Introduction
Good periodontal status is essential for a successful treatment outcome of impacted maxillary canines. Whereas the surgical technique used for tooth uncovering has been shown not to affect the final periodontal status of palatally impacted canines, its effect on labially impacted canines is still unclear.
Methods
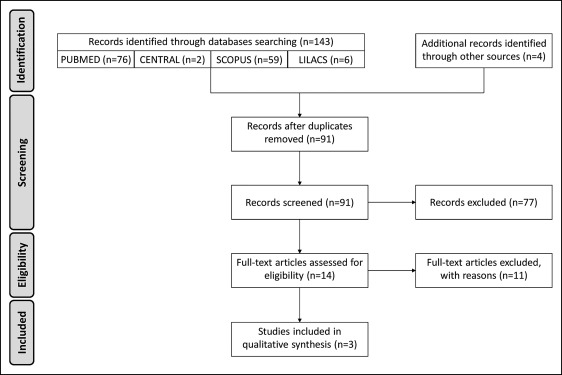
Searches of electronic databases through January 2015 and reference lists of relevant publications were used to identify studies evaluating the periodontal status of labially impacted canines after combined surgical-orthodontic treatment. Two reviewers independently screened the articles, extracted data, and ascertained the quality of the studies.
Results
Ninety-one studies were identified; 3 were included in the review. No included study examined the periodontal outcome of the closed eruption technique. Excisional uncovering was reported to have a detrimental effect on the periodontium (bleeding of the gingival margin, 29% vs 7% in the control group; gingival recession, −0.5 mm [SD, 1.0] vs −1.5 mm [SD, 0.8] in the control group; and width of keratinized gingiva, 2.6 mm [SD, 1.4] vs 4.1 mm [SD, 1.5] in the control group). Impacted canines uncovered with an apically positioned flap had periodontal outcomes comparable with those of untreated teeth.
Conclusions
The current literature is insufficient to determine which surgical procedure is better for periodontal health for uncovering labially impacted canines.
Highlights
- •
Periodontal status following treatment of labially impacted canines was reviewed.
- •
Excisional uncovering seems to result in a detrimental effect on the periodontium.
- •
An apically positioned flap seems to lead to periodontal outcomes similar to untreated teeth.
- •
Closed eruption’s periodontal outcome has not been properly evaluated yet.
- •
No surgical technique can be supported over others in terms of periodontal health.
Maxillary canine impaction is a clinical condition commonly encountered in dentistry. Approximately 2% of the general population and 4% of the subjects referred to orthodontists are affected, with a third of the impacted maxillary canines located labially.
Arch length deficiency has been reported to play an important role in the etiology of labial impactions: Jacoby found that only 17% of labially impacted canines had sufficient space to erupt. Orthodontic mechanics to open the space for the canine crown might lead to spontaneous eruption, but when space has been created and the canine does not erupt within a reasonable time, surgical uncovering of the impacted tooth should be considered. Three techniques are generally used to uncover labially impacted canines: excisional uncovering (gingivectomy), apically positioned flap, and closed eruption.
One fundamental indicator of a successful outcome in the treatment of impacted canines is the final periodontal status. A recent randomized clinical trial by Parkin et al showed that exposure and alignment of palatally impacted maxillary canines has a small periodontal impact that is unlikely to be clinically relevant, without significant differences in periodontal health between the open and closed techniques. Labial impactions seem to be more challenging to manage without adverse periodontal problems, and the surgical technique used to uncover the canine is thought to be critical for the final periodontal health because it affects the amount of attached gingiva over the tooth crown after eruption. However, the actual periodontal impact of the surgical technique used to uncover labially impacted canines is still unclear; to date, no systematic review has been undertaken on this topic.
The purpose of this study was to systematically review the literature on the periodontal status of labially impacted canines after combined surgical-orthodontic treatment with different surgical approaches to clarify whether there is sufficient evidence to support one surgical technique over the others in terms of periodontal health.
Material and methods
Eligibility was assessed on the basis of the following inclusion criteria.
- •
The population was patients receiving surgical treatment to correct labially impacted maxillary canines. No restriction for age, malocclusion, or type of orthodontic treatment was applied. Studies including both labial and palatal impactions were excluded because of the anatomic differences in the keratinized tissues between the palatal and labial mucosae. Studies including both incisors and canines were excluded because of the differences in the etiology of their impactions.
- •
The intervention was combined surgical-orthodontic treatment of labially impacted canines. At least 1 of the following surgical techniques had to be used in the study: closed surgical technique, excisional uncovering (radical exposure), or apically positioned flap.
- •
For comparison, when 1 technique was considered, the untreated contralateral side had to be used as the control. When 2 surgical techniques were compared, no untreated control group was required.
- •
Outcomes; studies were considered for inclusion if at least 1 of the following parameters was evaluated.
- 1.
Plaque accumulation: plaque volume on the dental surfaces. The Plaque Index by Silness and Loe, scored with a 4-point scale (0-3), is widely used to assess plaque accumulation.
- 2.
Gingival inflammation: assessment of the inflammatory conditions of the gingiva can be based on visual inspection and bleeding of the gingival margin (Gingival Index) or on gingival bleeding tendency alone (Gingival Bleeding Index) or bleeding tendency.
- 3.
Recession: distance from the cementoenamel junction (CEJ) to the gingival margin, with the gingival margin apical to the CEJ being positive, and the gingival margin coronal to the CEJ being negative.
- 4.
Periodontal probing depth: distance from the gingival margin to the location of the tip of a periodontal probe inserted into the pocket.
- 5.
Clinical attachment level: distance from the CEJ to the location of the inserted probe tip.
- 6.
Width of the keratinized gingiva: distance between the most apical point of the gingival margin and the mucogingival junction.
- 7.
Width of the attached gingiva: distance between the mucogingival junction and the projection on the external surface of the bottom of the gingival sulcus. It is obtained by subtracting the periodontal probing depth from the width of the keratinized gingiva.
- 8.
Crestal bone loss: distance between the CEJ and the alveolar bone crest measured on intraoral radiographs.
- 1.
- •
Study designs: randomized controlled trials, controlled clinical trials, and observational studies (cohort and case-control studies) were considered for inclusion if they fulfilled the population, intervention, comparisons, and outcomes criteria detailed above.
Information sources, search strategy, and study selection
The following databases were searched from their inception to January 2015 for relevant studies: PubMed, Cochrane Central Register of Controlled Trials, LILACS, and Scopus. There were no language restrictions. To identify the relevant studies the following search strategy was used: Search ((impact* OR unerupt* OR ectopic*) AND (labial* OR buccal* OR vestibular*) AND ((maxilla* OR upper) AND (canine* OR cuspid*)) AND (surgery or surgical*)); filters: humans. Further studies were identified by hand searching the reference lists of all relevant articles.
The first step in the screening process was to “unduplicate” the references by importing them into the reference management software “Mendeley” ( http://www.mendeley.com/features/reference-manager/ ). Two authors (D.R.I., S.I-P.) independently screened titles and abstracts. For studies that appeared to be relevant, or when a definite decision could not be made based on the title or abstract alone, the full article was obtained and independently examined by the reviewers for detailed assessment against the inclusion criteria. Because of the dichotomous nature of the ratings (accept or reject), agreement between the assessors (interassessor reliability) was formally assessed using the kappa statistic. Disagreements were resolved by discussion. When resolution was not possible, a third reviewer (G.A-B.) was consulted.
Data items and collection
Data extraction included the following items: (1) first author, year of publication, and location; (2) study design; (3) population characteristics (subjects enrolled, mean age, and sex distribution); (4) intervention (surgical exposure, orthodontic traction); (5) investigated comparisons; (6) follow-up of the study; (7) outcome measures; (8) significance level of the statistical tests; and (9) outcomes.
Two authors (D.R.I., S.I-P.) independently performed the data extraction using a previously piloted form. Disagreements were resolved by discussion. When resolution was not possible, a third reviewer (G.A-B.) was consulted.
Quality assessment in the studies
Two authors (V.C., A.G.) were blinded to the authors and the sources of each reference and independently assessed the research design as well as a 3-category rating of the internal validity of each study (according to criteria that varied depending on the study design), as stated by the U.S. Preventive Services Task Force ( Table I ). Disagreements were resolved through consensus. The Spearman rank correlation coefficient was applied to evaluate the agreement between the raters.
| Definition of ratings | |
|---|---|
| Study design | |
| I | Properly randomized controlled trial |
| II-1 | Well-designed controlled trial without randomization |
| II-2 | Well-designed cohort or case-control analytic study, preferably from more than 1 center or research group |
| II-3 | Multiple time series with or without the intervention; dramatic results in uncontrolled experiments could also be regarded as this type of evidence |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies, and case reports, or reports of expert committees |
| Internal validity ∗ | |
| Good | The study meets all criteria for that study design † |
| Fair | The study does not meet all criteria for that study design but is judged to have no fatal flaw that invalidates its results † |
| Poor | The study contains a fatal flaw |
∗ Internal validity is the degree to which the study provides valid evidence for the population and setting in which it was conducted.
† criteria for grading internal validity (limited to the study designs of the studies included in the review) were reported in Table V .
Data synthesis
The findings of the studies included in the systematic review were gathered. A quantitative synthesis using formal statistical techniques such as meta-analysis seemed inappropriate because the selected studies were too few, with nonrandomized designs and a lack of homogeneity in the study settings. Therefore, a narrative synthesis was carried out.
Results
Study selection and characteristics
The Figure shows the flow of the literature search according to the PRISMA format. The comprehensive search yielded 91 potentially relevant studies. Screening excluded 77 publications based on titles and abstracts. The full-text analysis of the remaining 14 studies led to the exclusion of 11 more articles ( Table II ). Therefore, 3 studies fully met the eligibility criteria and were included in the review ( Tables III and IV ). Excellent agreement between reviewers was found both in the screening (titles and abstracts, κ = 0.917; full texts, κ = 1.000) and in the quality assessment ( Table V ; P = 1.000).
| Authors, year | Reason for exclusion |
|---|---|
| Caminiti et al, 1998 | Unsuitable sample (palatal and labial impactions) |
| Crescini et al, 1994 | Unsuitable sample (palatal and labial impactions) |
| Crescini et al, 2007 | Unsuitable sample (palatal and labial impactions) |
| Gaulis and Joho, 1978 | Unsuitable sample (palatal and labial impactions), inadequate methodology (no inferential statistics) |
| Odenrick and Modéer, 1978 | Unsuitable sample (incisors and canines, palatal and labial impactions), inadequate methodology (no inferential statistics) |
| O’Dowling, 2009 | Review outcomes of interest not reported in the study |
| Quirynen et al, 2000 | Unsuitable sample (palatal and labial impactions) |
| Soroka-Letkiewicz et al, 2005 | Unsuitable sample (incisors and canines), inadequate methodology (no inferential statistics) |
| Szarmach et al, 2006 | Unsuitable sample (palatal and labial impactions) |
| Vermette et al, 1995 | Unsuitable sample (incisors and canines) |
| Wisth et al, 1976 | Unsuitable sample (palatal and labial impactions) |
| Characteristics | Boyd, 1984 | Tegsjö et al, 1984 | Kim et al, 2007 |
|---|---|---|---|
| Participants | |||
| Inclusion criteria | Unilateral labially impacted maxillary canine | Unilateral labially impacted maxillary canine | Labially impacted maxillary canine |
| Surgical exposure and orthodontic alignment of the impacted canine | Surgical exposure of the impacted canine performed between 1977 and 1979 | Surgical exposure of the impacted canine through APF | |
| All appliances removed for a minimum of 6 months | Minimum recall period of 1 year after the surgery | ||
| Subjects, n (% male) | 24 (33%) | 50 (44%) | 20 (-) |
| Mean age (y) (SD, range) | – (-, 15/22) at time of the study | 12.9 (-, 10/18) at time of the surgery | – |
| Intervention | RE: entire crown exposed by the window approach | RE: surgical uncovering; surgical dressing for 1 week; orthodontic traction | Full fixed orthodontics; surgical uncovering (APF); surgical dressing for 1 week; orthodontic traction |
| PE: 2-3 mm of keratinized tissue maintained with either an APF or a tissue excision | APF: Surgical uncovering; surgical dressing for 1 week; orthodontic traction | ||
| Comparisons | RE vs CTR | RE vs CTR | APF vs CTR |
| PE vs CTR | APF vs CTR | ||
| RE vs PE | RE vs APF | ||
| Recall period (mo) | 6-24 after removal of fixed appliances | 30-56 after surgical exposure | Minimum of 12 after surgery |
| Outcomes | PI, GI, BT, REC, PPD, LA, WAG | GBI, WKT (lab), PPD, REC | PI, GI, PPD, WAG, clinical crown length, bone loss |
| Study design | Controlled clinical trial | Retrospective cohort study | Retrospective cohort study |
| Boyd, 1984 | Tegsjö et al, 1984 | Kim et al, 2007 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CTR | RE | PE | Significance only P <0.05 |
CTR | RE | APF | Significance only P <0.01 |
CTR ∗ | APF ∗ | Significance only P <0.05 |
|
| PI | 0.66 (SE, 0.143) | 0.75 (SE, 0.150) | NS | ||||||||
| GI | NR | NR | NR | RE > CTR RE > PE |
0.30 (SE, 0.108) | 0.43 (SE, 0.120) | NS | ||||
| BT | NR | NR | NR | RE > CTR RE > PE |
|||||||
| GBIb | 7% | 29% | 7% | RE > APF RE > CTR |
|||||||
| REC | NR | NR | NR | RE > CTR RE > PE |
−1.5 mm (SD, 0.8 mm) † −1.1 mm (SD, 0.9 mm) ‡ |
−0.5 mm (SD, 1.0 mm) | −0.9 mm (SD, 1.2 mm) | RE > CTR | |||
| PPD | |||||||||||
| Buccal | 1.6 mm (SD, 0.6 mm) † 1.6 mm (SD, 0.4 mm) ‡ |
1.2 mm (SD, 0.4 mm) | 1.4 mm (SD, 0.4 mm) | APF > RE CTR > RE |
1.76 mm (SE, 0.092 mm) | 1.86 mm (SE, 0.105 mm) | NS | ||||
| Mesial | 1.9 mm (SD, 0.6 mm) † 2.2 mm (SD, 0.7 mm) ‡ |
2.4 mm (SD, 0.6 mm) | 2.1 mm (SD, 0.5 mm) | NS | |||||||
| Palatal | 1.9 mm (SD, 0.5 mm) † 2.0 mm (SD, 0.5 mm) ‡ |
2.1 mm (SD, 0.5 mm) | 2.0 mm (SD, 0.5 mm) | NS | |||||||
| Distal | 2.0 mm (SD, 0.6 mm) † 2.1 mm (SD, 0.6 mm) ‡ |
2.6 (SD, 0.6 mm) | 2.2 mm (SD, 0.6 mm) | NS | |||||||
| LA | NR | NR | NR | RE > CTR RE > PE |
|||||||
| WKG | 4.1 mm (SD, 1.5 mm) † 3.9 mm (SD, 1.5 mm) ‡ |
2.6 (SD, 1.4 mm) | 4.3 mm (SD, 1.8 mm) | APF > RE CTR > RE |
|||||||
| WAG | NR | 0.0 mm | 3.67 mm (SD, 1.72 mm) |
NR | 3.73 mm (SE, 0.254 mm) | 4.16 mm (SE, 0.410 mm) | NS | ||||
| Clinical crown length | 9.01 mm (SE, 0.418 mm) | 9.14 mm (SE, 0.371 mm) | NS | ||||||||
| Bone loss | 1.08 mm (SE, 0.173 mm) | 1.36 mm (SE, 0.185 mm) | NS | ||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


