6 Patient History and Clinical Examination
Painless Enlargement and Palpable Masses
Facial Nerve Weakness or Palsy
Disturbance of Saliva Secretion (Dry Mouth, Drooling)
The Submandibular and Sublingual Gland
Acute Inflammation and Abscess
Chronic Sialadenitis and Sialadenosis
Introduction
Any diagnosis of diseases of the salivary glands begins with a careful history and examination of the glands and saliva. Much depends on the duration of the history and the clinical features of a lesion. These may make it clear whether or not a tumor is present, and if it is may suggest whether it is benign or malignant. The patient’s age and sex, in conjunction with demographic features of salivary gland lesions, should also be taken into account in the diagnostic process. Any history of systemic disease and of drugs being taken should also be carefully assessed. Ultrasound is the most attractive method for completing the patient history and examination, as most hospitals have access to suitable equipment and expertise in its use. It is relatively easy to obtain good diagnostic scans of the major salivary glands, as they are largely subcutaneous structures, and there is the additional advantage that the technique is noninvasive, dynamic, and can be carried out in real time.
Patient History
A careful history is particularly helpful in evaluating salivary gland diseases and will often suggest a presumptive diagnosis. The duration of the disease, the description of the symptoms, and the patient’s age in particular are rewarding. The salivary glands produce saliva to moisten the mouth. The parotid gland produces 25% of the saliva and drains into the mouth near the upper teeth. The submandibular gland produces 70% of the saliva and drains into the mouth from under the tongue. The sublingual gland produces 5% of the saliva and drains into the floor of the mouth. In addition, 600–1000 tiny glands (the minor salivary glands) are located in the lips, inner cheek, and in the lining of the mouth and throat.
 The most common cause of salivary gland symptoms is because the duct has become blocked and saliva is unable to drain.
The most common cause of salivary gland symptoms is because the duct has become blocked and saliva is unable to drain.
 Acute Uncomfortable Swelling
Acute Uncomfortable Swelling
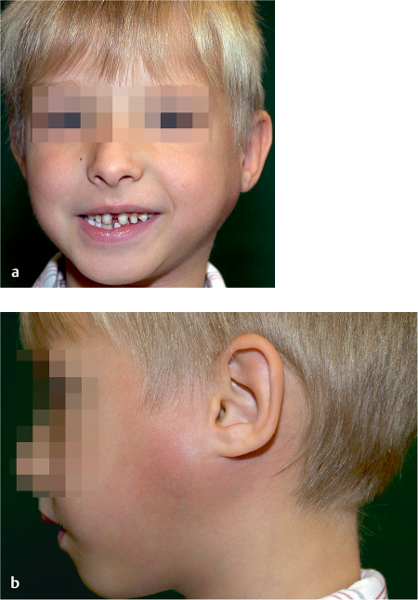
Obstruction to salivary flow most commonly occurs in the parotid and submandibular glands, usually due to stone formation. Symptoms typically occur during eating. Saliva production is initiated, but the saliva is unable to exit the ductal system, leading to swelling of the involved gland and significant pain, sometimes with an infection. If stones are not totally obstructive, the major glands will swell during eating and then gradually subside after eating, only to enlarge again at the next meal. Infection often develops in the abnormally pooled saliva, leading to more severe pain and swelling in the glands. If left untreated long enough, the glands may become abscessed. In some individuals, the ductal system of the major salivary glands may be abnormal. These ducts can develop small constrictions that reduce salivary flow, leading to recurrent infection and obstructive symptoms. Rarely, children have recurrent infections of the parotid gland, known as recurrent juvenile parotitis (Fig. 6.1). The most common salivary gland infection is mumps, which involves the parotid glands.
Fig. 6.1 a, b Recurrent juvenile parotitis: a typically a painful unilateral parotid swelling, usually with a fever, and b marked redness and swelling of the overlying parotid skin area.
 Mumps is most common cause of acute parotid swelling in children, but it may also affect adults. If an acute swelling occurs in an adult in a localized area of one parotid, it is more likely to be due to duct obstruction or a tumor.
Mumps is most common cause of acute parotid swelling in children, but it may also affect adults. If an acute swelling occurs in an adult in a localized area of one parotid, it is more likely to be due to duct obstruction or a tumor.
Summary
Differential diagnosis of painful swelling of salivary glands:
 Sialolithiasis
Sialolithiasis
 Viral sialadenitis
Viral sialadenitis
 Acute bacterial sialadenitis
Acute bacterial sialadenitis
 Malignant tumors
Malignant tumors
 Recurrent parotitis
Recurrent parotitis
 Chronic sialadenitis of the submandibular gland
Chronic sialadenitis of the submandibular gland
 Electrolyte sialadenitis
Electrolyte sialadenitis
 Drug-related salivary gland pain
Drug-related salivary gland pain
 Auriculotemporal neuralgia
Auriculotemporal neuralgia
 Sialadenitis of the minor salivary glands
Sialadenitis of the minor salivary glands
 Radiation sialadenitis
Radiation sialadenitis
 Painless Enlargement and Palpable Masses
Painless Enlargement and Palpable Masses
Primary benign and malignant salivary gland tumors usually present as painless enlargements of these glands. Tumors rarely involve more than one gland and are detected as a growth in the parotid, submandibular area, on the palate, floor of the mouth, cheeks, or lips. These enlargements should be checked carefully by an otolaryngologist and head and neck surgeon, since malignancy has to be excluded.
The only known risk factor is smoking, in relation to Warthin tumor. Salivary gland enlargement is also seen in autoimmune diseases, which cause significant inflammation. Patients than often have a dry mouth or dry eyes. This may also occur with other systemic diseases such as rheumatoid arthritis. Diabetes and other metabolic diseases may cause sialosis, an enlargement of both parotid glands. Salivary gland swelling (usually on both sides) is also seen in alcoholics and bulimic or anorectic patients. Painless masses on the palate or floor of the mouth are the most common presentation of minor salivary neoplasms.
 There are no specific tests or tumor markers currently available that are capable of identifying patients with a risk factor that may be associated with the early presence of a salivary gland malignancy. Benign and malignant tumors usually manifest clinically as a slowly growing, painless mass in the salivary gland.
There are no specific tests or tumor markers currently available that are capable of identifying patients with a risk factor that may be associated with the early presence of a salivary gland malignancy. Benign and malignant tumors usually manifest clinically as a slowly growing, painless mass in the salivary gland.
 Facial Nerve Weakness or Palsy
Facial Nerve Weakness or Palsy
Malignant tumors of a major salivary gland may grow rapidly or may show a sudden growth spurt. Pain may be present, and there can be a loss of movement of parts or all of the affected side of the face due to facial nerve involvement. The mass can be fixed to adjacent tissue, often with an ill-defined periphery or edge of the swelling. Eventually, the overlying skin or mucosa may become swollen, inflamed, or even ulcerated, or the adjacent tissues may be destroyed by tumor invasion. If such symptoms present or are described, they should suggest a serious diagnosis and prompt immediate investigation. It is important to emphasize that painful facial paralysis or another neurologic deficit associated with a salivary gland mass strongly suggests a possible malignant cause. However, most patients with salivary gland cancer present with a slowly enlarging, painless mass. A discrete mass in an otherwise normal-appearing gland is the usual finding for a parotid gland neoplasm.
|
|
Hypersialorrhea |
Sialopenia |
|
Physiologic states |
Acidic fruits |
Hot/dusty work environment |
|
|
Pregnancy |
|
|
|
Appetite stimulants |
|
|
|
Nausea and vomiting |
|
|
Diseases |
Stomatitis |
Febrile infections |
|
|
Diabetes insipidus |
Epithelioid cell sialadenitis (Sjögren disease) |
|
|
Parkinson disease |
Radiation sialadenitis |
|
|
Cerebral palsy |
Electrolyte sialadenitis |
|
|
Encephalitis |
Alcoholism |
|
|
Sluder neuralgia |
Vitamin A deficiency |
|
|
Erythroprosopalgia (Bing–Horton) |
Hyperthyroidism |
|
|
Myasthenia gravis |
Diabetes mellitus |
|
|
Wilson disease |
Pernicious anemia |
|
|
Rabies |
Iron-deficiency anemia |
|
|
Botulism |
Gastric achylia |
|
|
Pellagra |
Dehydration |
|
|
Down syndrome |
Uremia |
|
|
Psychoses |
Coma |
|
|
|
Cachexia and marasmus |
|
|
|
Depression |
|
Toxic agents |
Metal poisoning (e.g., mercury) |
Food poisoning (e.g., mushrooms) |
|
Pharmacological agents |
Psychotropic drugs (clozapine) |
Antihypertensives |
|
|
Acetylcholine |
Antidepressants |
|
|
Alkyl phosphatases (parathion) |
Analgetics |
|
|
Morphine |
Tranquilizers |
|
|
β–receptor-blocking drugs |
Diuretics |
|
|
Caffeine |
Chemotherapy |
|
|
Strychnine |
Antihistamines |
|
|
Theophylline |
|
The incidence of facial nerve involvement by parotid cancer on presentation has been reported to be below 20%. However, facial nerve palsy accompanied by pain serves as an important negative prognostic factor. Pain is a key prognostic factor and is associated with poor survival, based on the hypothesis that pain is predictive of tumor recurrence if it is associated with histologically visible perineural growth—suggesting that this characteristic may be the histologic substrate for pain.1
 Rapid growth, pain, or facial nerve palsy indicate a salivary gland cancer if a mass is present in one of the glands, and they serve as a negative prognostic factor. However, it is much more frequent for salivary gland cancer to present as an otherwise asymptomatic palpable lump in the gland affected.
Rapid growth, pain, or facial nerve palsy indicate a salivary gland cancer if a mass is present in one of the glands, and they serve as a negative prognostic factor. However, it is much more frequent for salivary gland cancer to present as an otherwise asymptomatic palpable lump in the gland affected.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses