communication, vision, hearing, and behavior/emotions. A basic medical history form should be completed in its entirety and the additional information provided in this patient information form should be considered supplemental.
Personal and Medical Information
This first section of the form should include basic contact information as well as emergency names and phone numbers. A section should be included to provide the names and contact information of the general physician, as well as those of any developmental specialist or other specialists who routinely care for the individual. The nature and diagnosis of the condition needs to be addressed and a list of all medications should be provided. Allergies and sensitivities can be common in patients with I&DDs and should be discussed. In addition, the dental professional needs to be aware of any bowel or bladder adaptations necessary prior to performing dental treatment.
Dental Experiences
Information requested in the section on dental experiences should include those that have occurred in previous dental settings, as well as those that occur on a daily basis in the home. A discussion is necessary to explore the history of these experiences, as well as details about the daily at-home dental care routine, including products being used. Families/caregivers should be asked to provide information about the tolerance level of dental treatment both in-office and at-home daily. Finally, this section must include a statement of dental goals and expectations, both short term as it relates to the upcoming dental visit, as well as long-term expected care and realized benefits.
Oral Habits
Individuals with I&DDs can have any number of oral habits that should be discovered prior to the first dental appointment. Many of these individuals snack routinely through the course of the day as part of their need to satisfy oral sensory issues. In addition, because of food sensitivities or aversions, individuals may tend to always choose foods of a specific texture. Some patients may routinely choose a soft diet, while others may require hard crunchy foods to satisfy their sensory needs.
It is also important to ask about the type and frequency of nonnutritive behaviors. For some, sensory chewing involves chewing on rubber tubing or other materials as a stress release or to increase the muscular and sensing abilities of the masticatory muscles. Nonnutritive behaviors range from thumb/finger/pacifier sucking to pica, the ingestion of nonedible materials, including dirt, clay, paint, plaster, chalk, cigarette butts/ashes, glue, paper, buttons, toothpaste, or soap. While parents may think toothpaste is the lesser of the evils in this list, they should be instructed about the danger of toothpaste ingestion and provided with clear instructions on the proper amount of toothpaste to be used during brushing.
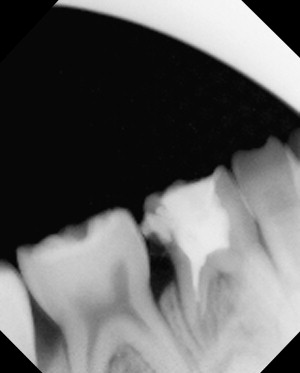
For teaching purposes, many therapists may choose caries-prone foods as a consistent reward for appropriate behaviors. Also, speech therapists may tend to choose foods that are sour or tart to help stimulate the mouth to entice language. Some of these choices, such as sour tarts, carbonated products, or lemons, can be erosive in nature and parents/caregivers need to provide therapists with more appropriate options ( Fig. 1 ).