Fig 5.1 Lekhom and Zarb classification of jawbone qualities – (A) quality 1 bone, (B) quality 2 bone, (C) quality 3 bone and (D) quality 4 bone.
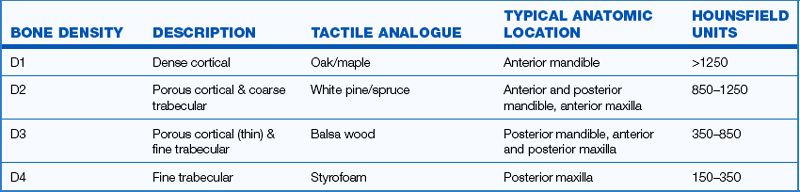
Misch bone density classification
Carl E Misch defined four bone density types found in all regions of the jaw. The trabecular and cortical parts of these bone types differ at the macroscopic level (< ?xml:namespace prefix = "mbp" />
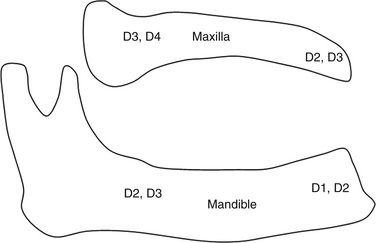
1. The anterior maxilla region (second premolar to second premolar), usually has D3 bone, but in few cases it may have D2 bone quality.
2. The posterior maxilla region (molar region) usually has D4 bone but in cases of sinus grafting it may have D3 bone 6 months after grafting.
3. The anterior mandible region (first premolar to first premolar) usually has D2 bone, but the resorbed anterior mandible may have D1 bone quality in approximately 25% of cases, more commonly in males.
4. The posterior mandible region (second premolar and molars) usually has D3 bone, but in some cases it can have D2 bone quality.

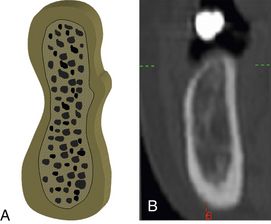
Fig 5.3 Diagrammatic presentation of the four bone density types described by Carl E Misch. (A) D1 bone is dense cortical bone and is the highest in the density, (B) D2 bone is coarse trabecular bone surrounded by thick porous cortical bone, (C) D3 bone is fine trabecular bone surrounded by thin porous cortical bone, and (D) D4 bone is fine trabecular bone with almost no cortical bone.
Determination of bone density
1. Computed tomography (CT) scan. Radiographs give a very limited idea of bone density, but with the help of the dental CT scan (DentaScan), the surgeon can ascertain bone density at the edentulous site before placing the implant. The dental CT scan is frequently used by the implant surgeon in treatment planning, as it gives all the details like three-dimensional bone volume, bone density, any defect present at the site, accurate implant simulation for the best possible prosthesis, etc. well before the actual implant surgery. Bone density is measured in the CT scan in Hounsfield unit (HU), i.e., denser bones have more Hounsfield units (
2. Tactile determination during bone drilling. As bone density is directly related to bone strength, bone density at the site for implant insertion can be determined by the tactile sensation felt by an experienced implant surgeon during pilot drilling in the bone at the time of osteotomy preparation. Higher speed and more pressure are needed to do pilot drilling in bone with high density. Osteotomy-widening drilling does not give as good an idea of bone density as pilot drilling at the time of osteotomy preparation, because less rigorous drilling is required to widen the osteotomy already prepared by the initial pilot drill.
D1/Type 1 bone (dense cortical bone)
This homogenous compact bone contains almost no trabecular bone. Being dense cortical, it is the hardest bone in the jaw showing the least amount of vascularity. Because of limited blood supply, this bone shows very poor bone regeneration capacity. Osteotomy should be prepared at higher speed and using a new drill, under maximum flow of chilled saline irrigation to reduce heat generation and bone necrosis. This bone type is most commonly found in the mandibular anterior region (
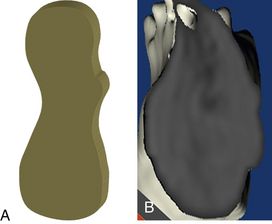
Fig 5.4 Dense cortical or homogenous compact D1 bone, (A) diagrammatic presentation and as seen in (B) 3D cross-section of a dental CT.
Advantages
1. Strongest bone in the mouth
2. Implant achieves highest primary stability
3. Implant achieves higher bone–implant surface contact (BIC) percentage
4. Fewer implants can be inserted to support a multiple unit prosthesis
5. Requires only 3 – 4 months for primary healing of implants (osseointegration)
6. One-stage non-submerged surgical protocol can be practised in most cases
7. Immediate loading protocol can be practised in selective cases
Disadvantages
1. Least amount of vascularity
2. Slow lamellar bone formation
3. Chances of bone overheating during osteotomy preparation are very high and may lead to osteonecrosis
4. Highest rate of failure in implant surgery
5. Longest time taken for implant placement
6. Requires drilling at high speed (2500 rpm) using new drills
7. Requires tapping (thread forming) for implants with non-cutting threads
8. May require crestal bone modification/drilling for the implant with broader platform than the implant body, to reduce incidence of mechanical overload during its insertion at crest.
D2/Type 2 bone
(Porous thick cortical and coarse trabecular) – This bone shows a thick layer of compact bone surrounding a core of dense trabecular bone (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses