Fig 7.1 Flowchart showing possible alterations in bone healing in diabetic patients.
Special considerations for implant therapy in diabetic patients
Healing and risk of postoperative infection: The repercussions of diabetes on the healing of soft tissue depend on the degree of glycaemic control in the perioperative period and the existence of chronic vascular complications. Patients with poor metabolic control have their immune defences impaired: granulocytes have altered functionality with modifications in their movement towards the infection site and deterioration in their microbicide activity, with greater predisposition to infection of the wound. In addition, the high concentration of blood-glucose in body fluids encourages the growth of mycotic pathogens such as candida. The microangiopathy arising as a complication of diabetes may compromise the vascularization of the flap, thus delaying healing, and also acting as a gateway for the infection of soft tissue.
Perioperative measures: In view of the studies revised, high levels of glucose in plasma have a negative influence on healing and bone remodelling processes. In order to ensure osseointegration of the implants (understood as the direct bond of the bone with the surface of the implant subjected to functional loading) and to avoid delays in the healing of gum tissue, it is necessary to maintain good glycaemic control before and after surgery. To measure the status of blood-glucose levels in the previous 6–8 weeks, the HbA1c values have to be known (< ?xml:namespace prefix = "mbp" />
Table 7.1 Showing the relation of glycosylated Hb% with diabetes
| GLYCOSYLATED HB% | DIABETIC SITUATION | IMPLANT SURGERY |
|---|---|---|
| <6% | Non-diabetic | Can be done |
| 6–7% | Excellent control | Can be done |
| 7–8% | Good control | Can be done with regular postoperative blood sugar monitoring |
| 8–10% | Average control | Should be avoided |
| >10% | Poor control | Contraindicated |
Table 7.2 Recommendations to reduce the risk of implant failure in diabetic patients
Conclusion
There is evidence that hyperglycaemia has a negative influence on bone formation and remodelling and reduces osseointegration of implants. Soft tissue is also affected by the microvascular complications deriving from hyperglycaemia – vascularization of the tissue is compromised, healing is delayed and wounds are more predisposed to infection. This entails an increase in the percentage of failures in implant treatment of diabetic patients. The bibliography reviewed recommends good glycaemic control in the perioperative period, in order to improve the survival rates for implants in diabetics. HbA1c figures of less than 7% indicate appropriate glycaemia levels in the preceding 6–8 weeks. Preoperative antibiotic therapy and the use of 0.12% chlorhexidine mouthwash are recommended, as both measures have been shown to reduce the percentage of failures. Although there is a higher risk of failure in diabetic patients, experimental studies have shown that the optimization of glycaemic control improves the degree of osseointegration in implants. Nonetheless, it is necessary to extend the number of prospective studies in humans, in order to clarify the true impact of diabetes on the prognosis for osseointegration.
Hypertension
Hypertensive patients often have the tendency to bleed more than the normal because of high vascular pressure; hence, they should be only operated under controlled blood pressure conditions. A continuous monitoring of the blood pressure is also mandatory during surgical procedures in implantology.
Thyroid disorders
Implant therapy can successfully be given to patients with hypothyroidism but hyperthyroidism is a medical problem which requires attention, as excessive production of the thyroxin hormone results in symptoms like increased pulse rate, nervousness, intolerance to heat, excessive sweating, atrial fibrillation, and congestive heart failure. Patients with hyperthyroidism are also sensitive to catecholamines such as epinephrine in local anaesthesia. When such patients are exposed to catecholamines, coupled with the stress often related to implant surgery, an exacerbation of the symptoms of hyperthyroidism may occur during surgery, resulting in thyrotoxicosis or “thyroid storm”, which is often life-threatening to the patient. The physician’s opinion and the normal range of thyroxin investigation, i.e. the patient who reports normal thyroid function and has had no symptoms of the disease during the preceding 6–8 months, is at low risk and can successfully get the implant surgery done. Patients with hyperthyroidism should receive the implant surgery in a very calm and comfortable operatory environment and if local anaesthesia is used, it should be devoid of adrenalin. Anti-anxiety/sedative drugs should also be avoided in such patients.
Bone disorders
Patients with bone disorders like osteoporosis, which is usually age-related, present with decrease in bone mass, increased micro-architectural deterioration, and susceptibility to bone fractures. This mostly occurs in the patients after the age of 60 but is very common even at an earlier age in postmenopausal women or women who have the history of ovariectomy, because the lack of oestrogen increases the chances of osteoporosis. A recommended dose of calcium, which can be range from 800 to 1500 mg/day and regular exercise is helpful to maintain the bone mass and increase bone strength. Such patients should thoroughly be investigated and treated before implant therapy.
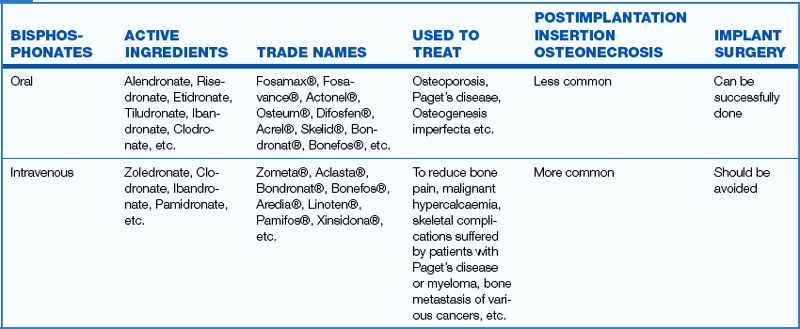
Patients on bisphosphonates
Bisphosphonates are a group of drugs used to treat pathologies, including Paget’s disease, osteoporosis, multiple myeloma and metastases associated with breast or prostate cancer. Bisphosphonates act on osteoclasts, inhibiting their chemotaxis and lifespan and hence, they inhibit bone resorption and induce osteonecrosis. There are important differences between bisphosphonates administered intravenously or taken orally. Oral administration of bisphosphonates to postmenopausal women to treat osteoporosis is fairly common. Hence, this group of patients should be investigated for bisphosphonate therapy. The American Association of Oral and Maxillofacial Surgeons does not contraindicate dental implant placement in patients who have been taking bisphosphonates orally for under 3 years prior to surgery, but the drug should be stopped for a minimum of 3 months before carrying out implant surgery and should be restarted only after at least 3 months following implant surgery (
Oral malignancy and osteoradionecrosis
Any benign or malignant oral lesion should be diagnosed and treated before implant insertion. Patients who are given postsurgical radiotherapy for oral malignant lesions often show degeneration of the osteovascular tissues (osteoradionecrosis); hence the regeneration capacity of the bone is hindered for a minimum of 6 months after radiotherapy is completed. Thus, the implant surgeon should wait for a minimum of 6 months after radiotherapy is completed, to place the implant. Six months after completion of radiotherapy treatment, new vascular tissue starts regenerating inside the bone, which is paramount for predictable quality implant osseointegration with the surrounding bone.
Liver cirrhosis
The major cause for liver cirrhosis is alcohol consumption. The liver synthesizes clotting factors and detoxifies drugs, hence patients with liver disease show reduced synthesis of the clotting factor (thrombocytopaenia) and prolonged bleeding time during implant surgery. The patients with normal liver function test (SMA, CBC, PTT, and PT) values are at low risk and can be treated as normal patients with basic implant procedures. The physician’s opinion is highly recommended for these patients before performing the implant surgical procedures.
Angina pectoris
It is a form of coronary heart disease, which causes chest pain or cramp of the cardiac muscles because of temporary myocardial ischaemia (low oxygen supply to the cardiac muscles). Atherosclerosis of the coronary vessels is the most common cause of angina pectoris. When treating such patients, the physician’s opinion should be taken before performing implant surgery and nitroglycerin (0.4 mg) tablets should be kept ready in the dental emergency kit. The dental procedure should be done in a stress-free environment and divided into multiple short duration procedures. If the patient complains of chest pain, the procedure should be stopped immediately and the nitroglycerin tablets should be administered sublingually. Local anaesthetics devoid of vasoconstrictors (adrenalin) like xylocard should be used in such patients. Anti-anxiety drugs and prophylactic administration of nitroglycerin tablets are also helpful to reduce the onset of angina in such patients during implant surgery.
Myocardial infarction
Myocardial infarction (MI) is a prolonged ischaemia (lack of oxygen supply) that causes injury to the heart. Such patients complain of severe chest pain in the left precordial area during the MI episode, which radiates to the left arm or mandible. The pain is similar to angina pectoris, but more severe and presents symptoms like cyanosis, cold sweat, weakness, nausea or vomiting, and irregular and increased pulse rate, etc. Being a life-threatening medical problem, the implant surgeon besides taking all the precautions as for angina, should take the opinion of a cardiologist before treating such patients. These patients should preferably be treated in hospital where all the emergency management facilities are available.
Subacute bacterial endocarditis (SABE)
It is an infection of the heart valves or the endothelial surfaces of the heart. The microorganisms mainly associated with endocarditis following dental treatment, are streptococci and staphylococci, and less frequently, anaerobes. The risk of bacterial endocarditis increases with the amount of intraoral soft tissue trauma. Improvement of oral hygiene with scaling and root planing, and the administration of prophylactic antibiotics before performing any implant surgical procedure, reduce the onset of subacute bacterial endocarditis after dental surgery, to a large extent (
Pregnancy
Being an elective procedure, implant surgery should be avoided during pregnancy as the radiographs and medications for the implant procedures may adversely affect the growth of the fetus. Moreover, periodontal diseases are often exacerbated during pregnancy.
Smoking
The lower success rate of endosteal implants in smokers is well documented in literature.
Oral examination
Detailed oral examination of the patient is paramount for diagnosis and treatment planning for successful implant therapy. The following clinical findings should be examined in detail.
Arch form
The arch form influences the number and positions of the implants required in fixed implant prosthesis for the edentulous maxilla and mandible. Three types of dental arch forms are found in patients.
Square arch: shows minimum facial cantilevered forces; thus minimum number of implants are required to support a full-arch fixed or completely implant-supported removable prosthesis. Only two implants are required at the canine positions to restore the anterior maxillary or mandibular region. Placement of any implant anterior to the canine region is usually not required to restore the full-arch. The full-arch, fixed, implant-supported restoration (12–14 units) can be made possible by placing only six implants (two at canine, two at second premolar, and two at first molar positions) (
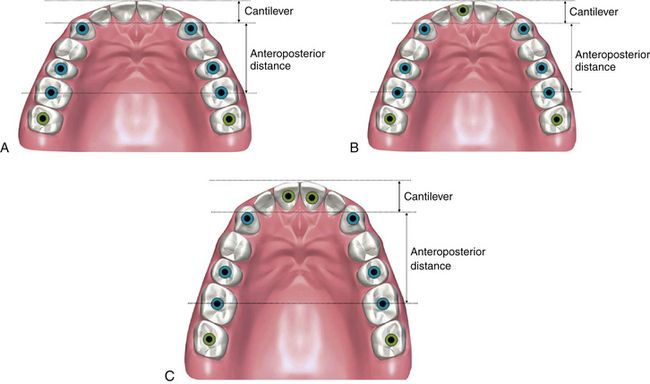
Fig 7.2 The arch form should be evaluated during treatment planning for multiple or full-arch implants. (A) The square arch form shows the least facial cantilever, hence requires least number of implants to restore the maxilla or mandible and no implant is usually required anterior to the canine positions. (B) The oval arch form has more facial cantilevering; hence at least one implant should be added anterior to the canine position to restore such arch. (C) The tapering arch form has the maximum facial cantilevering hence requires two additional implants anterior to the canine positions. If 14-unit fixed prosthesis is planned, two more implants should be added at the second molar positions.
Ovoid: shows more facial cantilevered forces on the prosthesis compared to the square arch form, thus one more implant should be added anterior to canines positions (at one of the central incisor positions) to reduce the cantilevered forces on the rest of the implants (
Tapering: has the maximum facial cantilevered forces, thus two more implants should be added anterior to canine positions (one at each central incisor position) to reduce the cantilevered forces on the rest of the implants (
Ridge morphology of edentulous region
Ridge morphology of the edentulous region gives an approximate idea about underlying bone dimensions, positions, and angulations required for implant placement, and also reveals the presence of any severe undercut in ridge morphology, etc.
Soft tissue biotype
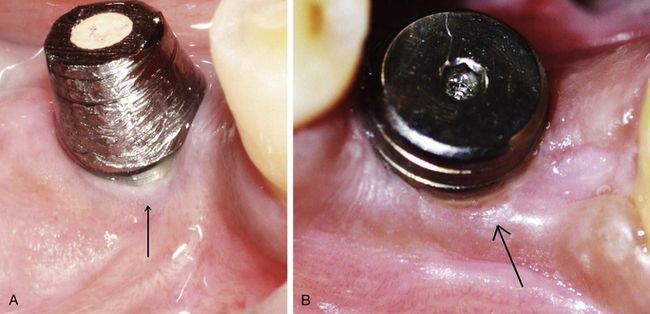
A thick biotype that contains a thick connective tissue layer under the keratinized attached epithelium is considered to be favourable for implants. The thick biotype makes a tight seal around the implant prosthesis and is more resistant to the recession and peri-implant infections (
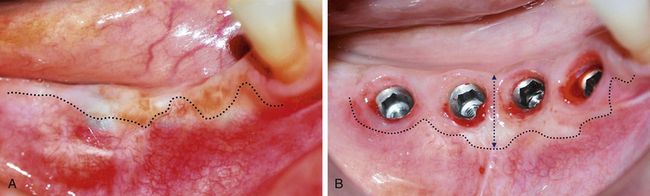
Width of keratinized soft tissue
A thick band of keratinized soft tissue is paramount around the future implant prosthesis to make it resistant to peri-implant infections. The clinician should evaluate and plan to achieve at least 3 mm of attached keratinized thick marginal soft tissue collar around the implant prosthesis. If a non-keratinized thin and mobile soft tissue is found at the implant site, he/she should plan for soft tissue grafting procedure at the time of implant uncovery, to generate new thick and keratinized soft tissue around the implant prosthesis (
Papilla at the implant site (intact or flattened)
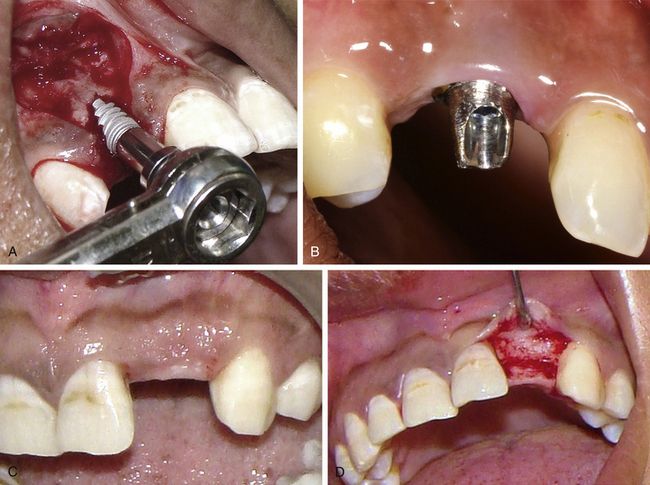
The careful evaluation of the presence or absence of papilla should be made during treatment planning for the implant in the aesthetic region. If the papillae are intact, the papilla preservation incision is preferred for the implant placement (
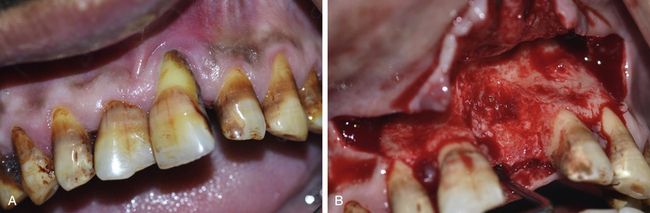
Periodontal health of adjacent teeth
The teeth adjacent to the edentulous region should be checked for any deep soft tissue pocket, or any periodontal defect with active purulent discharge. Often infection in the adjacent teeth can infect the inserted implant; therefore, all the periodontal problems of the adjacent teeth should thoroughly be diagnosed and treated before implant insertion (

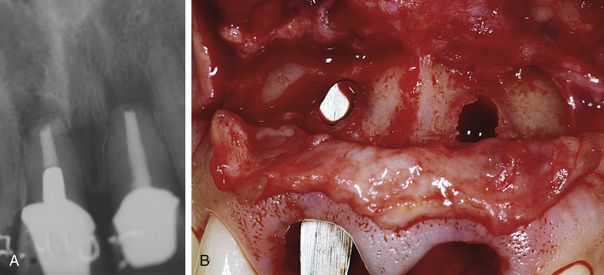
Fig 7.6 (A) Tooth adjacent to the future implant site showing deep periodontal pocket with purulent discharge through a sinus. The infected pocket is treated first with scaling, curettage and antibiotics until it healed and showed no active infection. (B and C) The healed periodontal osseous defect is exposed, cleaned, irrigated with antibiotics and grafted simultaneous to implant placement at the adjacent site.
Opposing and adjacent teeth at occlusal position
The teeth adjacent to and opposing the edentulous site should be examined for any supra eruption inclinations, mesial drifting, etc. for prosthetically guided implant insertion (
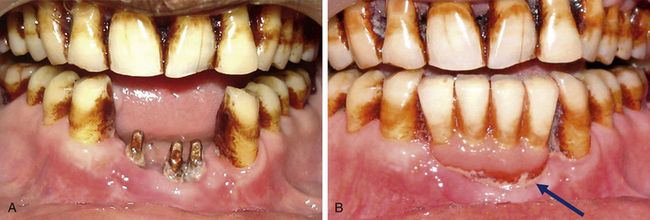
Oral hygiene of the patient
Oral hygiene maintenance is mandatory to avoid any infection to the inserted implants and also for their long-term survival. Advanced periodontitis should be treated before implant therapy. Scaling and root planing should always be done before implant insertion. Preoperative oral rinses with a 0.12% chlorhexidine digluconate solution has been shown to significantly lower the incidence of postimplantation infectious complications. A preoperative 30-s rinse is recommended, followed by twice daily rinses for 2 weeks following surgery.
Tobacco chewing
Tobacco chewing is often associated with poor oral hygiene and periodontal problems in the remaining teeth. Oral prophylaxis should be done before performing implant therapy and the patient should be encouraged to avoid tobacco chewing and adopt oral hygiene maintenance before placement of implants. Tobacco chewing also causes peri-implantitis in the restored implants; hence the patient should be instructed to avoid tobacco chewing for long-term survival of the implants (
Bruxism
The problem of bruxism should be treated before placing implants, to avoid post loading problems, such as the early wearing of the prosthesis, ceramic fractures, component fractures, crestal bone resorption, etc. (
History of diseased or lost teeth
The history of tooth loss can be very informative to evaluate the bony tissue present at the planned implant site. The traumatic loss of a tooth often leads to the fracture of the thin facial cortical plate. Either reduced buccolingual bone dimensions or a large osseous defect can be found in such cases, when the bony ridge is exposed for implant insertion (
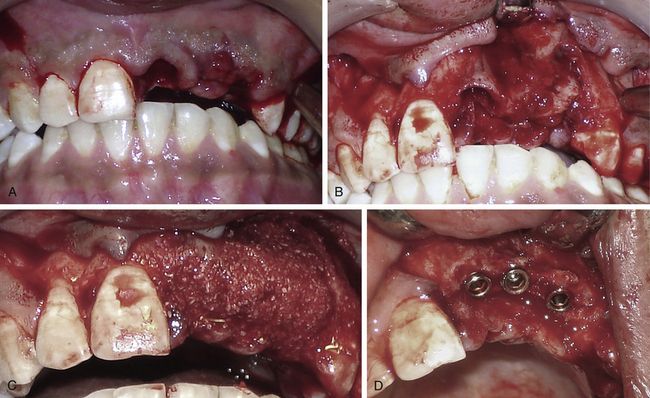
Fig 7.10 (A and B) The traumatic loss of teeth often results in loss of thin facial cortical plate. (C and D) The area should be grafted using bone regeneration material and implant inserted in the new bone dimensions after 4 months.
Mouth opening
This is one of the most neglected points when the implant surgeon plans for the implant therapy in the posterior region of the mouth. Often, patients with submucous fibrosis or TMJ problems, show limited mouth opening, which can cause problems with osteotomy preparation or other adjuvant procedures like sinus grafting.
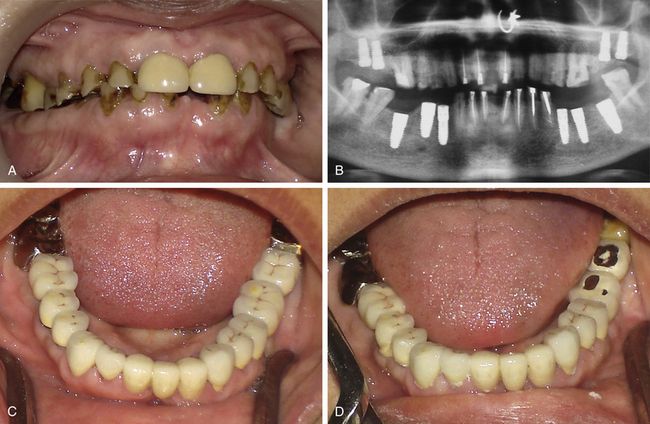
Diagnostic (panoramic/periapical) radiographs
Panoramic and periapical radiographs are very useful diagnostic tools to evaluate the edentulous bony ridge and its surrounding structures. These radiographs give ideas about any root remnant, mesiodistal dimensions of the edentulous space, bone height available to insert implant, any root curvature of adjacent teeth, any bone defect, any periodontal or periapical lesion with the adjacent teeth and the position and route of vital structures in the area, like mental foramina, mandibular canal, maxillary sinus floor, nasal floor, etc. However, when the dentist is planning implant therapy, he/she should always keep in mind that the panoramic radiograph may show 10–30% magnification of hard tissue structures. Whereas, depending on the cone angulation of the radiographic machine, the periapical radiographs show variable amounts of magnification. When planning with these radiographs, a radiographic template with the small metal balls placed above the ridge crest, should be used to calibrate image magnification. If the panoramic radiograph of the patient shows bone dimensions that are more than required, the implant surgeon, to be on the safer side, may plan for the ideal implant size by reducing the radiographic dimensions by 25%. For example, if the panoramic radiograph shows 20 mm bone height above the mandibular canal, it should be reduced by 25% (maximum possible magnification percentage); thus the actual bone height may be 15 mm. Further, leaving 3 mm bone above the canal as a safety guard to avoid nerve injury, the dentist should place only 12 mm long implants. For tight edentulous spaces and limited bone height the bone dimensions can be exactly calibrated using the small metal balls in the radiographic template (e.g. if the metal ball with actual diameter 3 mm is used and shows 4 mm diameter in the radiograph, that means the radiograph is showing 25% magnification). Other disadvantages of these radiographs are that they do not give any idea about bone width and bone density.
Impressions and diagnostic cast preparation
Impression of both the arches should be made using alginate impression material and bite registration should be recorded using an appropriate bite material. Upper and lower diagnostic casts must be articulated in occlusion (for partially edentulous patients) or in centric relation (for completely edentulous patients). These diagnostic casts are used:
a. To evaluate the patient’s opposing tooth/teeth, their overeruption, buccal or lingual inclinations, the drifting of adjacent teeth, ridge form, etc.
b. To fabricate a radiographic template (using radiograph or CT scan), which is used for accurate planning of the implant
c. To fabricate the surgical stent for accurate implant placement
d. For the fabrication of an interim prosthesis after implant insertion.
Clinical pictures of the edentulous area
a. The pre-clinical situation of the case
c. The width of keratinized soft tissue collar at the implant site
d. The periodontal health of the adjacent teeth
All these features, which are recorded along with clinical pictures, can be very helpful for treatment planning, as the implant dentist can correlate the hard tissue (bone) situations, which are recorded with the radiographs and CT scan, with the type and amount of soft tissue recorded with the clinical pictures.
Bone mapping
Bone mapping is done to evaluate the buccolingual bone dimensions at the edentulous site, which cannot be recorded with the radiograph. There are different ways of doing bone mapping but the easiest way is using a bone calliper. A surface anaesthetic or a small amount of local infiltration is given at the implant site and the bone calliper tips are pierced through the buccal and lingual soft tissue to reach the underlying bone. The bone calliper shows the reading on its scale. This procedure can be repeated at 2 to 3 points along the ridge height to evaluate the bone width at different points along the bony ridge (
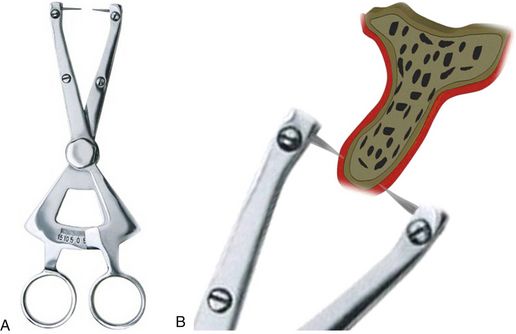
Fig 7.13 (A) Bone mapping calliper (Salvin Dental Specialities, USA). (B) Surface anaesthetic is applied at the site and the buccolingual bone dimensions at different points along the ridge height is measured using the bone calliper. Its sharp and pointed pins punch through the soft tissue to reach the underlying bone and its scale shows the ridge width present at the particular edentulous ridge site.
Radiographic template fabrication
An ideal provisional prosthesis is fabricated for the edentulous site by setting the teeth in position and in correct occlusion with the opposing dentition or prosthesis. Either radiopaque teeth are used in the template or a radiopaque material like gutta-percha or self-cure resin mixed with radiopaque barium sulphate is filled in the template at the prosthetically accurate, desired implant sites. This template is accurately seated in the patient’s mouth and the patient is sent for the dental radiographs and/or dental CT scan. The radiopaque teeth or the radiopaque material filled at the implant site is clearly visible in the dental radiograph or dental CT scan. With reference to these radiopaque sites, which represent the ideal implant positions and three-dimensional orientations for the accurate future prosthesis, the implants with ideal dimensions, positions, and angulations are planned, executed, and placed accurately for the future prosthesis (‘prosthetically guided implant insertion’).
Template for radiograph
As described earlier in this chapter, radiographs show some degree of magnification; thus the template with calibrated metal balls should be used in radiographic planning of the implant case, to exactly calculate the percentage of magnification in the radiographic image (
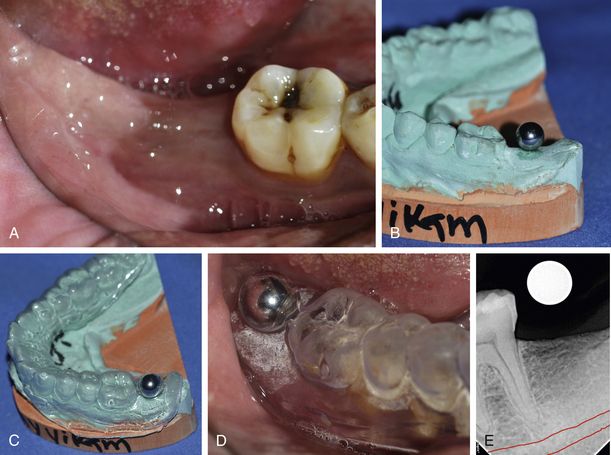
Fig 7.14 (A) Clinical view of missing mandibular second molar. An impression is made and a diagnostic cast is prepared. (B) A metal ball is fixed at the planned implant site on the diagnostic cast, using a glue and (C) a vacuum form tray is adapted over the same. (D) The vacuum form tray carrying the metal ball is seated in the patient’s mouth and (E) a radiograph is taken which shows the metal ball as the round white image. Now the diameter of real ball and its white image in radiograph is measured and calibrated to calculate the exact magnification that the radiograph shows. For example, if the diameter of the real ball is 3 mm and its radiographic image shows 4 mm, there is 25% magnification in the radiograph. Thus if the radiograph is showing 16 mm available bone height from crest to mandibular canal for the implant placement, the actual bone height could be only 12 mm (25% less than the radiographic bone height); therefore, the maximum length of the implant that can be inserted is 10 mm (leaving 2 mm as the safety margin from the mandibular canal).
Template for dental CT
Using the metal ball in the CT scan template results in the scattering of CT images. Moreover, the dental CT scan does not show any magnification, so ball calibration is also not required; hence any non–metallic, radiopaque material like gutta-percha or self-cure acrylic mixed with barium sulphate can be used in the template to evaluate and plan the desired edentulous ridge sites for three-dimensionally accurate implant placements (
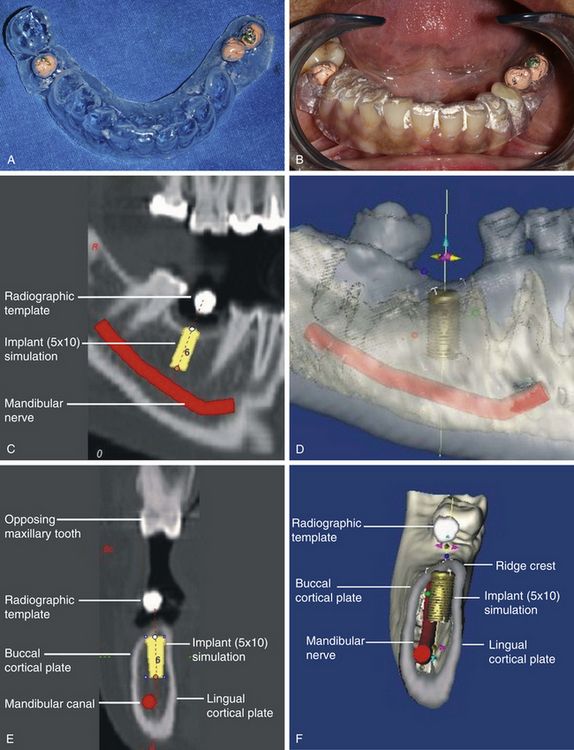
Fig 7.15 (A) The vacuum form tray is fabricated over the gutta-percha placed on the top of the ridge of the diagnostic cast. (B) The patient is sent for the dental CT scan with the vacuum form tray seated in the mouth. (C–F) The gutta-percha balls can be seen in the CT images as a white opaque image, and they are used as the reference point to plan the dimensions and angulation of the implant for the prosthesis.
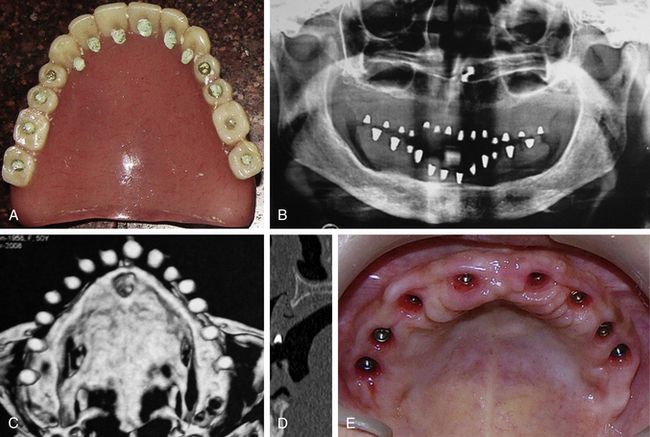
Fig 7.16 (A) Patient’s denture teeth are drilled at the ideal implant sites and holes filled with the heated gutta-percha. The patient is sent for radiograph and dental CT scan with the denture in the mouth. (B) The panoramic radiograph, and (C and D) 3D and cross-sectional views of the dental CT scan show the radiopaque GP points. (E) The implants are inserted at the desired site which shows the adequate bone dimensions and are also ideal for the implant prosthesis.
Radiographic implant template from the implant system
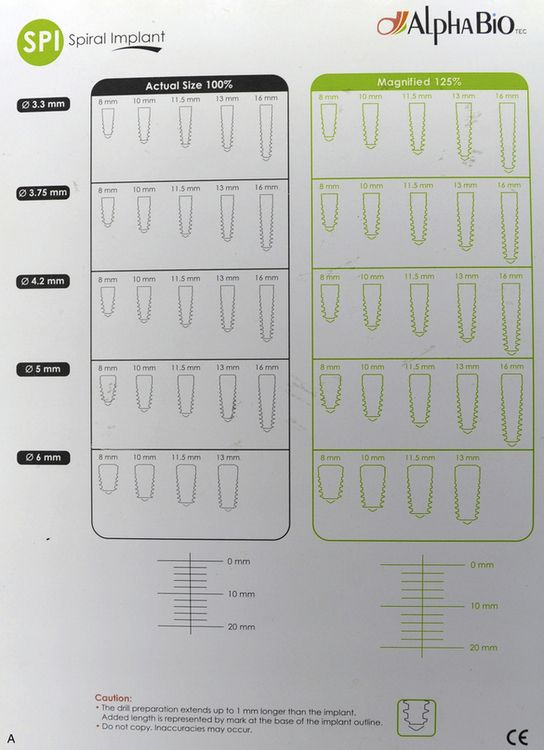
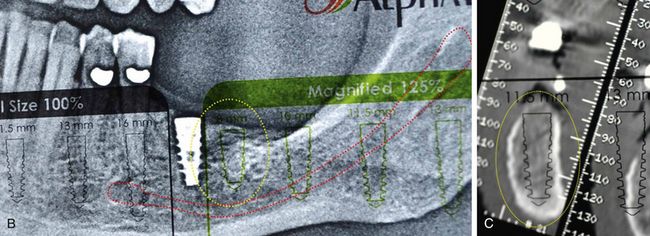
A few implant systems provide a radiographic template in the form of a transparent sheet showing the actual size images (100%) of all their implants as well as magnified implant images (125%). In planning with the patient’s radiograph, the magnified implant image of the template is used to make ideal implant selections for a particular site. However, if the implant surgeon is planning with the dental CT scan which shows no magnification, he/she should use the actual size implant image of the radiographic template for the planning (
Fig 7.17 (A) The radiographic template sheath of the SPI implant showing actual sizes (100%) of the implants (black images) as well as magnified images (125%) of the same implants (green images).
(B) When planning with the panoramic radiograph the green coloured magnified image is used for the planning (C) but if planning with the CT scan the black coloured actual size implant image is used for the same.
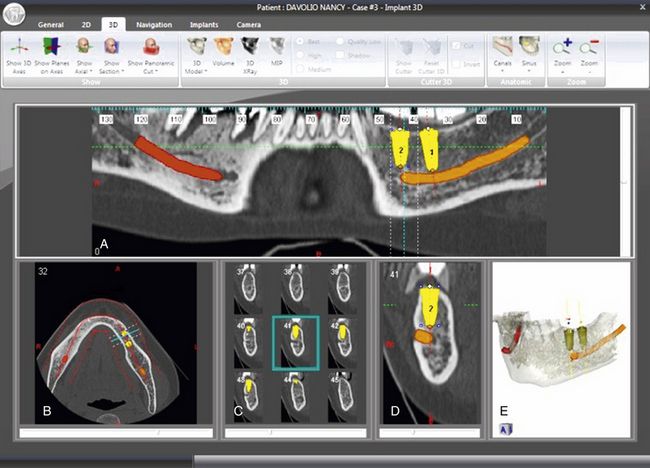
CT planning
With advancements in diagnostic tools, many implant dentists now prefer to evaluate bone quality and measure three-dimensional ridge dimensions accurately with the help of the dental CT scan (Dentascan). Some implant simulation softwares (Nobel Guide, Implant 3D, etc.) are also available in the market, which can create beautiful axial, panoramic, cross-sections and three-dimensional views of the jawbone using the raw dental CT files (
a. Accurate three-dimensional measurement of available bone (buccolingual, mesiodistal, and bone height)
b. Bone density at the implant site
e. Any osseous defect, if present
f. Three-dimensional view of the complete jawbone
g. Three-dimensional paths and architecture of vital structures like the mandibular canal, nasal cavity and its floor, sinus cavity and its floor, etc.
h. Implant simulation for accurate implant selection and its three-dimensional placement orientation for the best possible future prosthesis
i. Volume of the graft required, if any grafting procedure like sinus grafting, block grafting, etc. needs to be performed.
Surgical guide fabrication
As previously mentioned, implant insertion should be guided by the planned future prosthesis. Thus the use of the surgical guide is paramount for the ideal implant insertion. Depending on the technique, there are different ways to fabricate the surgical guide.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses