37. What are the histologic characteristics of the initial lesion (stage I gingivitis)?
Basically the vasculitis of the blood vessels is accompanied by an increase of gingival exudate from the sulcus. PMNs (polymorphonuclear leukocytes) migrate into the sulcus and junctional epithelium. The most coronal portion of the junctional epithelium is altered, and some perivascular collagen is lost.
38. What are the histologic characteristics of the early lesion (stage II gingivitis)?
Many of the changes are a continuation of the initial lesion. PMNs continue to migrate into the epithelium, and other lymphocytes follow. The collagen network continues to break down, and the junctional epithelial cells proliferate. Ulceration of the gingival sulcus is also noted.
39. What are the histologic characteristics of the established lesion (stage III gingivitis)?
A key component of the established lesion is the predominance of plasma cells in the connective tissue, with the production of antibodies, continued loss of connective tissue substance, and proliferation of junctional epithelium, with or without apical migration.
40. What are the histologic characteristics of the advanced lesion (stage IV gingivitis)?
Many of the features are similar to those of the established lesion. The advanced lesion extends to the periodontal ligament and alveolar bone with pocket formation and goes through periods of exacerbation and remission. There are more extensive cellular changes because of inflammation.
41. A patient presents with heavy plaque and calculus without attachment loss. What is the periodontal diagnosis?
It is dental plaque-induced gingival disease (Fig. 6-2).
42. What are the clinical signs of necrotizing ulcerative gingivitis (NUG)?
NUG is an acute recurring infection of the gingiva characterized by necrosis of the papilla (leading to blunting), spontaneous bleeding, pain, and fetor oris.
43. Which bacteria are associated with NUG?
The bacteria associated with NUG are a fusospirochetal complex—fusiform bacteria and spirochetes.
44. How is necrotizing ulcerative periodontitis (NUP) different NUG?
There is loss of clinical attachment and alveolar bone in NUP.
45. Which bacteria are associated with gingivitis of pregnancy? Why?
Bacteria associated with gingivitis of pregnancy are the black-pigmenting Bacteroides spp., which use steroid hormones for their own metabolism. Therefore, pregnancy essentially selects for these bacteria. Patients who use birth control pills or receive steroid therapy (for chronic autoimmune disease) are also at risk.

46. A pregnant patient presents with gingival swelling on the palatal of the #12/13 area. She presents with minimal plaque buildup, without radiographic evidence of bone loss. What is the ideal initial periodontal treatment (Fig. 6-3)?
The patient is diagnosed with pregnancy-associated gingivitis. The treatment will review plaque control technique and initiation of scaling. Following the initial treatment, gingival swelling has been reduced (Fig. 6-4).
47. What is the American Dental Association’s periodontal diseases classification?
| Type I | Gingivitis |
| Type II | Mild periodontitis |
| Type III | Moderate periodontitis |
| Type IV | Severe or advanced periodontitis |
These categories are based on clinical and radiographic criteria, such as the amount of bone loss, pocket depth, and mobility.
48. How is chronic periodontitis further subclassified and characterized?

• Slight: 1 to 2 mm of clinical attachment loss
• Moderate: 3 to 4 mm of clinical attachment loss
• Severe: ≥5 mm of clinical attachment loss
49. What are the clinical features of localized aggressive periodontitis (LAP)?
• Clinical signs of inflammation and amount of local factors less than what would be expected for the severity of destruction
• Circumpubertal onset of disease
• Localized first molar or incisor disease with proximal attachment loss on at least two permanent teeth, one of which is a first molar
• Robust serum antibody response to infecting agents
50. Initial radiograph shows no bone loss on #13. However, radiographs are taken 3 and 6 years later showed extensive progressive bone loss. What is the most appropriate diagnosis for this patient?
It would be localized aggressive periodontitis (Fig. 6-5).
51. What are the clinical features of generalized aggressive periodontitis (GAP)?
• Usually affecting persons younger than 30 (but may be older)
• Generalized proximal attachment loss affecting at least three teeth other than first molars and incisors
• Pronounced episodic nature of periodontal destruction
• Poor serum antibody response to infecting agents
52. This patient presented with significant bone and clinical attachment loss, but minimal local factors. What is the most likely classification of this patient’s periodontal disease?
It would be generalized aggressive periodontitis (Fig. 6-6).
53. What bacteria is commonly associated with aggressive periodontitis?


54. What is the first cellular line of defense of the body against the periodontal pathogens?
Other than the epithelial cell barrier, the first line of defense is the PMN.
55. What is meant by a “burnout lesion” in a patient with LAP?
At one point, the patient with LAP had an infection with periodontal lesions in which the chief infectious agent was A. actinomycetemcomitans. The body responds with an immunologic response and controls the infection, but the bony defect remains. The deep pocketing now becomes inhabited with bacterial flora, which is more characteristic of chronic periodontal lesions.
56. Patients with deep periodontal pockets and heavy deposits of plaque and calculus may develop an acute periodontal abscess after scaling. Why?
This is the result of incomplete removal of causative agents.
57. What is a perio-endo (periodontal-endodontic) abscess?
A perio-endo abscess is a combined lesion in which periodontal and endodontic problems occur simultaneously. The lesion can be initiated by extensive periodontitis or by pulpal pathology.
58. What treatment is frequently used for a periodontal abscess?
Initial treatment may consist of the establishment of drainage and removal of the causative agents (incision and drainage through the sulcus, along with scaling, root planing, and irrigation), followed first by a course of antibiotic therapy and then by surgical treatment, when needed.
59. When is it safe to treat a pregnant woman’s nonacute periodontal problem?
In general, the second trimester is the window of treatment for most dental procedures. If antibiotics or other medications are indicated, consult with the obstetrician.
60. Which periodontal disease almost fulfills Koch’s postulates?
Koch’s postulates state that a pathogenic bacterium causes a disease, the disease is transmissible through the bacteria, and if you eliminate or control the bacteria, you eliminate the infection. A. actinomycetemcomitans (localized aggressive periodontitis) and P. gingivalis almost fulfill Koch’s postulates.
61. Which bacterial group is associated with root caries?
Root caries may be a problem for patients with gingival recession and xerostomia (whether induced by drugs, radiation, or some other agent). The bacteria associated with root caries are gram-positive rods and filaments, particularly Actinomyces viscosus.
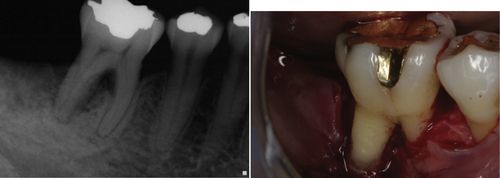
62. This patient presented with deep pocket depth and severe bone loss on #30. What is the most noticeable contributing factor that can be seen from the surgical exposure of the site?
It is enamel projection (Fig. 6-7).
Concept of Disease Activity
63. What is meant by active periodontitis?
It refers to periodontal inflammation causing an apical migration of epithelial attachment.
64. How is progressive periodontal disease activity measured?
Typically, disease activity (attachment loss) is measured by using a periodontal probe and fixed reference point, such as the cementoenamel junction (CEJ). The change in the probing depth, excluding any changes in the gingival height caused by inflammation, determines disease activity.
65. What is the classic definition of the presence of periodontal disease?
It is attachment loss with the presence of plaque-induced gingival inflammation and radiographic evidence of bone loss.
66. How is the radiographic evidence of bone loss determined?
In a healthy state, the crestal bone levels are about 2 mm below the CEJ. In periodontitis, crestal bone is below this level.
67. Which radiographs tend to be most accurate in the determination of bone loss?
Vertical bitewings.
68. What is the most common pattern of bone loss in periodontal disease?
Horizontal bone loss.
69. What is bone sounding?
Sounding is used to provide the clinician with additional information regarding the morphology of a bony defect. The area in question is anesthetized, and a probe is forced through the epithelium and connective tissue in the sulcus/pocket until it strikes the crestal bone. Sounding may facilitate flap design.
70. How is periodontal disease activity described?
Patterns of periodontal disease activity include random burst and slow continuous processes.
71. What is the difference between a nonspecific and specific plaque hypothesis?
The nonspecific hypothesis simply states that it is the quantity—not the quality—of the plaque that causes periodontal disease. The specific plaque hypothesis states that specific organisms in the plaque cause periodontal disease.
72. What traditional clinical marker (other than a great change in attachment loss) may be significant in determining active periodontal disease?
It is bleeding on probing—the more bleeding, the higher the likelihood of periodontal breakdown.
73. Which two inflammatory mediators may be indicators of disease activity?
Interleukin-l (IL-1) beta and tumor necrosis factor alpha may indicate disease activity.
74. What are the major risk factors for periodontal disease?
• Plaque
• Smoking
• Diabetes
• Incompetent immune system
• Genetics
75. What is the effect that open interproximal contacts can have on the periodontium?
Open interproximal can lead to food impaction, caused by plunger cusp activity, which can lead to inflammation and increased alveolar bone loss.
Periodontal Diagnosis
76. How is a periodontal pocket defined?
77. What is the difference between a suprabony and infrabony pocket?
• An infrabony pocket is where the tip of the probe is apical to the crest of the adjacent alveolar bone.
• A suprabony pocket is where the tip of the probe is at or coronal to the crest of the adjacent alveolar bone.
78. Which sites are routinely probed during a thorough periodontal examination?
Six sites are commonly checked—the mesio-, mid-, and distobuccal sites, as well as the corresponding lingual and palatal sites. Most periodontists sweep the probe continuously through the sulcus to get a better feel for the pocket depths as a whole.
79. What is a pseudopocket?
It is a pathologically deepened sulcus formed by gingival enlargement or incomplete passive eruption without attachment loss.
80. What is clinical attachment loss (CAL)?
The most coronal portion of the epithelial attachment is apical to the cementoenamel junction (CEJ). It is measured by adding the measurement of visible recession plus pocket/sulcus depth. If there is no visible recession it is the distance from the CEJ to the most coronal part of the epithelial attachment.
81. Which is more important in the progression of periodontal disease, attachment loss or periodontal pocketing?
Periodontal pocketing is more important because it is a pathologically deepened sulcus that cannot be maintained by the patient and can lead to additional attachment loss.
82. Which is more important in defining periodontal disease, attachment loss or periodontal pocketing?
Attachment loss is more important because the depth of a pocket does not necessarily indicate that there is bone loss.
83. What are the two most significant clinical parameters for the prognosis of a periodontally involved tooth?
The two most significant clinical parameters are mobility and attachment loss.
84. What is gingival hypertrophy?
Gingival hypertrophy indicates that there is an increase in size, generally because of edema.
85. What causes gingival recession?
• Toothbrush or floss abrasion
• Periodontal disease
• Trauma
• Prominent roots with a thin biotype
• Absence of a minimal zone of attached gingiva
86. Which area of the oral cavity has the least amount of attached gingiva?
The buccal mandibular premolar area commonly has the least amount of attached tissue.
87. What is a long junctional epithelium?
After a periodontal pocket has been scaled, root-planed, and curetted, a reattachment by epithelial cells to the root surface may occur. This reattachment is called a long junctional epithelium.
88. What is the term for gingival cells that attach to the root cementum? How do they attach to the root?
The term is junctional epithelium; the cells attach via mucopolysaccharides through hemidesmosomes.
89. What are mucogingival defects?
Mucogingival defects are defined by periodontal pocketing that extends to or beyond the mucogingival junction. It is an absence of attached gingiva.
90. Is periodontal disease a risk factor for other diseases?
Some epidemiologic evidence indicates that periodontal disease ia s risk factor for some other chronic systemic diseases (e.g. diabetes, cerebrocardiovascular (CVA) disease, adverse pregnancy outcome).
91. What is the crown-to-root ratio in a healthy dentition?
As a general rule, the crown-to-root ratio in a healthy dentition is 1:2 (for each tooth). Teeth with poor crown-to-root ratios tend to have a poor prognosis, especially if mobility is significant.
92. What root shapes generally have a more favorable prognosis?
The crown-to-root ratio is very important. Long tapering roots are usually sturdier than short conical roots. Long root trunks in multirooted teeth are more favorable than short root trunks.
93. What is the difference between bony fenestration and bony dehiscence?
Fenestration refers to a window in the bone, exposing the root. A dehiscence is where denuded areas of teeth extend through the marginal bone. Both are commonly noted in thin periodontium.
94. What is positive bony architecture?
Positive bony architecture is when the interproximal marginal bone is coronal to the cervical bone.
95. What is negative bony architecture?
Negative bony architecture is when the interproximal marginal bone is apical to the cervical bone.
96. What is flat bony architecture?
It is when both the cervical and the interproximal alveolar bone is at the same level.
97. What is an ideal bony architecture?
It is occurs when positive bony architecture is at the same level throughout the arch.
98. What are the basic classifications of bony defects?
Bony defects are generally classified according to the number of bony walls that remain. For example, a one-wall defect has only one remaining wall of bone and two-wall defects have two remaining walls.
99. Which bony defect is most likely to repair or fill naturally after treatment?
Narrow three-wall periodontal defects are most likely to repair naturally after therapy because there is less denuded surface of tooth to regenerate.
100. Name different microbiologic methods of assessing bacterial plaque.
There are numerous ways to assess bacterial plaque. General categories include culturing, microscopic, enzymatic, and genetic methods.
101. How are furcations classified?
Furcations are classified according to probing. Class I furcations are incipient furcations, class II, approximately are halfway into the furcation, and class III are completely through a furcation, from the facial to the lingual.
102. Why do diabetes, Papillon-LeFevre, and Chediak-Higashi diseases affect periodontium?
With all these diseases, the normal cellular immunologic response is impaired. The white cells (PMNs) do not function properly. Therefore, patients are susceptible to periodontal infections.
103. What is gingival crevicular fluid (GCF)?
GCF is an ultrafiltrate of serum. Therefore, it contains many of the components of serum, particularly complement and antibody. The flow rates of GCF have been studied in an attempt to predict disease activity. Furthermore, investigators have been interested in GCF for other markers of periodontal breakdown (e.g., beta-glucuronidase, interleukin, and collagenase).
104. Do links to specific genetic alleles predict a risk for periodontitis?
Yes, a variation in the IL-1 beta allele may indicate a risk for periodontitis. This variation has been shown to be especially important in smokers.
105. Do current smokers have the same levels of periodontitis as nonsmokers?
Generally, smokers have more attachment loss than nonsmokers.
106. What is the healing response of current smokers?
Typically, the response to nonsurgical and surgical therapy is poorer in smokers than non-smokers.
107. What happens to the risk of periodontitis and healing response if a patient stops smoking?
When a patient becomes a former smoker, the risk for periodontitis decreases and the healing response improves.
Adjunctive Periodontal Therapy
108. What antibiotics are used frequently to treat an acute periodontal abscess?
After the establishment of drainage, penicillin V (500 mg every 6 hours for 7 days) provides adequate antibiotic coverage.
109. What local delivery antibiotics may be advised for the treatment of chronic periodontitis?
They are minocycline and doxycycline.
110. What is the protocol for systemically treating aggressive periodontitis using antibiotics?
Localized aggressive periodontitis has a preponderance of A. actinomycetemcomitans and is treated with a combination of amoxicillin and metronidazole.
111. In a patient who is allergic to penicillin and erythromycin, what is the next antibiotic to be used for prophylaxis?
It is clindamycin, 600 mg, 1 hour before treatment.
112. Why are third-generation cephalosporins frequently contraindicated for the treatment of a periodontal abscess?
Frequently, the spectrum of a third-generation cephalosporin becomes so specific that it does not provide adequate antimicrobial coverage. Penicillin should be the first choice; erythromycin or clindamycin may be used in penicillin-allergic patients.
113. What complication may occur with the use of broad-spectrum antibiotics?
A major problem is the development of pseudomembranous colitis, caused by the overgrowth and toxin production of Clostridium difficile.
114. What are the major advantages and disadvantages of using local delivery doxycycline or minocycline for the treatment of periodontal disease?
The spectrum of doxycycline and minocycline may be slightly better than mechanical debridement alone, particularly in covering P. gingivalis. Other advantages include less photosensitivity, less chelating, and better patient compliance when compared with systemic antibiotics. Because both antibiotics are fat-soluble, the dose is reduced to 50 or 100 mg twice daily.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



